Detection of Early Warning Signs in Autism Spectrum Disorders: A Systematic Review
Abstract
:1. Introduction
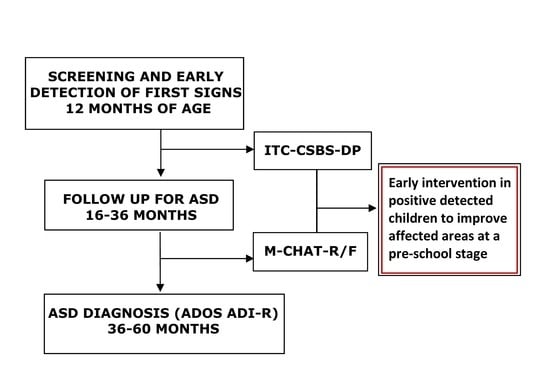
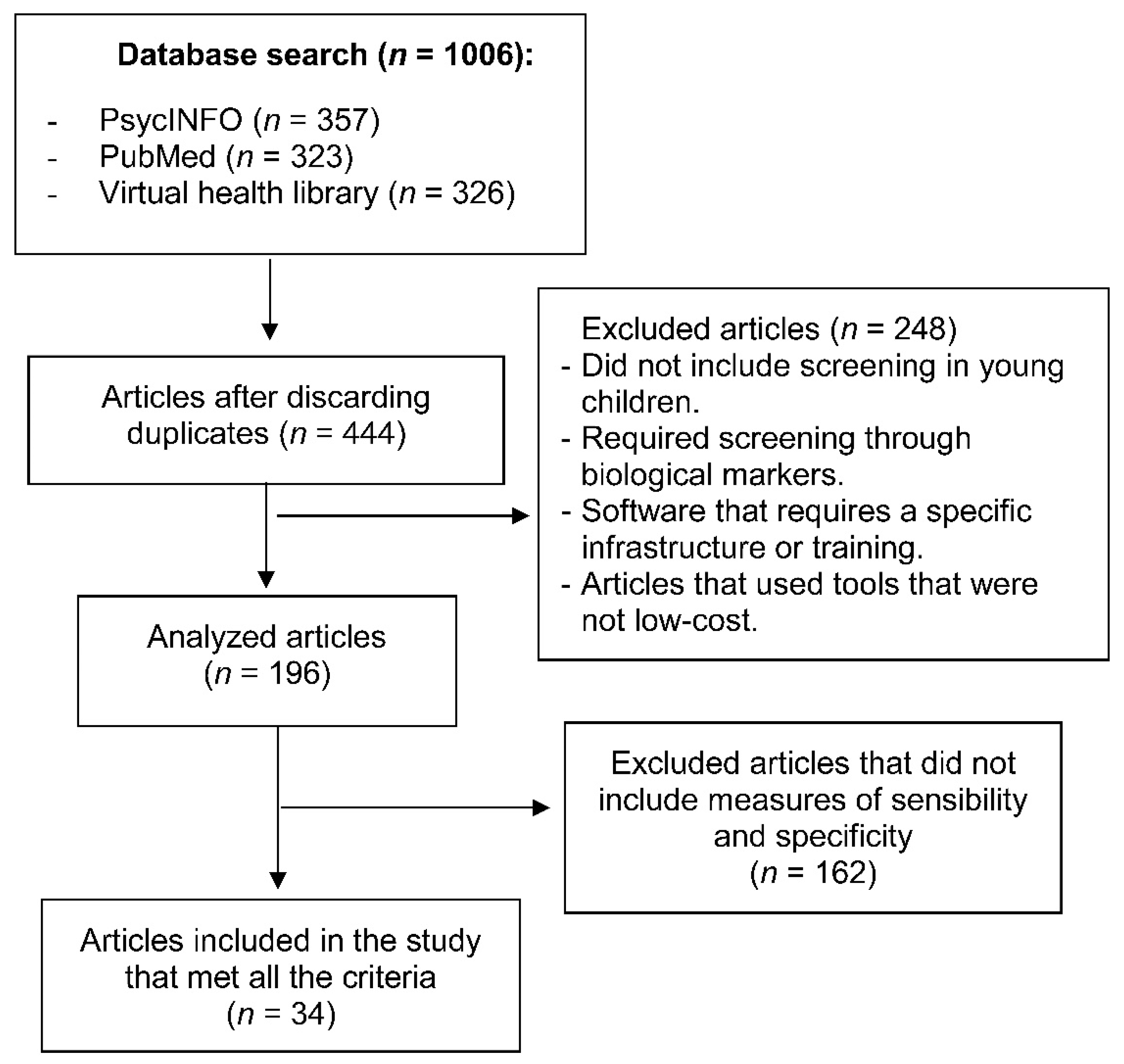
2. Material and Methods
3. Inclusion and Exclusion Criteria
4. Data Extraction
5. Results
6. Discussion
7. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Christensen, D.L.; Bilder, D.A.; Zahorodny, W.; Pettygrove, S.; Durkin, M.S.; Fitzgerald, R.T.; Rice, C.; Kurzius-Spencer, M.; Baio, J.; Yeargin-Allsopp, M. Prevalence and Characteristics of Autism Spectrum Disorder Among 4-Year-Old Children in the Autism and Developmental Disabilities Monitoring Network. J. Dev. Behav. Pediatr. 2016, 37, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Baio, J.; Wiggins, L.; Christensen, D.L.; Maenner, M.J.; Daniels, J.; Warren, Z.; Kurzius-Spencer, M.; Zahorodny, W.; Robinson Rosenberg, C.; White, T.; et al. Prevalence of Autism Spectrum Disorders in a Total Population Sample-Autism and Developmental Disabilities Monitoring Network, 11 Sites, United States, 2014. MMWR Surveill Summ. 2018, 67, 1–25. [Google Scholar] [CrossRef] [PubMed]
- Hernandez, J.M.; Artigas-Pallares, J.; Martos-Perez, J.; Palacios, S.; Fuentes-Biggi, J.; Belinchon-Carmona, M.; Canal-Bedia, R.; Diez-Cuervo, A.; Ferrari-Arroyo, M.J.; Hervas, A.; et al. Guía de buena práctica para la detección temprana de los trastornos del espectro autista. Rev. Neurol. 2005, 41, 237–245. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Jones, E.J.H.; Gliga, T.; Bedford, R.; Charman, T.; Johnson, M.H. Developmental pathways to autism: A review of prospective studies of infants at risk. Neurosci. Biobehav. Rev. 2014, 39, 1–33. [Google Scholar] [CrossRef] [Green Version]
- Chawarska, K.; Paul, R.; Klin, A.; Hannigen, S.; Dichtel, L.E.; Volkmar, F. Parental Recognition of Developmental Problems in Toddlers with Autism Spectrum Disorders. J. Autism Dev. Disord. 2007, 37, 62–72. [Google Scholar] [CrossRef]
- Zwaigenbaum, L.; Bryson, S.; Garon, N. Early identification of autism spectrum disorders. Behav. Brain Res. 2013, 251, 133–146. [Google Scholar] [CrossRef] [PubMed]
- Beranova, S.; Stoklasa, J.; Dudova, I.; Markova, D.; Kasparova, M.; Zemankova, J.; Urbanek, T.; Talasek, T.; Luukka, P.; Hrdlicka, M. A possible role of the Infant/Toddler Sensory Profile in screening for autism: A proof-of-concept study in the specific sample of prematurely born children with birth weights <1500 g. Neuropsychiatr. Dis. Treat. 2017, 13, 191–200. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- DMoher, L.A.; Tetzlaff, J.; Altman, D.G. Prisma Group Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. PLoS Med. 2009, 6, e1000097. [Google Scholar] [CrossRef] [Green Version]
