Persistent Detection and Infectious Potential of SARS-CoV-2 Virus in Clinical Specimens from COVID-19 Patients
Abstract
:1. Introduction
2. SARS-CoV-2 Entry and Replication
3. Duration of SARS-CoV-2 RT-PCR Positivity and Factors Associated with Prolonged Clinical Shedding
4. Persistent Detection of SARS-CoV-2 in Feces
5. Persistent Detection of SARS-CoV-2 in Other Bodily Fluids
6. Infectious Potential of Clinically Shed SARS-CoV-2
7. Infectivity of SARS-CoV-2 Shed by Pre-Symptomatic and Asymptomatic Infected Individuals
8. SARS-CoV-2 Clinical Shedding by Children
9. Persistent Clinical Shedding, Relapse, and Reinfection
10. Discussion
Funding
Acknowledgments
Conflicts of Interest
References
- Anthony, S.J.; Johnson, C.K.; Greig, D.J.; Kramer, S.; Che, X.; Wells, H.; Hicks, A.L.; Joly, D.O.; Wolfe, N.D.; Daszak, P.; et al. PREDICT Consortium, Mazet JAK, Goldstein T. Virus Evol. 2017, 3, vex012. [Google Scholar] [PubMed]
- Cui, J.; Li, F.; Shi, Z.-L. Origin and evolution of pathogenic coronaviruses. Nat. Rev. Genet. 2019, 17, 181–192. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zhang, S.-F.; Tuo, J.-L.; Huang, X.-B.; Zhu, X.; Zhang, D.-M.; Zhou, K.; Yuan, L.; Luo, H.-J.; Zheng, B.-J.; Yuen, K.-Y.; et al. Epidemiology characteristics of human coronaviruses in patients with respiratory infection symptoms and phylogenetic analysis of HCoV-OC43 during 2010–2015 in Guangzhou. PLoS ONE 2018, 13, e0191789. [Google Scholar] [CrossRef] [PubMed]
- Vennema, H.; De Groot, R.J.; A Harbour, D.; Dalderup, M.; Gruffydd-Jones, T.; Horzinek, M.C.; Spaan, W.J. Early death after feline infectious peritonitis virus challenge due to recombinant vaccinia virus immunization. J. Virol. 1990, 64, 1407–1409. [Google Scholar] [CrossRef] [Green Version]
- She, J.; Jiang, J.; Ye, L.; Hu, L.; Bai, C.; Song, Y. 2019 novel coronavirus of pneumonia in Wuhan, China: Emerging attack and management strategies. Clin. Transl. Med. 2020, 9, 19. [Google Scholar] [CrossRef]
- Guan, W.J.; Ni, Z.-Y.; Hu, Y.; Liang, W.-H.; Ou, C.-Q.; He, J.-X.; Liu, L.; Shan, H.; Lei, C.-L.; Hui, D.; et al. For the China Medical Treatment Expert Group for Covid-19. Clinical Characteristics of Coronavirus Disease 2019 in China. N. Engl. J. Med. 2020, 382, 1708–1720. [Google Scholar] [CrossRef]
- Xu, X.; Chen, P.; Wang, J.; Feng, J.; Zhou, H.; Li, X.; Zhong, W.; Hao, P. Evolution of the novel coronavirus from the ongoing Wuhan outbreak and modeling of its spike protein for risk of human transmission. Sci. China Life Sci. 2020, 63, 457–460. [Google Scholar] [CrossRef] [Green Version]
- Jaimes, J.A.; André, N.M.; Chappie, J.S.; Millet, J.K.; Whittaker, G.R. Phylogenetic Analysis and Structural Modeling of SARS-CoV-2 Spike Protein Reveals an Evolutionary Distinct and Proteolytically Sensitive Activation Loop. J. Mol. Biol. 2020, 432, 3309–3325. [Google Scholar] [CrossRef]
- Gorbalenya, A.E.; Baker, S.C.; Baric, R.S.; de Groot, R.J.; Drosten, C.; Haagmans, B.L.; Neuman, B.W.; Perlman, S.; Poon, L.L.M.; Gulyaeva, A.A.; et al. The species Severe acute respiratory syndrome-related coronavirus: Classifying 2019-nCoV and naming it SARS-CoV-2. Nat. Microbiol. 2020, 5, 536–544. [Google Scholar] [CrossRef] [Green Version]
- WHO Statement on Novel Coronavirus in Thailand. Available online: https://www.who.int/news-room/detail/13-01-2020-who-statement-on-novel-coronavirus-in-thailand (accessed on 31 July 2020).
- WHO Statement on Novel Coronavirus—Japan (Ex-China). Available online: https://www.who.int/csr/don/16-january-2020-novel-coronavirus-japan-ex-china/en/ (accessed on 31 July 2020).
- WHO Director-General’s Statement on IHR Emergency Committee on Novel Coronavirus (2019-nCoV). Available online: https://www.who.int/dg/speeches/detail/who-director-general-s-statement-on-ihr-emergency-committee-on-novel-coronavirus-(2019-ncov) (accessed on 31 July 2020).
- WHO Media Briefing on #COVID19 with @DrTedros. Available online: https://twitter.com/WHO/status/1237777021742338049?ref_src=twsrc%5Etfw%7Ctwcamp%5Etweetembed%7Ctwterm%5E1237777021742338049&ref_url=https%3A%2F%2Fwww.who.int%2Femergencies%2Fdiseases%2Fnovel-coronavirus-2019%2Fevents-as-they-happen (accessed on 31 July 2020).
- COVID-19 Dashboard by the Center for Systems Science and Engineering (CSSE) at Johns Hopkins University. Available online: https://0-coronavirus-jhu-edu.brum.beds.ac.uk/map.html (accessed on 24 November 2020).
- Worldometer: COVID-19 Coronavirus Pandemic. Available online: https://www.worldometers.info/coronavirus/#countries (accessed on 23 November 2020).
