The Consequences of Delaying Telling Children with Perinatal HIV About Their Diagnosis as Perceived by Healthcare Workers in the Eastern Cape; A Qualitative Study
Abstract
:1. Introduction
2. Materials and Methods
2.1. Design of the Study
2.2. Data Collection
2.3. Data Analysis
2.4. Ethical Considerations
3. Results
3.1. Description of the Study Participants
3.2. Themes
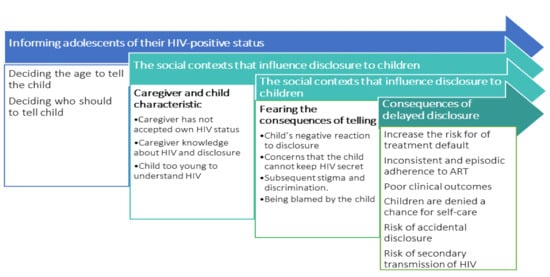
3.2.1. Informing Adolescents of their HIV-Positive Status.
Deciding the Age to Tell Children
“I don’t think there is a specific time or age that a child could be ready, but every time the healthcare worker meets the child, they should assess the maturity to determine readiness.” (FDG 4: Nurse).
“The important thing is to consider the age of the child…, check if the child is really matured to understand the disclosure.” (FGD 1; Lay counsellor).
“Personally, I think at least at the age of 10 years the child has some light and can understand better because this is when puberty starts.” (FGD 1: Social worker).
Deciding Who Should Tell the Child
“I say it is the parent..., parents know their children. I think disclosure is the right that should be given to the parent.” (FGD 1: Lay counsellor).
“The caregiver should initiate disclosure. The child trust the family more than the nurses at the clinic. Caregiver-initiated disclosure builds trust to the child and helps him/her to believe what the healthcare workers will tell her at the clinic.” (FGD 4: Nurse).
“The reluctance of parents to disclose to their children leaves us with no option but to disclose to the children ourselves.” (FGD 7: Nurse).
“Healthcare workers should disclose because they have more HIV-related information than the caregivers.” (FGD 1: Social worker).
I can say the healthcare worker because parents sometimes give false information, they don’t explain why or not give all information, they tell children that they will die if they don’t take treatment without the actual information” (FGD 1: Social worker).
“I intervened in children who defaulted because they were told false information, they were told that have heart disease. I provide ongoing counselling to support them and make appointments until adherence to treatment” (FGD 1: Dietician).
“I was exposed a lot to children who were not disclosed well or lied to by parents. Children were told that they are taking TB treatment and because they start to understand that TB treatment is six months they ask questions why are they still continuing to take such a treatment beyond the six months” (FGD 2: PN).
“I think the health worker can initiate disclosure but do it in the presence of the caregiver. During this process, both the caregiver and the health worker should talk, because the role of the health worker is to support the caregiver.” (FGD 7: Nurse).
“The caregiver and the health worker should work together during disclosure because it is the health worker who has more information relating to health matters, and is in a better position to explain what will happen if the treatment is not taken as prescribed.” (FGD 8: Nurse).
3.2.2. The Social Contexts That Influence Disclosure
Caregivers’ Acceptance of Thier Own HIV Status
“Sometimes parents do not disclose because they are scared that the child will tell other people about the HIV status, and by so doing reveal his/her status as well as that of the parent; while the parent was not ready for other people to know her HIV status.” (FGD 4; Nurse).
Caregiver’s Knowledge about HIV and Disclosure
“Parents are afraid that the child might ask questions about how they contracted HIV. So, parents are scared to be confronted by such questions from children.” (FGD 3: Lay counsellor).
“When the mother realises that she will not be able to answer questions about how the child became infected, she then avoids disclosing.” (FGD 8: Nurse).
“One parent approached me and told me that she wanted to disclose to her child but did not know how. This child started taking treatment when she was 9 years old and the mother came with her to me when she was 13 years old.” (FGD 1: Social worker).
Child too Young to Understand HIV
“Parents think that children are too young to understand, generally, they won’t understand hence they don’t disclose.” (FGD 5: Dietician).