- Petrocchi, S.; Levante, A.; Lecciso, F. Systematic Review of Level 1 and Level 2 Screening Tools for Autism Spectrum Disorders in Toddlers. Brain Sci. 2020, 10, 180. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sacrey, L.R.; Bryson, S.; Zwaigenbaum, L.; Brian, J.; Smith, I.M.; Roberts, W.; Szatmari, P.; Vaillancourt, T.; Roncadin, C.; Garon, N. The Autism Parent Screen for Infants: Predicting risk of autism spectrum disorder based on parent-reported behavior observed at 6-24 months of age. Autism 2018, 22, 322–334. [Google Scholar] [CrossRef]
- Bong, G.; Kim, J.H.; Hong, Y.; Yoon, N.H.; Sunwoo, H.; Jang, J.Y.; Oh, M.; Lee, K.S.; Jung, S.; Yoo, H.J. The Feasibility and Validity of Autism Spectrum Disorder Screening Instrument: Behavior Development Screening for Toddlers (BeDevel)-A Pilot Study. Autism Res. 2019, 12, 1112–1128. [Google Scholar] [CrossRef]
- Sipes, M.; Matson, J.L.; Turygin, N. The use of the Battelle Developmental Inventory–Second Edition (BDI-2) as an early screener for autism spectrum disorders. Dev. Neurorehabil. 2011, 14, 310–314. [Google Scholar] [CrossRef] [PubMed]
- Matson, J.L.; Wilkins, J.; Sharp, B.; Knight, C.; Sevin, J.A.; Boisjoli, J.A. Sensitivity and specificity of the Baby and Infant Screen for Children with aUtIsm Traits (BISCUIT): Validity and cutoff scores for autism and PDD-NOS in toddlers. Res. Autism Spectr. Disord. 2009, 3, 924–930. [Google Scholar] [CrossRef]
- Kiss, I.G.; Feldman, M.S.; Sheldrick, R.C.; Carter, A.S. Developing Autism Screening Criteria for the Brief Infant Toddler Social Emotional Assessment (BITSEA). J. Autism Dev. Disord. 2017, 47, 1269–1277. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Arun, P.; Chavan, B.S. Development of a screening instrument for autism spectrum disorder: Chandigarh Autism Screening Instrument. Indian J. Med. Res. 2018, 147, 369–375. [Google Scholar] [CrossRef]
- Dereu, M.; Raymaekers, R.; Warreyn, P.; Schietecatte, I.; Meirsschaut, M.; Roeyers, H. Can child care workers contribute to the early detection of autism spectrum disorders? A comparison between screening instruments with child care workers versus parents as informants. J. Autism Dev. Disord. 2012, 42, 781–796. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Havdahl, K.A.; von Tetzchner, S.; Huerta, M.; Lord, C.; Bishop, S.L. Utility of the Child Behavior Checklist as a Screener for Autism Spectrum Disorder. Autism Res. 2016, 9, 33–42. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Limberg, K.; Gruber, K.; Noterdaeme, M. The German version of the Child Behavior Checklist 1.5-5 to identify children with a risk of autism spectrum disorder. Autism 2017, 21, 368–374. [Google Scholar] [CrossRef]
- Dereu, M.; Roeyers, H.; Raymaekers, R.; Meirsschaut, M.; Warreyn, P. How useful are screening instruments for toddlers to predict outcome at age 4? General development, language skills, and symptom severity in children with a false positive screen for autism spectrum disorder. Eur. Child Adolesc Psychiatry 2012, 21, 541–551. [Google Scholar] [CrossRef] [PubMed]