- Wang, D.; Hu, B.; Hu, C.; Zhu, F.; Liu, X.; Zhang, J.; Wang, B.; Xiang, H.; Cheng, Z.; Xiong, Y.; et al. Clinical Characteristics of 138 Hospitalized Patients With 2019 Novel Coronavirus-Infected Pneumonia in Wuhan, China. JAMA 2020, 323, 1061. [Google Scholar] [CrossRef]
- Becker, R.C. COVID-19 update: Covid-19-associated coagulopathy. J. Thromb. Thrombolysis 2020, 50, 54–67. [Google Scholar] [CrossRef] [PubMed]
- Shi, S.; Qin, M.; Shen, B.; Cai, Y.; Liu, T.; Yang, F.; Gong, W.; Liu, X.; Liang, J.; Zhao, Q.; et al. Association of Cardiac Injury with Mortality in Hospitalized Patients With COVID-19 in Wuhan, China. JAMA Cardiol. 2020, 5, 802. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Raza, A.; Estepa, A.; Chan, V.; Jafar, M.S. Acute Renal Failure in Critically Ill COVID-19 Patients with a Focus on the Role of Renal Replacement Therapy: A Review of What We Know So Far. Cureus 2020, 12, e8429. [Google Scholar] [CrossRef] [PubMed]
- Kennedy, M.; Helfand, B.K.I.; Gou, R.Y.; Gartaganis, S.L.; Webb, M.; Moccia, J.M.; Bruursema, S.N.; Dokic, B.; McCulloch, B.; Ring, H.; et al. Delirium in Older Patients With COVID-19 Presenting to the Emergency Department. JAMA Netw. Open 2020, 3, e2029540. [Google Scholar] [CrossRef]
- Cozzi, D.; Albanesi, M.; Cavigli, E.; Moroni, C.; Bindi, A.; Luvarà, S.; Lucarini, S.; Busoni, S.; Mazzoni, L.N.; Miele, V. Chest X-ray in new Coronavirus Disease 2019 (COVID-19) infection: Findings and correlation with clinical outcome. La Radiol. Med. 2020, 125, 730–737. [Google Scholar] [CrossRef]
- Pourbagheri-Sigaroodi, A.; Bashash, D.; Fateh, F.; Abolghasemi, H. Laboratory findings in COVID-19 diagnosis and prognosis. Clin. Chim. Acta 2020, 510, 475–482. [Google Scholar] [CrossRef]
- Li, Q.; Zheng, X.-S.; Shen, X.-R.; Si, H.-R.; Wang, X.; Wang, Q.; Li, B.; Zhang, W.; Zhu, Y.; Jiang, R.-D.; et al. Prolonged shedding of severe acute respiratory syndrome coronavirus 2 in patients with COVID-19. Emerg. Microbes Infect. 2020, 1–28. [Google Scholar] [CrossRef]
- Khailany, R.A.; Safdar, M.; Ozaslan, M. Genomic characterization of a novel SARS-CoV-2. Gene Rep. 2020, 19, 100682. [Google Scholar] [CrossRef]
- Aronson, J.K. Coronaviruses—A General Introduction; Centre for Evidence-Based Medicine, Nuffield Department of Primary Care Health Sciences, University of Oxford: Oxford, UK, 2020. [Google Scholar]
- Kabbani, N.; Olds, J.L. Does COVID19 Infect the Brain? If So, Smokers Might Be at a Higher Risk. Mol. Pharmacol. 2020, 97, 351–353. [Google Scholar] [CrossRef]
- Kumar, S.; Nyodu, R.; Maurya, V.K.; Saxena, S.K. Morphology, Genome Organization, Replication, and Pathogenesis of Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2). In Medical Virology: From Pathogenesis to Disease Control; Saxena, S., Ed.; Springer: Singapore, 2020. [Google Scholar]
- Cheng, P.K.C.; Wong, D.; Tong, L.K.L.; Ip, S.-M.; Lo, A.C.T.; Lau, C.-S.; Yeung, E.Y.H.; Lim, W.W.L. Viral shedding patterns of coronavirus in patients with probable severe acute respiratory syndrome. Lancet 2004, 363, 1699–1700. [Google Scholar] [CrossRef] [Green Version]
- Oh, M.-D.; Park, W.B.; Choe, P.G.; Choi, S.-J.; Kim, J.-I.; Chae, J.; Park, S.S.; Kim, E.-C.; Oh, H.S.; Kim, E.J.; et al. Viral Load Kinetics of MERS Coronavirus Infection. N. Engl. J. Med. 2016, 375, 1303–1305. [Google Scholar] [CrossRef] [PubMed]
- Zou, L.; Ruan, F.; Huang, M.; Liang, L.; Huang, H.; Hong, Z.; Yu, J.; Kang, M.; Song, Y.; Xia, J.; et al. SARS-CoV-2 Viral Load in Upper Respiratory Specimens of Infected Patients. N. Engl. J. Med. 2020, 382, 1177–1179. [Google Scholar] [CrossRef] [PubMed]
- Young, B.E.; Ong, S.W.X.; Kalimuddin, S.; Low, J.G.; Tan, S.Y.; Loh, J.; Ng, O.-T.; Marimuthu, K.; Ang, L.W.; Mark, T.M.; et al. Epidemiologic Features and Clinical Course of Patients Infected With SARS-CoV-2 in Singapore. JAMA 2020, 323, 1488–1494. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zhou, F.; Yu, T.; Du, R.; Fan, G.; Liu, Y.; Liu, Z.; Xiang, J.; Wang, Y.; Song, B.; Gu, X.; et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: A retrospective cohort study. Lancet 2020, 395, 1054–1062. [Google Scholar] [CrossRef]
- Zhou, B.; She, J.; Wang, Y.; Ma, X. Duration of Viral Shedding of Discharged Patients with Severe COVID-19. Clin. Infect. Dis. 2020, 71, 2240–2242. [Google Scholar] [CrossRef]
- Zheng, S.; Fan, J.; Yu, F.; Feng, B.; Lou, B.; Zou, Q.; Xie, G.; Lin, S.; Wang, R.; Yang, X.; et al. Viral load dynamics and disease severity in patients infected with SARS-CoV-2 in Zhejiang province, China, January-March 2020: Retrospective cohort study. BMJ 2020, 369, m1443. [Google Scholar] [CrossRef] [Green Version]
- Fang, Z.; Zhang, Y.; Hang, C.; Ai, J.-W.; Li, S.; Zhang, W. Comparisons of viral shedding time of SARS-CoV-2 of different samples in ICU and non-ICU patients. J. Infect. 2020, 81, 147–178. [Google Scholar] [CrossRef]