“Parents do not disclose because they believe that the child is not yet matured enough to understand what is happening regarding HIV (FGD2; lay counsellor).
“Parents delay disclosing to their children and say that they are still waiting for child to be matured and ready in order to tell him/her about his/her HIV status (FFGD 6: PN)/
3.2.3. Fearing the Consequences of Telling
Child’s Negative Reaction to Disclosure
“They think disclosure will lead to children isolating themselves from other people because of the thought that they will die.” (FGD 5: Social worker).
“Sometimes the mother is scared that the child may commit suicide.” (FGD 4: Nurse).
“Other parents don’t disclose because they fear that they might lose their children, if the child discovers that she was infected through them.” (FGD 7: Nurse).
Concerns That the Child Cannot Keep HIV Secret
“The child might go and talk to other children; and the children will be not able to keep that secret because children don’t understand confidentiality.” (FGD 3: Lay counsellor, 34 years).
Subsequent Stigma and Discrimination
“The society looks at you with a different eye when you are HIV-positive. The lack of acceptance within homes and society drives those who are HIV-positive to live in constant denial of their condition.” (FGD 7: Nurse).
Being Blamed by the Child
“Parents feel responsible for passing the disease to the children. That’s why they don’t want to disclose.” (FGD 1: Dietitian).
“The other thing that causes the parent to fear, is the thinking that the child might hate her for the rest of his/her life, blaming her of infecting him/her.” (FGD 8: Nurse).
“I think the parent feels guilty and thinks that the child will blame her for carelessness and for failing to take measures to protect her/him from HIV infection. So, the parent is avoiding to be blamed and accused for the reason that the child is positive.” (FGD 6: Nurse).
3.2.4. Consequences of Delayed Disclosure
Contributes to Treatment Default
“Children get tired of taking treatment so they stop taking treatment if they don’t understand the reasons for taking it continuously.” (FGD 2: Nurse).
“I have an orphan teenage boy who started taking treatment at birth under the supervision of the grandfather, but when he entered adolescence, he stopped the treatment due to lack of knowledge about his status.” (FGD 4: Lay counsellor).
Poor Clinical Outcomes
“Deception about the nature of the disease for children leads to the decline of children’s health status as they become sick due to poor adherence. One child had to be changed to the second line of treatment.” (FGD 1: Dietician).
“I realised that unsuppressed viral loads among these children are due to non-adherence of treatment. They sometimes stop taking treatment since they don’t know why they are taking the treatment for.” (FGD 2: Nurse).
Inconsistent and Episodic Adherence to ART
“I have a case of two orphaned children aged 6 and 13 years old with high viral loads due to non-adherence to treatment. The grandmother explained that they are missing treatment because they come back home very late at night. These children don’t even know why they are taking treatment as no one ever told them about it.” (FGD 7: Nurse).
Children Are Denied a Chance for Self-Care
“Every time the young one takes her ARVs she also demanded that the older sibling should be given the treatment. She constantly asked why she was the only one taking the treatment. Whenever she fetched her treatment she also distributed to other children in the house and said that they must also drink.” (FGD 8; Nurse).
“I discovered during a home visit that he was throwing the tablets under the bed because he was sleeping alone.” (FGD 4: Lay counsellor).
Leads to Accidental Disclosure
“If the parent does not disclose, the child may discover his/her HIV status accidentally, which may cause denial for a very long time.” (FGD 3: Lay counsellor).
“Ooh! Just like what happened to me here. The child has been on ARVs for a very long time. I said to the child, ‘When you are HIV-positive you take this treatment’ and there…, the child started screaming. The child was just crying because he was on ARVs for so long without knowing that he is on HIV treatment. So accidents do happen.” (FGD 1: Nurse).
Risk of Secondary Transmission of HIV
“The disadvantage of non-disclosure during adolescence is that you may find the child has already started dating and practising unsafe sex.” (FGD 4: Nurse).
“Depending on their age, some of these children become sexually active at a very early age, for example at 11 or 12 years, so we do encourage them to use dual protection when engaging in sexual activities.” (FGD 7: Nurse).