- David, D.; Dobrean, A.; Mogoaşe, C.; Dobrescu, I. Screening for autism in Romanian population: An initial study investigating the clinical utility of the Screening Questionnaire for Autism Spectrum Disorders (Chestionarul de Screening pentru Tulburări de Spectru Autist—CS-TSA). Transylv. J. Psychol. 2013, 14, 127–148. [Google Scholar]
- Gray, K.M.; Tonge, B.J.; Sweeney, D.J.; Einfeld, S.L. Screening for Autism in young children with developmental delay: An evaluation of the Developmental Behavior Checklist: Early Screen. JADD 2008, 38, 1003–1010. [Google Scholar] [CrossRef]
- Tsai, W.-C.; Soong, W.-T.; Shyu, Y.-I.L. Toddler autism screening questionnaire: Development and potential clinical validity. Autism 2012, 16, 340–349. [Google Scholar] [CrossRef] [PubMed]
- Fallucco, E.M.; Wysocki, T.; James, L.; Kozikowski, C.; Williams, A.; Gleason, M.M. The Brief Early Childhood Screening Assessment: Preliminary Validity in Pediatric Primary Care. J Dev Behav Pediatr. 2017, 38, 89–98. [Google Scholar] [CrossRef] [PubMed]
- Watson, L.R.; Baranek, G.T.; Crais, E.R.; Reznick, J.S.; Dykstra, J.; Perryman, T. The First Year Inventory: Retrospective parent responses to a questionnaire designed to identify one-year-olds at risk for autism. J. Autism Dev. Disord. 2007, 37, 49–61. [Google Scholar] [CrossRef]
- Wetherby, A.M.; Brosnan-maddox, S.; Peace, V.; Newton, L. Validation of the Infant-Toddler Checklist as a Broadband Screener for Autism Spectrum Disorders from 9 to 24 Months of Age. Autism 2008, 12. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Canal-Bedia, R.; García-Primo, P.; Martín-Cilleros, M.V.; Santos-Borbujo, J.; Guisuraga-Fernández, Z.; Herráez-García, L.; Herráez-García, M.M.; Boada-Muñoz, L.; Fuentes-Biggi, J.; Posada-de, L.P.M. Modified checklist for autism in toddlers: Cross-cultural adaptation and validation in Spain. J. Autism Dev. Disord. 2011, 41, 1342–1351. [Google Scholar] [CrossRef]
- Seif Eldin, A.; Habib, D.; Noufal, A.; Farrag, S.; Bazaid, K.; Al-Sharbati, M.; Badr, H.; Moussa, S.; Essali, A.; Gaddour, N. Use of M-CHAT for a multinational screening of young children with autism in the Arab countries. Int. Rev. Psychiatry 2008, 20, 281–289. [Google Scholar] [CrossRef] [PubMed]
- Kim, S.H.; Joseph, R.M.; Frazier, J.A.; O’Shea, T.M.; Chawarska, K.; Allred, E.N.; Leviton, A.; Kuban, K.K. Extremely Low Gestational Age Newborn (ELGAN) Study Investigators. Predictive validity of the Modified Checklist for Autism in Toddlers (M-CHAT) born very preterm. J. Pediatr. 2016, 178, 101–107. [Google Scholar] [CrossRef] [Green Version]
- Srisinghasongkram, P.; Pruksananonda, C.; Chonchaiya, W. Two-Step Screening of the Modified Checklist for Autism in Toddlers in Thai Children with Language Delay and Typically Developing Children. J. Autism Dev. Disord. 2016, 46, 3317–3329. [Google Scholar] [CrossRef]
- Sturner, R.; Howard, B.; Bergmann, P.; Morrel, T.; Andon, L.; Marks, D.; Rao, P.; Landa, R. Autism Screening with Online Decision Support by Primary Care Pediatricians Aided by M-CHAT/F. Pediatrics 2016, 138. [Google Scholar] [CrossRef] [Green Version]