- Liu, Y.; Yan, L.-M.; Wan, L.; Xiang, T.-X.; Le, A.; Liu, J.-M.; Peiris, M.; Poon, L.L.; Zhang, W. Viral dynamics in mild and severe cases of COVID-19. Lancet Infect. Dis. 2020, 20, 656–657. [Google Scholar] [CrossRef] [Green Version]
- To, K.K.-W.; Tsang, O.T.-Y.; Leung, W.-S.; Tam, A.R.; Wu, T.-C.; Lung, D.C.; Yip, C.C.-Y.; Cai, J.-P.; Chan, J.M.-C.; Chik, T.S.-H.; et al. Temporal profiles of viral load in posterior oropharyngeal saliva samples and serum antibody responses during infection by SARS-CoV-2: An observational cohort study. Lancet Infect. Dis. 2020, 20, 565–574. [Google Scholar] [CrossRef] [Green Version]
- Long, Q.; Tang, X.-J.; Shi, Q.-L.; Li, Q.; Deng, H.-J.; Yuan, J.; Hu, J.-L.; Xu, W.; Zhang, Y.; Lv, F.-J.; et al. Clinical and immunological assessment of asymptomatic SARS-CoV-2 infections. Nat. Med. 2020, 26, 1200–1204. [Google Scholar] [CrossRef]
- Li, T.-Z.; Cao, Z.-H.; Chen, Y.; Cai, M.-T.; Zhang, L.-Y.; Xu, H.; Zhang, J.-Y.; Ma, C.-H.; Liu, Y.; Gao, L.-J.; et al. Duration of SARS-CoV-2 RNA shedding and factors associated with prolonged viral shedding in patients with COVID-19. J. Med. Virol. 2020, 10. [Google Scholar] [CrossRef] [PubMed]
- Xiao, A.T.; Tong, Y.X.; Zhang, S. Profile of RT-PCR for SARS-CoV-2: A Preliminary Study From 56 COVID-19 Patients. Clin. Infect. Dis. 2020. [Google Scholar] [CrossRef] [PubMed]
- Xu, K.; Chen, Y.; Yuan, J.; Yi, P.; Ding, C.; Wu, W.; Li, Y.; Ni, Q.; Zou, R.; Li, X.; et al. Factors Associated with Prolonged Viral RNA Shedding in Patients with Coronavirus Disease 2019 (COVID-19). Clin. Infect. Dis. 2020, 71, 799–806. [Google Scholar] [CrossRef] [PubMed]
- Mönkemüller, K.; Fry, L.; Rickes, S. Covid-19, Coronavirus, SARS-CoV-2 and the small bowel. Rev. Española Enferm. Dig. 2020. [Google Scholar] [CrossRef]
- Wrapp, D.; Wang, N.; Corbett, K.S.; Goldsmith, J.A.; Hsieh, C.-L.; Abiona, O.; Graham, B.S.; McLellan, J.S. Cryo-EM structure of the 2019-nCoV spike in the prefusion conformation. Science 2020, 367, 1260–1263. [Google Scholar] [CrossRef] [Green Version]
- Leung, W.K.; To, K.-F.; Chan, P.K.; Chan, H.L.; Wu, A.K.; Lee, N.; Yuen, K.Y.; Sung, J.J. Enteric involvement of severe acute respiratory syndrome-associated coronavirus infection. Gastroenterology 2003, 125, 1011–1017. [Google Scholar] [CrossRef] [Green Version]
- Song, Y.; Liu, P.; Shi, X.L.; Chu, Y.L.; Zhang, J.; Xia, J.; Gao, X.Z.; Qu, T.; Wang, M.Y. SARS-CoV-2 induced diarrhea as onset symptom in patient with COVID-19. Gut 2020, 69, 1143–1144. [Google Scholar] [CrossRef] [Green Version]
- Morone, G.; Palomba, A.; Iosa, M.; Caporaso, T.; De Angelis, D.; Venturiero, V.; Savo, A.; Coiro, P.; Carbone, D.; Gimigliano, F.; et al. Incidence and Persistence of Viral Shedding in COVID-19 Post-acute Patients with Negativized Pharyngeal Swab: A Systematic Review. Front. Med. 2020, 7. [Google Scholar] [CrossRef]
- Van Doorn, A.S.; Meijer, B.; Frampton, C.M.A.; Barclay, M.L.; De Boer, N.K.H. Systematic review with meta-analysis: SARS-CoV-2 stool testing and the potential for faecal-oral transmission. Aliment. Pharmacol. Ther. 2020. [Google Scholar] [CrossRef]
- Jones, D.L.; Baluja, M.Q.; Graham, D.W.; Corbishley, A.; McDonald, J.E.; Malham, S.K.; Hillary, L.S.; Connor, T.R.; Gaze, W.H.; Moura, I.B.; et al. Shedding of SARS-CoV-2 in feces and urine and its potential role in person-to-person transmission and the environment-based spread of COVID-19. Sci. Total. Environ. 2020, 749, 141364. [Google Scholar] [CrossRef]
- Guerrero-Latorre, L.; Ballesteros, I.; Villacrés-Granda, I.; Granda, M.G.; Freire-Paspuel, B.; Ríos-Touma, B. SARS-CoV-2 in river water: Implications in low sanitation countries. Sci. Total. Environ. 2020, 743, 140832. [Google Scholar] [CrossRef] [PubMed]
- Randazzo, W.; Truchado, P.; Cuevas-Ferrando, E.; Simón, P.; Allende, A.; Sánchez, G. SARS-CoV-2 RNA in wastewater anticipated COVID-19 occurrence in a low prevalence area. Water Res. 2020, 181, 115942. [Google Scholar] [CrossRef] [PubMed]
- Xu, C.L.H.; Raval, M.; Schnall, J.A.; Kwong, J.C.; Holmes, N.E. Duration of Respiratory and Gastrointestinal Viral Shedding in Children With SARS-CoV-2: A Systematic Review and Synthesis of Data. Pediatr. Infect. Dis. J. 2020, 39, e249–e256. [Google Scholar] [CrossRef] [PubMed]
- Santos, V.S.; Gurgel, R.Q.; Cuevas, L.E.; Martins-Filho, P.R. Prolonged Fecal Shedding of SARS-CoV-2 in Pediatric Patients: A Quantitative Evidence Synthesis. J. Pediatr. Gastroenterol. Nutr. 2020, 71, 150–152. [Google Scholar] [CrossRef]
- Xing, Y.-H.; Ni, W.; Wu, Q.; Li, W.-J.; Li, G.-J.; Wang, W.-D.; Tong, J.-N.; Song, X.-F.; Wong, G.; Xing, Q. Prolonged viral shedding in feces of pediatric patients with coronavirus disease 2019. J. Microbiol. Immunol. Infect. 2020, 53, 473–480. [Google Scholar] [CrossRef]