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- John-Stewart, G.C.; Wariua, G.; Beima-Sofie, K.M.; Richardson, B.A.; Farquhar, C.; Maleche-Obimbo, E.; Mbori-Ngacha, D.; Wamalwa, D. Prevalence, perceptions, and correlates of pediatric HIV disclosure in an HIV treatment program in Kenya. AIDS Care 2013, 25, 1067–1076. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Vreeman, R.C.; Gramelspacher, A.M.; Gisore, P.O.; Scanlon, M.L.; Nyandiko, W.M. Disclosure of HIV status to children in resource-limited settings: A systematic review. J. Int. AIDS Soc. 2013, 16, 18466. [Google Scholar] [CrossRef] [PubMed]
- Vreeman, R.C.; Scanlon, M.L.; Mwangi, A.; Turissini, M.; Ayaya, S.O.; Tenge, C.; Nyandiko, W.M. A Cross-Sectional Study of Disclosure of HIV Status to Children and Adolescents in Western Kenya. PLoS ONE 2014, 9, e86616. [Google Scholar] [CrossRef] [PubMed]
- Beima-Sofie, K.M.; Brandt, L.; Hamunime, N.; Shepard, M.; Uusiku, J.; John-Stewart, G.C.; O’Malley, G. Pediatric HIV disclosure intervention improves knowledge and clinical outcomes in HIV-infected children in Namibia. J. Acquir. Immune Defic. Syndr. 2017, 75, 18. [Google Scholar] [CrossRef]
- Gyamfi, E.; Okyere, P.; Appiah-Brempong, E.; Adjei, R.O.; Mensah, K.A. Benefits of disclosure of HIV status to infected children and adolescents: Perceptions of caregivers and health care providers. J. Assoc. Nurses AIDS Care 2015, 26, 770–780. [Google Scholar] [CrossRef]
- Heeren, G.A.; Jemmott, J.B., III; Sidloyi, L.; Ngwane, Z.; Tyler, J.C. Disclosure of HIV diagnosis to HIV-infected children in South Africa: Focus groups for intervention development. Vulnerable Child. Youth Stud. 2012, 7, 47–54. [Google Scholar] [CrossRef] [Green Version]
- Lowenthal, E.D.; Jibril, H.B.; Sechele, M.L.; Mathuba, K.; Tshume, O.; Anabwani, G.M. Disclosure of HIV status to HIV-infected children in a large African treatment center: Lessons learned in Botswana. Child. Youth Serv. Rev. 2014, 45, 143–149. [Google Scholar] [CrossRef]
- Madiba, S.; Mokgatle, M. Health care workers’ perspectives about disclosure to HIV-infected children; cross-sectional survey of health facilities in Gauteng and Mpumalanga provinces, South Africa. PeerJ 2015, 3, e893. [Google Scholar] [CrossRef] [Green Version]
- Mutumba, M.; Musiime, V.; Tsai, A.C.; Byaruhanga, J.; Kiweewa, F.; Bauermeister, J.A.; Snow, R.C. Disclosure of HIV Status to Perinatally Infected Adolescents in Urban Uganda: A Qualitative Study on Timing, Process, and Outcomes. J. Assoc. Nurses AIDS Care 2015, 26, 472–484. [Google Scholar] [CrossRef]
- O’Malley, G.; Beima-Sofie, K.; Feris, L.; Shepard-Perry, M.; Hamunime, N.; John-Stewart, G.; Kaindjee-Tjituka, F.; Brandt, L. “If I Take My Medicine, I Will Be Strong:” Evaluation of a Pediatric HIV Disclosure Intervention in Namibia. J. Acquir. Immune Defic. Syndr. 2015, 68, e1–e7. [Google Scholar] [CrossRef]
- Dahourou, D.; Raynaud, J.-P.; Leroy, V. The challenges of timely and safe HIV disclosure among perinatally HIV-infected adolescents in sub-Saharan Africa. Curr. Opin. HIV AIDS 2018, 13, 220–229. [Google Scholar] [CrossRef] [PubMed]
- Britto, C.; Mehta, K.; Thomas, R.; Shet, A. Prevalence and correlates of HIV disclosure among children and adolescents in low-and middle-income countries: A systematic review. J. Dev. Behav. Pediat. JDBP 2016, 37, 496. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Doat, A.-R.; Negarandeh, R.; Hasanpour, M. Disclosure of HIV status to children in Sub-Saharan Africa: A systematic review. Medicina 2019, 55, 433. [Google Scholar] [CrossRef] [Green Version]
- World Health Organization. Guideline on HIV Disclosure Counselling for Children up to 12 Years of Age. World Health Organization. 2011. Available online: https://apps.who.int/iris/bitstream/handle/10665/44777/9789241502863_eng.pdf (accessed on 11 September 2020).