- Robins, D.; Casagrande, K.; Barton, M.; Chen, C.-M.; Dumont-Mathieu, T.; Fein, D. Validation of the Modified Checklist for Autism in Toddlers, Revised with Follow-up (M-CHAT-R/F). Pediatrics 2014, 133, 37–45. [Google Scholar] [CrossRef] [Green Version]
- Kamio, Y.; Inada, N.; Koyama, T.; Inokuchi, E.; Tsuchiya, K.; Kuroda, M. Effectiveness of using the Modified Checklist for Autism in Toddlers in two-stage screening of autism spectrum disorder at the 18-month health check-up in Japan. J. Autism Dev. Disord. 2014, 44, 194–203. [Google Scholar] [CrossRef]
- Perera, H.; Jeewandara, K.C.; Seneviratne, S.; Guruge, C. Culturally adapted pictorial screening tool for autism spectrum disorder: A new approach. World J. Clin. Pediatr. 2017, 6, 45–51. [Google Scholar] [CrossRef]
- Zahorodny, W.; Shenouda, J.; Mehta, U.; Yee, E.; Garcia, P.; Rajan, M.; Goldfarb, M. Preliminary Evaluation of a Brief Autism Screener for Young Children. J. Dev. Behav. Pediatr. 2018, 39, 183–191. [Google Scholar] [CrossRef]
- Feldman, M.A.; Ward, R.A.; Savona, D.; Regehr, K.; Parker, K.; Hudson, M.; Penning, H.; Holden, J.J. Development and initial validation of a parent report measure of the behavioral development of infants at risk for autism spectrum disorders. J Autism Dev. Disord. 2012, 42, 13–22. [Google Scholar] [CrossRef]
- Smith, N.J.; Sheldrick, C.; Perrin, E.L. An abbreviated screening instrument for autism spectrum disorders. Infant Ment. Health J. 2013, 34, 149–155. [Google Scholar] [CrossRef]
- Olliac, B.; Crespin, G.; Laznik, M.C.; Cherif Idrissi El Ganouni, O.; Sarradet, J.L.; Bauby, C.; Dandres, A.M.; Ruiz, E.; Bursztejn, C.; Xavier, J.; et al. Infant and dyadic assessment in early community-based screening for autism spectrum disorder with the PREAUT grid. PLoS ONE 2017, 12, e0188831. [Google Scholar] [CrossRef] [Green Version]
- Allison, C.; Auyeung, B.; Baron-Cohen, S. Toward brief “red flags” for autism screening: The Short Autism Spectrum Quotient and the Short Quantitative Checklist for Autism in Toddlers in 1000 cases and 3000 controls. J. Am. Acad. Child Adolesc. Psychiatry 2012, 51, 338. [Google Scholar] [CrossRef]
- Barbaro, J.; Dissanayake, C. Prospective identification of autism spectrum disorders in infancy and toddlerhood using developmental surveillance: The social attention and communication study. J. Dev. Behav. Pediatr. 2010, 3, 376–385. [Google Scholar] [CrossRef] [PubMed]
- Stone, W.L.; McMahon, C.R.; Henderson, L.M. Use of the Screening Tool for Autism in Two-Year-Olds (STAT) for children under 24 months: An exploratory study. Autism 2008, 12, 557–573. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Dow, D.; Day, T.N.; Kutta, T.J.; Nottke, C.; Wetherby, A.M. Screening for autism spectrum disorder in a naturalistic home setting using the systematic observation of red flags (SORF) at 18-24 months. Autism Res. 2020, 13, 122–133. [Google Scholar] [CrossRef]