- To, K.F.; Tong, J.H.M.; Chan, P.K.S.; Au, F.W.L.; Chim, S.S.C.; Chan, K.C.A.; Cheung, J.L.K.; Liu, E.Y.M.; Tse, G.M.K.; Lo, A.W.I.; et al. Tissue and cellular tropism of the coronavirus associated with severe acute respiratory syndrome: An in-situ hybridization study of fatal cases. J. Pathol. 2004, 202, 157–163. [Google Scholar] [CrossRef]
- Zhou, J.; Chu, H.; Chan, J.F.-W.; Yuen, K.-Y. Middle East respiratory syndrome coronavirus infection: Virus-host cell interactions and implications on pathogenesis. Virol. J. 2015, 12, 218. [Google Scholar] [CrossRef] [Green Version]
- Yang, X.; Yu, Y.; Xu, J.; Shu, H.; Xia, J.; Liu, H.; Wu, Y.; Zhang, L.; Yu, Z.; Fang, M.; et al. Clinical course and outcomes of critically ill patients with SARS-CoV-2 pneumonia in Wuhan, China: A single-centered, retrospective, observational study. Lancet Respir. Med. 2020, 8, 475–481. [Google Scholar] [CrossRef] [Green Version]
- Chen, T.; Wu, D.; Chen, H.; Yan, W.; Yang, D.; Chen, G.; Ma, K.; Xu, D.; Yu, H.; Wang, H.; et al. Clinical characteristics of 113 deceased patients with coronavirus disease 2019: Retrospective study. BMJ 2020, 368. [Google Scholar] [CrossRef] [Green Version]
- Naicker, S.; Yang, C.-W.; Hwang, S.-J.; Liu, B.-C.; Chen, J.-H.; Jha, V. The Novel Coronavirus 2019 epidemic and kidneys. Kidney Int. 2020, 97, 824–828. [Google Scholar] [CrossRef]
- Roshandel, M.R.; Nateqi, M.; Lak, R.; Aavani, P.; Sari Motlagh, R.; Shariat, S.F.; Aghaei Badr, T.; Sfakianos, J.; Kaplan, S.A.; Tewari, A.K. Diagnostic and methodological evaluation of studies on the urinary shedding of SARS-CoV-2, compared to stool and serum: A systematic review and meta-analysis. Cell Mol. Biol. 2020, 66, 148–156. [Google Scholar] [CrossRef] [PubMed]
- Xu, D.; Zhang, Z.; Jin, L.; Chu, F.; Mao, Y.; Wang, H.; Liu, M.; Wang, M.; Zhang, L.; Gao, G.F.; et al. Persistent shedding of viable SARS-CoV in urine and stool of SARS patients during the convalescent phase. Eur. J. Clin. Microbiol. Infect. Dis. 2005, 24, 165–171. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wang, J.-X.; Li, Y.-Y.; Liu, X.-D.; Cao, X. Virus transmission from urinals. Phys. Fluids 2020, 32, 081703. [Google Scholar] [CrossRef] [PubMed]
- Massarotti, C.; Garolla, A.; Maccarini, E.; Scaruffi, P.; Stigliani, S.; Anserini, P.; Foresta, C. SARS-CoV-2 in the semen: Where does it come from? Andrology 2020. [Google Scholar] [CrossRef] [PubMed]
- Li, X.; Chan, J.F.-W.; Li, K.K.-W.; Tso, E.Y.-K.; Yip, C.C.-Y.; Sridhar, S.; Chung, T.W.-H.; Chiu, K.H.-Y.; Hung, D.L.-L.; Wu, A.K.-L.; et al. Detection of SARS-CoV-2 in conjunctival secretions from patients without ocular symptoms. Infection 2020, 1–9. [Google Scholar] [CrossRef]
- Kaya, H.; Çalışkan, A.; Okul, M.; Sarı, T.; Akbudak, İ.H. Detection of SARS-CoV-2 in the tears and conjunctival secretions of Coronavirus disease 2019 patients. J. Infect. Dev. Ctries. 2020, 14, 977–981. [Google Scholar] [CrossRef]
- Han, D.; Fang, Q.; Wang, X. SARS-CoV-2 was found in the bile juice from a patient with severe COVID-19. J. Med. Virol. 2020. [Google Scholar] [CrossRef]
- Laferl, H.; Kelani, H.; Seitz, T.; Holzer, B.; Zimpernik, I.; Steinrigl, A.; Schmoll, F.; Wenisch, C.; Allerberger, F. An approach to lifting self-isolation for health care workers with prolonged shedding of SARS-CoV-2 RNA. Infection 2020, 6, 1–7. [Google Scholar] [CrossRef]
- Sohn, Y.; Jeong, S.J.; Chung, W.S.; Hyun, J.H.; Baek, Y.J.; Cho, Y.; Kim, J.H.; Ahn, J.Y.; Choi, J.Y.; Yeom, J.S. Assessing Viral Shedding and Infectivity of Asymptomatic or Mildly Symptomatic Patients with COVID-19 in a Later Phase. J. Clin. Med. 2020, 9, 2924. [Google Scholar] [CrossRef]
- Singanayagam, A.; Patel, M.; Charlett, A.; Lopez Bernal, J.; Saliba, V.; Ellis, J.; Ladhani, S.; Zambon, M.; Gopal, R. Duration of infectiousness and correlation with RT-PCR cycle threshold values in cases of COVID-19, England, January to May 2020. Eurosurveillance 2020, 25. [Google Scholar] [CrossRef]
- Jeong, H.W.; Kim, S.M.; Kim, H.S.; Kim, Y.I.; Kim, J.H.; Cho, J.Y.; Kim, S.H.; Kang, H.; Kim, S.G.; Park, S.J.; et al. Viable SARS-CoV-2 in various specimens from COVID-19 patients. Clin. Microbiol. Infect. 2020. [Google Scholar] [CrossRef] [PubMed]
- CDC Guidance for Discontinuation of Transmission-Based Precautions and Disposition of Patients with COVID-19 in Healthcare Settings (Interim Guidance). Available online: https://www.cdc.gov/coronavirus/2019-ncov/hcp/disposition-hospitalized-patients.html (accessed on 20 October 2020).
- Available online: https://www.sciencenews.org/article/coronavirus-covid-19-who-asymptomatic-cases-spread (accessed on 20 October 2020).