- Arrivé, E.; Dicko, F.; Amghar, H.; Aka, A.E.; Dior, H.; Bouah, B.; Traoré, M.; Ogbo, P.; Dago-Akribi, H.A.; Eboua, T.K.F. HIV status disclosure and retention in care in HIV-infected adolescents on antiretroviral therapy (ART) in West Africa. PLoS ONE 2012, 7, e33690. [Google Scholar] [CrossRef] [PubMed]
- Vaz, L.; Corneli, A.; Dulyx, J.; Rennie, S.; Omba, S.; Kitetele, F.; AD Research Group; Behets, F. The process of HIV status disclosure to HIV-positive youth in Kinshasa, Democratic Republic of the Congo. AIDS Care Psychol. Soc. Med. Asp. AIDS/HIV 2008, 20, 842–852. [Google Scholar] [CrossRef] [PubMed]
- Eneh, A.; Ugwu, R.; Paul, N. HIV Disclosure in Children in This Millenium—Should It still be an Issue? Adv. Res. 2019, 20, 1–11. [Google Scholar] [CrossRef]
- Gitahi, N.; Camlin, C.; Mwania, V.; Ngure, K.; Auerswald, C.; Bukusi, E. Psychosocial needs among older perinatally infected adolescents living with HIV and transitioning to adult care in Kenya. PLoS ONE 2020, 15, e0233451. [Google Scholar] [CrossRef]
- Brandt, L.; Beima-Sofie, K.; Hamunime, N.; Shepard, M.; Ferris, L.; Ingo, P.; John-Stewart, G.; O’Malley, G. Growing-up just like everyone else: Key components of a successful pediatric HIV disclosure intervention in Namibia. ACID 2015, 29 (Suppl. 1), S81–S89. [Google Scholar] [CrossRef] [Green Version]
- Kalembo, F.W.; Kendall, G.E.; Ali, M.; Chimwaza, A.F. Healthcare workers’ perspectives and practices regarding the disclosure of HIV status to children in Malawi: A cross-sectional study. BMC Health Serv. Res. 2018, 18, 540. [Google Scholar] [CrossRef]
- Madiba, S.; Mokwena, K. Caregivers’ Barriers to Disclosing the HIV Diagnosis to Infected Children on Antiretroviral Therapy in a Resource-Limited District in South Africa: A Grounded Theory Study. AIDS Res. Treat. 2012, 2012, 402403. [Google Scholar] [CrossRef] [Green Version]
- Mweemba, M.; Musheke, M.M.; Michelo, C.; Halwiindi, H.; Mweemba, O.; Zulu, J.M. “When am I going to stop taking the drug?” Enablers, barriers and processes of disclosure of HIV status by caregivers to adolescents in a rural district in Zambia. BMC Public Health 2015, 15, 1028. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gyamfi, E.; Okyere, P.; Enoch, A.; Appiah-Brempong, E. Prevalence of, and barriers to the disclosure of HIV status to infected children and adolescents in a district of Ghana. BMC Int. Health Hum. Rights 2017, 17, 1–8. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kiwanuka, J.; Mulogo, E.; Haberer, J.E. Caregiver Perceptions and Motivation for Disclosing or Concealing the Diagnosis of HIV Infection to Children Receiving HIV Care in Mbarara, Uganda: A Qualitative Study. PLoS ONE 2014, 9, e93276. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mburu, G.; Ram, M.; Oxenham, D.; Haamujompa, C.; Iorpenda, K.; Ferguson, L. Responding to adolescents living with HIV in Zambia: A social-ecological approach. Child. Youth Serv. Rev. 2014, 45, 9–17. [Google Scholar] [CrossRef] [Green Version]
- Atwiine, B.; Kiwanuka, J.; Musinguzi, N.; Atwine, D.; Haberer, J.E. Understanding the role of age in HIV disclosure rates and patterns for HIV-infected children in southwestern Uganda. AIDS Care 2015, 27, 424–430. [Google Scholar] [CrossRef] [PubMed]