- Oner, P.; Oner, O.; Munir, K. Three-Item Direct Observation Screen (TIDOS) for autism spectrum disorder. Autism 2014, 18, 733–742. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Honda, H.; Shimizu, Y.; Nitto, Y.; Imai, M.; Ozawa, T.; Iwasa, M.; Shiga, K.; Hira, T. Extraction and Refinement Strategy for detection of autism in 18-month-olds: A guarantee of higher sensitivity and specificity in the process of mass screening. J. Child Psychol. Psychiatry 2009, 50, 972–981. [Google Scholar] [CrossRef]
- Briggs-Gowan, M.; Carter, A.; Irwin, J.; Wachtel, K.; Cicchetti, D. The Brief-Infant Toddler Social and Emotional Assessment: Screening for social emotional problems and delays in competence. J. Pediatr. Psychol. 2004, 29, 143–155. [Google Scholar] [CrossRef] [PubMed]
- Towle, P.O.; Patrick, P.A. Autism Spectrum Disorder Screening Instruments for Very Young Children: A Systematic Review. Autism Res. Treat. 2016, 2016, 1–29. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cunningham, S. Examining the Validity of the Autism Spectrum Rating Scales with a Preschool Population Referred for Special Education Evaluation; Department of Educational Psychology, University of Utah: Salt Lake City, UT, USA, 2013. [Google Scholar]
- Bradstreet, L.E.; Juechter, J.I.; Kamphaus, R.W.; Kerns, C.M.; Robins, D.L. Using the BASC-2 Parent Rating Scales to screen for autism spectrum disorder in toddlers and preschool-aged children. J. Abnorm. Child Psychol. 2017, 45, 359–370. [Google Scholar] [CrossRef] [Green Version]
- Mayes, S.D. Brief Report: Checklist for Autism Spectrum Disorder: Most Discriminating Items for Diagnosing Autism. J. Autism Dev. Disord. 2017, 1–5. [Google Scholar] [CrossRef]
- Morales-Hidalgo, P.; Roige-Castellvi, J.; Vigil-Colet, A.; Sans, J.C. The Childhood Autism Spectrum Test (CAST): Spanish adaptation and validation. Autism Res. 2017, 10, 1491–1498. [Google Scholar] [CrossRef] [PubMed]
- Morales-Hidalgo, P.; Hernández-Martínez, C.; Voltas, N.; Canals, J. EDUTEA: A DSM-5 teacher screening questionnaire for autism spectrum disorder and social pragmatic communication disorder. Int. J. Clin. Heal. Psychol. 2017, 17, 269–281. [Google Scholar] [CrossRef]
- Nygren, G.; Sandberg, E.; Gillstedt, F.; Ekeroth, G.; Arvidsson, T.; Gillberg, C. A new screening programme for autism in a general population of Swedish toddlers. Res. Dev. Disabil. 2012, 33, 1200–1210. [Google Scholar] [CrossRef]
- Paula, C.S.; Cunha, G.R.; Bordini, D.; Brunoni, D.; Moya, A.C.; Bosa, C.A.; Mari, J.J.; Cogo-Moreira, H. Identifying Autism with a Brief and Low-Cost Screening Instrument—OERA: Construct Validity, Invariance Testing, and Agreement Between Judges. J. Autism Dev. Disord. 2017, 1–12. [Google Scholar] [CrossRef] [PubMed]
- Johnson, S.; Hollis, C.; Hennessy, E.; Kochhar, P.; Wolke, D.; Marlow, N. Screening for autism in preterm children: Diagnostic utility of the Social Communication Questionnaire. Arch. Dis. Child. 2011, 96, 73–77. [Google Scholar] [CrossRef] [PubMed]