- He, X.; Lau, E.H.; Wu, P.; Deng, X.; Wang, J.; Hao, X.; Lau, Y.C.; Wong, J.Y.; Guan, Y.; Tan, X.; et al. Temporal dynamics in viral shedding and transmissibility of COVID-19. Nat. Med. 2020, 26, 672–675. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Arons, M.M.; Hatfield, K.M.; Reddy, S.C.; Kimball, A.; James, A.; Jacobs, J.R.; Taylor, J.; Spicer, K.; Bardossy, A.C.; Oakley, L.P.; et al. Presymptomatic SARS-CoV-2 Infections and Transmission in a Skilled Nursing Facility. N. Engl. J. Med. 2020, 382, 2081–2090. [Google Scholar] [CrossRef] [PubMed]
- Gandhi, M.; Yokoe, D.S.; Havlir, D.V. Asymptomatic Transmission, the Achilles’ Heel of Current Strategies to Control Covid-19. N. Engl. J. Med. 2020, 382, 2158–2160. [Google Scholar] [CrossRef]
- Oran, D.P.; Topol, E.J. Prevalence of Asymptomatic SARS-CoV-2 Infection. Ann. Intern. Med. 2020, 173, 362–367. [Google Scholar] [CrossRef]
- Bahar, B.; Jacquot, C.; Mo, Y.D.; DeBiasi, R.L.; Campos, J.; Delaney, M. Kinetics of Viral Clearance and Antibody Production Across Age Groups in Children with Severe Acute Respiratory Syndrome Coronavirus 2 Infection. J. Pediatr. 2020, 227, 31–37.e1. [Google Scholar] [CrossRef]
- Liu, P.; Cai, J.; Jia, R.; Xia, S.; Wang, X.; Cao, L.; Zeng, M.; Xu, J. Dynamic surveillance of SARS-CoV-2 shedding and neutralizing antibody in children with COVID-19. Emerg. Microbes Infect. 2020, 9, 1254–1258. [Google Scholar] [CrossRef]
- De Ioris, M.; Scarselli, A.; Degli Atti, M.L.C.; Ravà, L.; Smarrazzo, A.; Concato, C.; Romani, L.; Scrocca, R.; Geremia, C.; Carletti, M.; et al. Dynamic Viral Severe Acute Respiratory Syndrome Coronavirus 2 RNA Shedding in Children: Preliminary Data and Clinical Consideration from a Italian Regional Center. J. Pediatr. Infect. Dis. Soc. 2020, 9, 366–369. [Google Scholar] [CrossRef]
- Lu, Y.; Li, Y.; Deng, W.; Liu, M.; He, Y.; Huang, L.; Lv, M.; Li, J.; Du, H. Symptomatic Infection is Associated with Prolonged Duration of Viral Shedding in Mild Coronavirus Disease 2019. Pediatr. Infect. Dis. J. 2020, 39, e95–e99. [Google Scholar] [CrossRef]
- Lopez, A.S.; Hill, M.; Antezano, J.; Vilven, D.; Rutner, T.; Bogdanow, L.; Claflin, C.; Kracalik, I.T.; Fields, V.L.; Dunn, A.; et al. Transmission Dynamics of COVID-19 Outbreaks Associated with Child Care Facilities—Salt Lake City, Utah, April–July 2020. MMWR Morb. Mortal. Wkly. Rep. 2020, 69, 1319–1323. [Google Scholar] [CrossRef]
- Merckx, J.; Labrecque, J.A.; Kaufman, J.S. Transmission of SARS-CoV-2 by Children. Dtsch. Arztebl. Int. 2020, 117, 553–560. [Google Scholar] [CrossRef] [PubMed]
- Zhu, Y.; Bloxham, C.J.; Hulme, K.D.; Sinclair, J.E.; Tong, Z.W.M.; Steele, L.E.; Noye, E.C.; Lu, J.; Chew, K.Y.; Pickering, J.; et al. Children are unlikely to have been the primary source of household SARS-CoV-2 infections. Lancet 2020. [Google Scholar] [CrossRef]
- Posfay-Barbe, K.M.; Wagner, N.; Gauthey, M.; Moussaoui, D.; Loevy, N.; Diana, A.; L’Huillier, A.G. COVID-19 in Children and the Dynamics of Infection in Families. Pediatrics 2020, 146, e20201576. [Google Scholar] [CrossRef] [PubMed]
- Macartney, K.; E Quinn, H.; Pillsbury, A.J.; Koirala, A.; Deng, L.; Winkler, N.; Katelaris, A.L.; O’Sullivan, M.V.N.; Dalton, C.; Wood, N.; et al. Transmission of SARS-CoV-2 in Australian educational settings: A prospective cohort study. Lancet Child Adolesc. Health 2020, 4, 807–816. [Google Scholar] [CrossRef]
- Hildenwall, H.; Luthander, J.; Rhedin, S.; Hertting, O.; Olsson-Åkefeldt, S.; Melén, E.; Alfvén, T.; Herlenius, E.; Rinder, M.R. Paediatric COVID-19 admissions in a region with open schools during the two first months of the pandemic. Acta Paediatr. 2020. [Google Scholar] [CrossRef] [PubMed]
- Viner, R.M.; Russell, S.J.; Croker, H.; Packer, J.; Ward, J.; Stansfield, C.; Mytton, O.; Bonell, C.; Booy, R. School closure and management practices during coronavirus outbreaks including COVID-19: A rapid systematic review. Lancet Child Adolesc Health 2020, 4, 397–404. [Google Scholar] [CrossRef]
- Davies, N.G.; Klepac, P.; Liu, Y.; Prem, K.; Jit, M.; CMMID COVID-19 working group; Eggo, R.M. Age-dependent effects in the transmission and control of COVID-19 epidemics. Nat. Med. 2020, 26, 1205–1211. [Google Scholar] [CrossRef]
- Education: From Disruption to Recovery. Available online: https://en.unesco.org/covid19/educationresponse (accessed on 25 November 2020).