- Madiba, S. Caregivers Lack of Disclosure Skills Delays Disclosure to Children with Perinatal HIV in Resource-Limited Communities: Multicenter Qualitative Data from South Africa and Botswana. Nurs. Res. Pract. 2016, 2016, 9637587. [Google Scholar] [CrossRef] [PubMed]
- Namukwaya, S.; Paparini, S.; Seeley, J.; Bernays, S. “How Do We start? and how Will They react?” Disclosing to Young People with Perinatally acquired hiV in Uganda. Front. Public Health 2017, 5, 343. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sariah, A.; Rugemalila, J.; Somba, M.; Minja, A.; Makuchilo, M.; Tarimo, E.; Urassa, D.; Siril, H. “Experiences with disclosure of HIV-positive status to the infected child”: Perspectives of healthcare providers in Dar es Salaam, Tanzania. BMC Public Health 2016, 16, 1083. [Google Scholar] [CrossRef] [Green Version]
- Beima-Sofie, K.; John-Stewart, G.; Shah, B.; Wamalwa, D.; Maleche-Obimbo, E.; Kelley, M. Using Health Provider Insights to Inform Pediatric HIV Disclosure: A Qualitative Study and Practice Framework from Kenya. AIDS Patient Care STDs 2014, 28, 555–564. [Google Scholar] [CrossRef] [Green Version]
- Watermeyer, J. ‘Are we allowed to disclose?’: A healthcare team’s experiences of talking with children and adolescents about their HIV status. Health Expect. 2015, 18, 590–600. [Google Scholar] [CrossRef] [Green Version]
- Santamaria, E.K.; Dolezal, C.; Marhefka, S.L.; Hoffman, S.; Ahmed, Y.; Elkington, K.; Mellins, C.A. Psychosocial implications of HIV serostatus disclosure to youth with perinatally acquired HIV. AIDS Patient Care STDs 2011, 25, 257–264. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mavhu, W.; Berwick, J.; Chirawu, P.; Makamba, M.; Copas, A.; Dirawo, J.; Willis, N.; Araya, R.; Abas, M.A.; Corbett, E.L.; et al. Enhancing psychosocial support for HIV positive adolescents in Harare, Zimbabwe. PLoS ONE 2013, 8, e70254. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Phuma-Ngaiyaye, E.E.; Dartey, A.F. Experiences of children living with HIV and AIDS following their diagnosis disclosure in Mzuzu, Malawi. Vulnerable Child. Youth Stud. 2015, 10, 357–365. [Google Scholar] [CrossRef]
- Kajubi, P.; Whyte, S.; Muhumuza, S.; Kyaddondo, D.; Katahoire, A.R. Communication between HIV-infected children and their caregivers about HIV medicines: A cross-sectional study in Jinja district, Uganda. J. Int. AIDS Soc. 2014, 17, 19012. [Google Scholar] [CrossRef] [PubMed]
- Braun, V.; Clarke, V. Using thematic analysis in psychology. Qual. Res. Psychol. 2006, 3, 77–101. [Google Scholar] [CrossRef] [Green Version]
- Nowell, L.S.; Norris, J.M.; White, D.E.; Moules, N.J. Thematic analysis: Striving to meet the trustworthiness criteria. Int. J. Qual. Methods 2017, 16. [Google Scholar] [CrossRef]
- Creswell, J.W. Qualitative Inquiry and Research Method: Choosing Among Five Approaches, 2nd ed.; Sage: Thousand Oaks, CA, USA, 2007. [Google Scholar]
- Anney, V.N. Ensuring the quality of the findings of qualitative research: Looking at trustworthiness criteria. J. Emerg. Trends Educ. Res. Policy Stud. 2014, 2, 272–281. [Google Scholar]