- Crais, E.R.; Watson, L.R. Challenges and opportunities in early identification and intervention for children at-risk for autism spectrum disorders. Int. J. Speech. Lang. Pathol. 2014, 16, 23–29. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Estes, A.; Vismara, L.; Mercado, C.; Fitzpatrick, A.; Elder, L.; Greenson, J.; Lord, C.; Munson, J.; Winter, J.; Young, G. The impact of parent-delivered intervention on parents of very young children with autism. J. Autism Dev. Disord. 2014, 44, 353–365. [Google Scholar] [CrossRef]
- Benvenuto, A.; Marciano, S.; Capuano, I.; Curatolo, P. An update on autism spectrum disorders in children. Minerva Pediatr. 2013, 65, 19–36. [Google Scholar]
- Bradshaw, J.; Steiner, A.M.; Gengoux, G.; Koegel, L.K. Feasibility and effectiveness of very early intervention for infants at-risk for autism spectrum disorder: A systematic review. J. Autism Dev. Disord. 2015, 45, 778–794. [Google Scholar] [CrossRef]
- Shattuck, P.T.; Durkin, M.; Maenner, M.; Newschaffer, C.; Mandell, D.S.; Wiggins, L.; Lee, L.C.; Rice, C.; Giarelli, E.; Kirby, R.; et al. Timing of identification among children with an autism spectrum disorder: Findings from a population-based surveillance study. J. Am. Acad. Child Adolesc. Psychiatry 2009, 48, 474–483. [Google Scholar] [CrossRef] [Green Version]
- Barton, M.L.; Dumont-Mathieu, T.; Fein, D. Screening young children for autism spectrum disorders in primary practice. J. Autism Dev. Disord. 2012, 42, 1165–1174. [Google Scholar] [CrossRef]
- Rutherford, M.; Burns, M.; Gray, D.; Bremner, L.; Clegg, S.; Russell, L.; Smith, C.; O’Hare, A. Improving Efficiency and Quality of the Children’s ASD Diagnostic Pathway: Lessons Learned from Practice. J. Autism Dev. Disord. 2018, 48, 1579–1595. [Google Scholar] [CrossRef] [Green Version]
- Pierce, K.; Carter, C.; Weinfeld, M.; Desmond, J.; Hazin, R.; Bjork, R.; Gallagher, N. Detecting, Studying, and Treating Autism Early: The One-Year Well-Baby Check-Up Approach. J. Pediatr. 2011, 159, 458–465.e6. [Google Scholar] [CrossRef] [Green Version]
- JMatson, L.; Rivet, T.T.; Fodstad, J.C.; Dempsey, T.; Boisjoli, J.A. Examination of adaptive behavior differences in adults with autism spectrum disorders and intellectual disability. Res. Dev. Disabil. 2009, 30, 1317–1325. [Google Scholar] [CrossRef] [PubMed]
- Ibañez, L.V.; Stoep, A.V.; Myers, K.; Zhou, C.; Dorsey, S.; Steinman, K.J.; Stone, W.L. Promoting early autism detection and intervention in underserved communities: Study protocol for a pragmatic trial using a stepped-wedge design. BMC Psychiatry. 2019, 19, 169. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Devescovi, R.; Monasta, L.; Bin, M.; Bresciani, G.; Mancini, A.; Carrozzi, M.; Colombi, C. A Two-Stage Screening Approach with I-TC and Q-CHAT to Identify Toddlers at Risk for Autism Spectrum Disorder within the Italian Public Health System. Brain Sci. 2020, 10, 184. [Google Scholar] [CrossRef] [Green Version]