- Kang, H.; Wang, Y.; Tong, Z.; Liu, X. Retest positive for SARS-CoV-2 RNA of “recovered” patients with COVID-19: Persistence, sampling issues, or re-infection? J. Med. Virol. 2020, 92, 2263–2265. [Google Scholar] [CrossRef]
- Duggan, N.M.; Ludy, S.M.; Shannon, B.C.; Reisner, A.T.; Wilcox, S.R. Is novel coronavirus 2019 reinfection possible? Interpreting dynamic SARS-CoV-2 test results through a case report [published online ahead of print, 2020 Jul 4]. Am. J. Emerg. Med. 2020. [Google Scholar] [CrossRef]
- Lafaie, L.; Célarier, T.; Goethals, L.; Pozzetto, B.; Grange, S.; Ojardias, E.; Annweiler, C.; Botelho-Nevers, E. Recurrence or Relapse of COVID-19 in Older Patients: A Description of Three Cases. J. Am. Geriatr. Soc. 2020, 68, 2179–2183. [Google Scholar] [CrossRef]
- Torres, D.D.A.; Ribeiro, L.D.C.B.; Riello, A.P.D.F.L.; Horovitz, D.D.G.; Pinto, L.F.R.; Croda, J. Reinfection of COVID-19 after 3 months with a distinct and more aggressive clinical presentation: Case report. J. Med. Virol. 2020. [Google Scholar] [CrossRef] [PubMed]
- Lan, L.; Xu, D.; Ye, G.; Xia, C.; Wang, S.; Li, Y.; Xu, H. Positive RT-PCR Test Results in Patients Recovered From COVID-19. JAMA 2020, 323, 1502–1503. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tillett, R.L.; Sevinsky, J.R.; Hartley, P.D.; Kerwin, H.; Crawford, N.; Gorzalski, A.; Laverdure, C.; Verma, S.C.; Rossetto, C.C.; Jackson, D.; et al. Genomic evidence for reinfection with SARS-CoV-2: A case study. Lancet Infect. Dis. 2020. [Google Scholar] [CrossRef]
- Goldman, J.D.; Wang, K.; Roltgen, K.; Nielsen, S.C.A.; Roach, J.C.; Naccache, S.N.; Yang, F.; Wirz, O.F.; Yost, K.E.; Lee, J.Y.; et al. Reinfection with SARS-CoV-2 and Failure of Humoral Immunity: A case report. medRxiv 2020. [Google Scholar] [CrossRef]
- To, K.K.-W.; Hung, I.F.-N.; Ip, J.D.; Chu, A.W.-H.; Chan, W.-M.; Tam, A.R.; Fong, C.H.-Y.; Yuan, S.; Tsoi, H.-W.; Ng, A.C.-K.; et al. Coronavirus Disease 2019 (COVID-19) Re-infection by a Phylogenetically Distinct Severe Acute Respiratory Syndrome Coronavirus 2 Strain Confirmed by Whole Genome Sequencing. Clin. Infect. Dis. 2020. [Google Scholar] [CrossRef]
- Lu, J.; Peng, J.; Xiong, Q.; Liu, Z.; Lin, H.; Tan, X.; Kang, M.; Yuan, R.; Zeng, L.; Zhou, P.; et al. Clinical, immunological and virological characterization of COVID-19 patients that test re-positive for SARS-CoV-2 by RT-PCR. EBioMedicine 2020, 59. [Google Scholar] [CrossRef]
- York, A. Can COVID-19 strike twice? Nat. Rev. Genet. 2020, 18, 477. [Google Scholar] [CrossRef]
- Elrashdy, F.; AlJaddawi, A.A.; Redwan, E.M.; Uversky, V.N. On the potential role of exosomes in the COVID-19 reinfection/reactivation opportunity. J. Biomol. Struct. Dyn. 2020, 1–12. [Google Scholar] [CrossRef]
- Urbanelli, L.; Buratta, S.; Tancini, B.; Sagini, K.; Delo, F.; Porcellati, S.; Emiliani, C. The Role of Extracellular Vesicles in Viral Infection and Transmission. Vaccines 2019, 7, 102. [Google Scholar] [CrossRef] [Green Version]
- Lancman, G.; Mascarenhas, J.; Bar-Natan, M. Severe COVID-19 virus reactivation following treatment for B cell acute lymphoblastic leukemia. J. Hematol. Oncol. 2020, 13, 1–3. [Google Scholar] [CrossRef]
- Koirala, A.; Joo, Y.J.; Khatami, A.; Chiu, C.; Britton, P.N. Vaccines for COVID-19: The current state of play. Paediatr. Respir. Rev. 2020, 35, 43–49. [Google Scholar] [CrossRef] [PubMed]
- Cevik, M.; Tate, M.; Lloyd, O.; Maraolo, A.E.; Schafers, J.; Ho, A. SARS-CoV-2, SARS-CoV, and MERS-CoV viral load dynamics, duration of viral shedding, and infectiousness: A systematic review and meta-analysis. Lancet Microbe 2020. [Google Scholar] [CrossRef]
- Corman, V.M.; Albarrak, A.M.; Omrani, A.S.; Albarrak, M.M.; Farah, M.E.; Almasri, M.; Muth, D.; Sieberg, A.; Meyer, B.; Assiri, A.M.; et al. Viral Shedding and Antibody Response in 37 Patients with Middle East Respiratory Syndrome Coronavirus Infection. Clin. Infect. Dis. 2015, 62. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wölfel, R.; Corman, V.M.; Guggemos, W.; Seilmaier, M.; Zange, S.; Müller, M.A.; Niemeyer, D.; Jones, T.C.; Vollmar, P.; Rothe, C.; et al. Virological assessment of hospitalized patients with COVID-2019. Nature 2020, 581, 465–469. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Van Kampen, J.J.A.; van de Vijver, D.A.M.C.; Fraaij, P.L.A.; Haagmans, B.L.; Lamers, M.M.; Okba, N.; van den Akker, J.P.C.; Endeman, H.; Gommers, D.A.M.P.J.; Cornelissen, J.J.; et al. Shedding of infectious virus in hospitalized patients with coronavirus disease-2019 (COVID-19): Duration and key determinants. medRxiv 2020. [Google Scholar] [CrossRef]
- CDC Guidance for Duration of Isolation and Precautions for Adults with COVID-19. Available online: https://www.cdc.gov/coronavirus/2019-ncov/hcp/duration-isolation.html?CDC_AA_refVal=https%3A%2F%2Fwww.cdc.gov%2Fcoronavirus%2F2019-ncov%2Fcommunity%2Fstrategy-discontinue-isolation.html (accessed on 25 November 2020).
- Hua, C.Z.; Miao, Z.P.; Zheng, J.S.; Huang, Q.; Sun, Q.F.; Lu, H.P.; Su, F.F.; Wang, W.H.; Huang, L.P.; Chen, D.Q.; et al. Epidemiological features and viral shedding in children with SARS-CoV-2 infection. J. Med. Virol. 2020. [Google Scholar] [CrossRef]
- U.S. News and World Report: Mass Nationwide School Closures Loom as Coronavirus Cases Spike. Available online: https://www.usnews.com/news/education-news/articles/2020-11-17/mass-nationwide-school-closures-loom-as-coronavirus-cases-spike (accessed on 23 November 2020).