- Mumburi, L.P.; Hamel, B.C.; Philemon, R.N.; Kapanda, G.N.; Msuya, L.J. Factors associated with HIV-status disclosure to HIV-infected children receiving care at Kilimanjaro Christian Medical Centre in Moshi, Tanzania. Pan. Afr. Med. J. 2014, 18, 50. [Google Scholar] [CrossRef]
- Kidia, K.; Mupambireyi, Z.; Cluver, L.D.; Ndhlovu, C.E.; Borok, M.; Ferrand, R.A. HIV Status Disclosure to Perinatally-Infected Adolescents in Zimbabwe: A Qualitative Study of Adolescent and Healthcare Worker Perspectives. PLoS ONE 2014, 9, e87322. [Google Scholar] [CrossRef] [Green Version]
- Mandalazi, P.; Bandawe, C.; Umar, E. HIV Disclosure: Parental dilemma in informing HIV infected Children about their HIV Status in Malawi. Malawi Med. J. 2014, 26, 101–104. [Google Scholar]
- DeSilva, M.B.; Penwill, N.; Sabin, L.; Gifford, A.L.; Li, Z.; Fujie, Z.; Weiwei, M.; Yongzhen, L.; HongYan, L.; Xuemei, Z.; et al. We don’t dare to tell her … we don’t know where to begin: Disclosure experiences and challenges among adolescents living with HIV and their caregivers in China. Int. J. Pediatr. Adolesc. Med. 2018, 5, 5–12. [Google Scholar] [CrossRef] [PubMed]
- Rujumba, J.; Mbasaalaki-Mwaka, C.L.; Ndeezi, G. Challenges faced by health workers in providing counselling services to HIV-positive children in Uganda: A descriptive study. J. Int. AIDS Soc. 2010, 13, 9. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Vreeman, R.C.; Scanlon, M.L.; Inui, T.S.; McAteer, C.I.; Fischer, L.J.; McHenry, M.S.; Marete, I.; Nyandiko, W.M. ‘Why did you not tell me?’: Perspectives of caregivers and children on the social environment surrounding child HIV disclosure in Kenya. AIDS 2015, 29, S47–S55. [Google Scholar] [CrossRef] [PubMed]
- Wariri, O.; Ajani, A.; Raymond, M.P.; Iliya, A.; Lukman, O.; Okpo, E.A.; Isaac, E. “What will my child think of me if he hears I gave him HIV?”: A sequential, explanatory, mixed-methods approach on the predictors and experience of caregivers on disclosure of HIV status to infected children in Gombe, Northeast Nigeria. BMC Public Health 2020, 20, 373. [Google Scholar] [CrossRef] [Green Version]
- Kalembo, F.W.; Kendall, G.E.; Ali, M.; Chimwaza, A.F. Prevalence and factors associated with emotional and behavioural difficulties among children living with HIV in Malawi: A cross-sectional study. BMC Psychiatry 2019, 19, 60. [Google Scholar] [CrossRef] [Green Version]
- Mburu, G.; Hodgson, I.; Kalibala, S.; Haamujompa, C.; Cataldo, F.; Lowenthal, E.D.; Ross, D. Adolescent HIV disclosure in Zambia: Barriers, facilitators and outcomes. J. Int. AIDS Soc. 2014, 17, 18866. [Google Scholar] [CrossRef]
- Vaz, L.M.E.; Maman, S.; Eng, E.; Barbarin, O.A.; Tshikandu, T.; Behets, F. Patterns of Disclosure of HIV Status to Infected Children in a Sub-Saharan African Setting. J. Dev. Behav. Pediatr. 2011, 32, 307–315. [Google Scholar] [CrossRef] [Green Version]
- Madiba, S.; Josiah, U. Perceived Stigma and Fear of Unintended Disclosure are Barriers in Medication Adherence in Adolescents with Perinatal HIV in Botswana: A Qualitative Study. BioMed Res. Int. 2019, 2019, 9623159. [Google Scholar] [CrossRef] [Green Version]