- Cicchetti, D.V. The precision of reliability and validity estimates re-visited: Distinguishing between clinical and statistical significance of sample size requirements. J Clin. Exp. Neuropsychol. 2001, 23, 695–700. [Google Scholar] [CrossRef] [PubMed]
- Miller, J.S.; Gabrielsen, T.; Villalobos, M.; Alleman, R.; Wahmhoff, N.; Carbone, P.S.; Segura, B. The each child study: Systematic screening for autism spectrum disorders in a pediatric setting. Pediatrics 2011, 127, 866–871. [Google Scholar] [CrossRef]
| Instrument | Administration Age (Months) | Used Sample (Children) | Sensitivity | Specificity | Positive Predictive Value (PPV) | Negative Predictive Value (NPV) | Reference |
|---|---|---|---|---|---|---|---|
| APSI | 6–24 | 204 high-risk, 79 low-risk controls | 0.67 | 0.87 | 6–8 months: 0.43 21–24 months: 0.79 | 0.87–0.99 | [10] |
| BeDevel | 18–42 | 155 (75 ASD, 55 NT, 25 OPD) | 0.83 | 0.81 | 0.80 | 0.83 | [11] |
| BDI-II | 0–95 | 604 ASD, 1064 NT | 0.94 | 0.31 | --- | --- | [12] |
| BISCUIT | 17–37 | 1007 risk of ASD | 0.93 | 0.86 | … | … | [13] |
| BITSEA | 11–48 | 223 ASD, 289 non-ASD | Up to 24 months: 0.91 | Up to 24 months: 0.80 | --- | --- | [14] |
| CASI (for Indi) | 18-120 | 405 (75 ID, 83 ASD, 87 OPD, 160 NT) | 0.89 | 0.89 | 0.67 | 0.96 | [15] |
| CBCL 1.5-5 | 18–71 | 226 ASD, 163 OPD | 0.74 | 0.53 | --- | --- | [16] |
| CBCL 1.5-5 (Withdrawn PDP Scale) | 18–59 | 101 ASD, 117 NT | Withdrawn: 0.89 PDP: 0.85 | Withdrawn: 0.92 PDP: 0.90 | Withdrawn: 0.90 PDP: 0.88 | Withdrawn: 0.90 PDP: 0.87 | [17] |
| 18–59 | 80 ASD, 103 OPD | Withdrawn: 0.88 PDP: 0.83 | Withdrawn: 0.63 PDP: 0.60 | Withdrawn: 0.65 PDP: 0.62 | Withdrawn: 0.87 PDP: 0.82 | [18] | |
| CESDD | 3–39 | 357 risk of ASD or language problems | 0.92 and 0.90 | 0.73 and 0.68 | 0.19 and 0.32 | 0.99 and 0.98 | [19] |
| CS-TSA | 18–60 | 27 ASD, 41 OPD, 64 NT | Section 1: 0.89 Section 2: 0.78 | Section 1: 0.68 Section 2: 0.79 | --- | --- | [20] |
| DBC-ES | 18–48 | n = 142 ASD or PDD n = 65 OPD | 0.83 | 0.48 | 0.78 | 0.56 | [21] |
| Screening questionnaire developed for Taiwan | 18–24 | 18 ASD, 59 NT | 1 | 0.96 | 0.90 | 1 | [22] |
| ECSA (Brief) | 18–60 | 69 ASD | 0.89 | 0.85 | --- | --- | [23] |
| FYI | 12 | 38 ASD, 15 NO-ASD, developmental delay 40 NT | 0.92 | 0.78 | 0.74 | 0.93 | [24] |
| ITC/CSBS-DP | 6–24 | 5385 general population | 0.93 | 0.89 | 12–24 months: +0.70 | 12–24 months: +0.87 | [25] |
| M-CHAT | 16–30 | Sample 1: 2480 High- and low-risk Sample 2: 2055 low-risk | Both samples: 1 | Both samples: 0.98 | M1: 0.35 M2: 0.19 | 1 | [26] |
| 122 risk of ASD, 106 NT | 0.86 | 0.80 | 0.88 | --- | [27] | ||
| 966 born very premature | 0.52 | 0.84 | 0.20 | 0.96 | [28] | ||
| 109 language delay 732 NT | 0.90 | 0.99 | 0.96 | 0.99 | [29] | ||
| M-CHAT/F | 16/30 | 341 positive for M-CHAT | 0.55 | 0.79 | 0.78 | --- | [30] |
| M-CHAT-R/F | 16–30 | 15,612 general population | 0.96 | 0.86 | 0.47 | 0.99 | [31] |
| M-CHAT-JV/F | 16–30 | 1851 general population | 0.47 | 0.98 | 0.45 | --- | [32] |