- CDC Guidance for Operating Schools during COVID-19: CDC’s Considerations. Available online: https://www.cdc.gov/coronavirus/2019-ncov/community/schools-childcare/reopening-schools.html (accessed on 25 November 2020).
- American Academy of Pediatrics COVID-19 Planning Considerations: Guidance for School Re-Entry. Available online: https://services.aap.org/en/pages/2019-novel-coronavirus-covid-19-infections/clinical-guidance/covid-19-planning-considerations-return-to-in-person-education-in-schools/ (accessed on 25 November 2020).
- Hepmag: Hepatitis C Treatment History Timeline. Available online: https://www.hepmag.com/blog/hepatitis-c-treatment-history-timeline (accessed on 4 November 2020).
- Verne, J. A Journey to the Centre of the Earth; Pierre-Jules Hetzel: Paris, France, 2006. [Google Scholar]

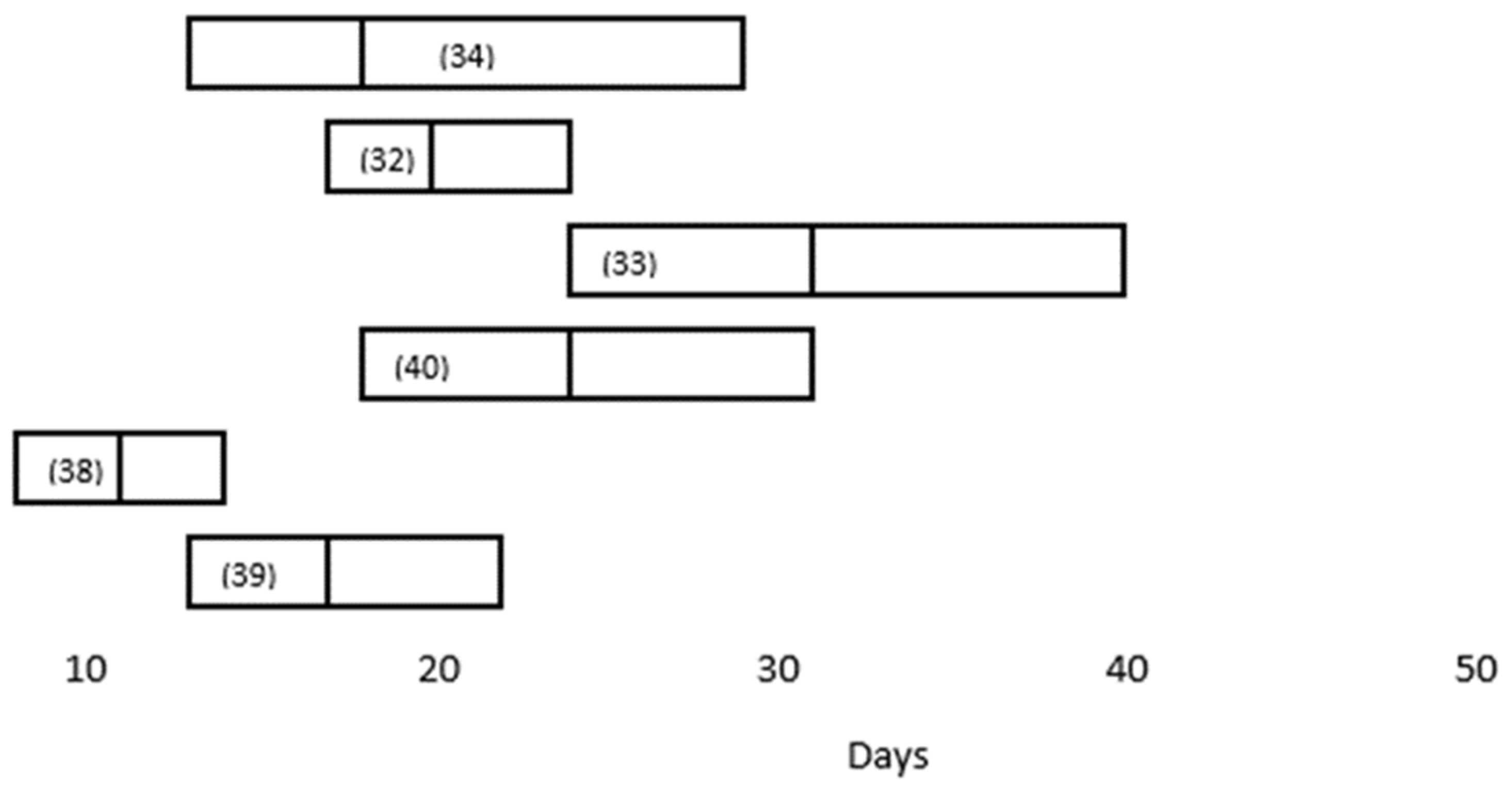

| Study (Reference) | Number Studied (N) | Median Duration in Respiratory Specimens (Days) | Independent Factors Associated with Viral Persistence |
|---|---|---|---|
| Zhou F, Yu T, Du R, et al. [32] | 191 | 20.0 days (IQR 17.0–24.0) | NE |
| Zhou B, She J, Wang Y, Ma X. [33] | 41 | 31 (IQR 24.0–40.0) | NE |
| Xiao AT, Tong YX, Zhang S. [40] | 56 | 24 (IQR, 18–31) | NE |
| Zheng S, Fan J, Yu F, et al. [34] | 96 | 18 (Range 13–29) | (1) severe disease (21 days, 14–30 days) |
| (2) age > 60 years | |||
| (3) male gender | |||
| Fang Z, Zhang Y, Hang C, Ai J, Li S, Zhang W. [35] | 32 | 22.25 ± 3.62 (ICU) vs. 15.67 ± 6.68 (non-ICU) | ICU hospitalization |
| Li TZ, Cao ZH, Chen Y, et al. [39]) | 101 | 11 (IQR 8–14.3) | (1) temperature > 38.5 °C) (OR 5.1, 95%CI: 1.5–18.1) |
| (2) corticosteroid use (OR 6.3, 95%CI: 1.5–27.8) | |||
| (3) time from onset to hospitalization (OR 1.8, 95%CI: 1.19–2.7) | |||
| Kaijin Xu, Yanfei Chen, Jing Yuan, et al. [41] | 113 | 17 (IQR, 13–22) | (1) male gender (OR, 3.24; 95% CI, 1.31–8.02) |
| (2) invasive mechanical ventilation (OR, 9.88; 95% CI, 1.11–88.02) | |||