- Okawa, S.; Mwanza-Kabaghe, S.; Mwiya, M.; Kikuchi, K.; Jimba, M.; Kankasa, C.; Ishikawa, N. Adolescents’ Experiences and Their Suggestions for HIV Serostatus Disclosure in Zambia: A Mixed-Methods Study. Front. Public Health 2017, 5, 326. [Google Scholar] [CrossRef]
- Mengesha, M.M.; Dessie, Y.; Roba, A.A. Perinatally acquired HIV-positive status disclosure and associated factors in Dire Dawa and Harar, Eastern Ethiopia: A health facility-based cross-sectional study. BMJ Open 2018, 8, e019554. [Google Scholar] [CrossRef] [Green Version]
| Variables | Characteristics | Frequency (%) |
|---|---|---|
| Sex | Female | 46 (90.2) |
| Male | 5 (9.8) | |
| Designations of HCWs | Lay counsellor | 16 (31.3) |
| Enrolled nursing assistant | 1 (1) | |
| Enrolled nurse | 2 (3.9) | |
| Professional nurse | 24 (47) | |
| Social worker | 5 (9.8) | |
| Dietician | 3 (5.9) | |
| Age group | 20–29 | 5 (9.8) |
| 30–39 | 15 (29.4) | |
| 40–49 | 16 (31.4) | |
| 50–59 | 14 (27.4) | |
| 60–69 | 1 (2) | |
| Paediatric HIV experience | <1 year | 4 (7.8) |
| 1–4 years | 11 (21.6) | |
| 5–10 years | 19 (37.3) | |
| >10 years | 17 (33.3) | |
| Ever disclosed HIV to a child? | Yes | 36 (70.6) |
| No | 15 (29.4) | |
| Ideal age of disclosure | 8–12 years | 40 (80) |
| <12 years | 2 (4) | |
| >8 years | 8 (16) | |
| HCW who have disclosed | Lay counsellor | 13 out of 16 |
| Enrolled nursing assistant | 0 out of 1 | |
| Enrolled nurse | 0 out of 2 | |
| Professional nurse | 19 out of 24 | |
| Social worker | 3 out of 5 | |
| Dietician | 1 out of 2 |
| Informing Children of Their HIV-Positive Status | Deciding the Age to Tell the Child |
| Deciding Who Should Tell the Child | |
| The social contexts that influence disclosure to children | Caregiver and child characteristic The caregiver has not accepted own HIV status Caregiver knowledge about HIV and disclosure Child too young to understand HIV |
| Fearing the consequences of telling Child’s negative reaction to disclosure Concerns that the child cannot keep HIV secret Subsequent stigma and discrimination Being blamed by the child | |
| Consequences of delayed disclosure | Contributes to treatment default Inconsistent and episodic adherence to ART Poor clinical outcomes Children are denied a chance for self-care Leads to accidental disclosure Risk of secondary transmission of HIV |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Madiba, S.; Diko, C. The Consequences of Delaying Telling Children with Perinatal HIV About Their Diagnosis as Perceived by Healthcare Workers in the Eastern Cape; A Qualitative Study. Children 2020, 7, 289. https://0-doi-org.brum.beds.ac.uk/10.3390/children7120289
Madiba S, Diko C. The Consequences of Delaying Telling Children with Perinatal HIV About Their Diagnosis as Perceived by Healthcare Workers in the Eastern Cape; A Qualitative Study. Children. 2020; 7(12):289. https://0-doi-org.brum.beds.ac.uk/10.3390/children7120289
Chicago/Turabian StyleMadiba, Sphiwe, and Cynthia Diko. 2020. "The Consequences of Delaying Telling Children with Perinatal HIV About Their Diagnosis as Perceived by Healthcare Workers in the Eastern Cape; A Qualitative Study" Children 7, no. 12: 289. https://0-doi-org.brum.beds.ac.uk/10.3390/children7120289