| PAAS | 18–48 | 105 general population | 0.88 | 0.93 | 0.95 | 0.84 | [33] |
| PDQ-1 | 18–36 | 42 ASD, 38 OPD, 100 NT | 0.85 | 0.99 | 0.88 | 0.99 | [34] |
| POEMS | 1–24 | 108 high-risk | 0.74 | 0.73 | [35] | ||
| POSI | 16–48 | 232 children (16–36 months) | 0.83 | 0.75 | --- | --- | [36] |
| PREAUT Grid | 4–24 | 4755 general population | P-4: 0.16 a 0.21 P-9: 0.30 a 0.41 P-24: 0.40–0.41 | P-4: 0.99 P-9: 0.99 P-24: 0.99 | P-4: 0.25 a 0.26 P-9: 0.20 a 0.36 P-24: 0.26 a 0.27 | P-4: 0.99 P-9: 0.99 P-24: 0.99 | [37] |
| Q-CHAT-10 | 18–24 | 126 ASD | 0.91 | 0.89 | 0.58 | --- | [38] |
| SACS | 12–24 | 20,770 general population | 0.69 a 0.83 | 0.99 | 0.81 | --- | [39] |
| STAT | 12–23 | 71 siblings with ASD | 0.95 | 0.73 | 0.56 | 0.97 | [40] |
| SORF | 18–24 | n = 84 ASD, n = 82 OPD, n = 62 NT | 0.80 | 0.78 | 0.81 | 0.78 | [41] |
| TIDOS | 18–60 | n = 86 ASD n = 76 OPD n = 97 general population | 0.95 | 0.85 | 0.91 | 0.90 | [42] |
| YACHT-18 | 18 | 2814 general population | 0.60 ASD, 0.82 other developmental disorders | 0.86 for developmental disorders | --- | --- | [43] |
| Instrument | Administration Age (Years) | Sample Used | Sensitivity | Specificity | Positive Predictive Value (PPV) | Negative Predictive Value (NPV) | Reference |
|---|---|---|---|---|---|---|---|
| AQ-10 Child | 4–11 | 432 ASD | 0.95 | 0.97 | 0.94 | --- | [38] |
| ASRS | 2–18 | 37 ASD, 30 OPD | Parents: 0.64 Teachers: 0.52 | Parents: 63.30 Teachers: 0.71 | Parents: 0.68 Teachers: 0.61 | Parents: 0.59 Teachers: 0.62 | [46] |
| BASC-2 (PRS-P) | 2–5 | 224 positive ASD screening | 0.76 | 0.73 | 0.86 | 0.57 | [47] |
| CASD CASD SF | 3–17 | 469 ASD, 138 OPD | CASD: 0.86 CASD SF: 0.95 | CASD: 100 CASD SF: 0.96 | … | … | [48] |
| CAST | 4–12 | 1496 general population | Complete version: 0.83 Reduced version: 0.85 | Complete version: 0.92 Reduced version: 0.91 | Complete version: 0.63 Reduced version: 0.61 | --- | [49] |
| EDUTEA | 3–12 | 2660 general population | 0.87 | 0.91 | 0.86 | 0.99 | [50] |
| M-CHAT and JA-OBS | 2–3 | 3999 general population | 0.90 | --- | 0.96 | --- | [51] |
| OERA | 3–10 | 76 ASD, 23 non-ASD | 0.92 | 0.91 | 0.92 | --- | [52] |
| SCQ | 3–7 | 219 premature children | 0.91 | 0.86 | 0.31 | 0.99 | [53] |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Salgado-Cacho, J.M.; Moreno-Jiménez, M.d.P.; de Diego-Otero, Y. Detection of Early Warning Signs in Autism Spectrum Disorders: A Systematic Review. Children 2021, 8, 164. https://0-doi-org.brum.beds.ac.uk/10.3390/children8020164
Salgado-Cacho JM, Moreno-Jiménez MdP, de Diego-Otero Y. Detection of Early Warning Signs in Autism Spectrum Disorders: A Systematic Review. Children. 2021; 8(2):164. https://0-doi-org.brum.beds.ac.uk/10.3390/children8020164
Chicago/Turabian StyleSalgado-Cacho, José María, María del Pilar Moreno-Jiménez, and Yolanda de Diego-Otero. 2021. "Detection of Early Warning Signs in Autism Spectrum Disorders: A Systematic Review" Children 8, no. 2: 164. https://0-doi-org.brum.beds.ac.uk/10.3390/children8020164