| (3) time from illness onset to hospital admission (odds ratio [OR], 1.30; 95% confidence interval [CI], 1.10–1.54; p = 0.002) |
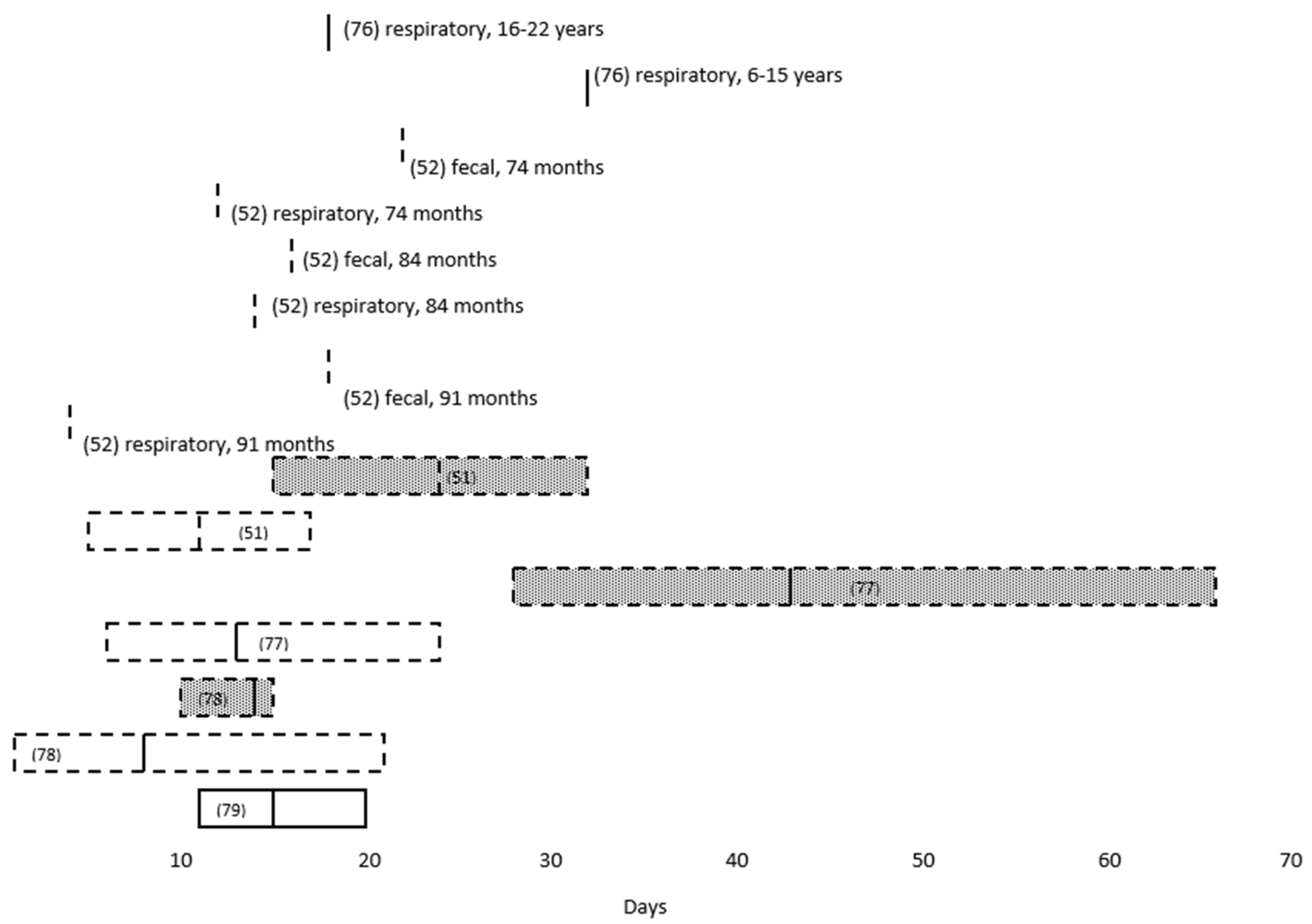
| Study (Reference) | Number Studied (N) | Median Age | Median Duration in Respiratory Specimens (Days) | Median Duration in Fecal Specimens (Days) | Median Time to Seropositivity (Days) |
|---|---|---|---|---|---|
| Bahar B, Jacquot C, Mo YD, et al. [76] | 6369 | 32 (ages 6–15 years) | NE | 18 (36 days for “adequate levels” of neutralizing antibodies) | |
| 18 (ages 16–22 years) | |||||
| Santos VS, Gurgel RQ, Cuevas LE, et al. [52] | 36 | 74 months (mean) | 12 (mean) | 22 (mean) | NE |
| 56 months (mean) | NE | NE | |||
| 84 months (mean) | 14.3 (mean) | 16.3 (mean) | |||
| 91 (mean) | 3.9 (mean) | 18.1 (mean) | |||
| Xu CLH, Raval M, Schnall JA, et al. [51] | 69 | 11.1 ± (mean) ± 5.8 | 23.6 ± (mean) ± 8.8 | NE | |
| Liu P, Cai J, Jia R, et al. [77] | 9 | 13 (range 6–24) | 43 (range 28–66) | 12.9 | |
| De Ioris MA, Scarselli A, Ciofi Degli Atti ML, et al. [78] | 22 | 84 months (range 8 days–210 months) | 8 (range 1–21) | 14 (range 10–15) | NE |
| Lu Y, Li Y, Deng W, et al. [79] | 110 | 6 years | 15 (IQR 11–20) | NE | NE |
| 11 (asymptomatic) | |||||
| 17 (symptomatic) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the author. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zapor, M. Persistent Detection and Infectious Potential of SARS-CoV-2 Virus in Clinical Specimens from COVID-19 Patients. Viruses 2020, 12, 1384. https://0-doi-org.brum.beds.ac.uk/10.3390/v12121384
Zapor M. Persistent Detection and Infectious Potential of SARS-CoV-2 Virus in Clinical Specimens from COVID-19 Patients. Viruses. 2020; 12(12):1384. https://0-doi-org.brum.beds.ac.uk/10.3390/v12121384
Chicago/Turabian StyleZapor, Michael. 2020. "Persistent Detection and Infectious Potential of SARS-CoV-2 Virus in Clinical Specimens from COVID-19 Patients" Viruses 12, no. 12: 1384. https://0-doi-org.brum.beds.ac.uk/10.3390/v12121384





