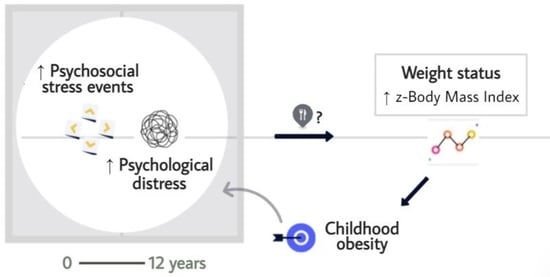
Linking Psychosocial Stress Events, Psychological Disorders and Childhood Obesity
Abstract
:1. Introduction
2. Materials and Methods
2.1. Participants and Procedure
2.2. Instruments of Assessment
- ▪
- Children’s anthropometric data. Height and weight were measured using a digitally calibrated scale (Type SECA 799 and 769) and a tallimeter at the primary care centres. Child weight status was calculated according to BMI standard deviation scores (BMI z-scores). BMI z-scores were computed by comparing the children’s BMI scores with the ideal BMI of the general population of the same age and sex [36] The average range of z-scores in the whole sample was between −0.33 (SD = 0.76) and +3.08 (SD = 0.83).
- ▪
- Socio-demographic variables. Trained staff carried out a structured medical-psychosocial interview (information about age, marital status, level of education, job occupation and medical and psycho-family history) with the children and their primary caregiver. Families’ socioeconomic status (SES) was calculated using the Hollingshead index [39].
- ▪
- Psychological distress. The prevalence of child psychological disorders in the sample was assessed by trained interviewers through a semi-structured interview to diagnose current and past episodes of psychopathology in children and adolescents according to the DSM-5 (K-SADS-PL, 2018) [40]. The interview was conducted first with the children, and then the primary caregiver confirmed the information. For the current study, we used two categories: 0 (absent disorder) and 2 (definitive clinical disorder).
- ▪
- Psychosocial Stress Events (PSEs). This scale is a new version created ad hoc after a comprehensive systematic review of common stressful events for primary school-aged children (8 to 12 years old). The inventory by Oliva et al. (2008) served as the main reference [7]. A panel of five evaluators was created to check the validity of the structure and content of the items proposed in this new version. The inter-rater reliability of the new questionnaire was calculated by administering the Free Marginal Kappa (k) statistical tool among five evaluators. Kappa scores higher than 0.90 were obtained for all the items except one (k = 0.60), which was eliminated from the original version. A pilot study was carried out to verify that it was understandable for children between 8 and 12, with adequate responses. Finally, the scale consists of 27 items that comprises three subscales related with adversities to personal (e.g., medical condition), family (e.g., parent’s divorce, serious illness of a relative, sibling rivalry) and school and social environments (e.g., class year repetition, change of school, bullying) during school years. There are two categories of response by the children, depending on whether or not each event occurred (Yes/No). The instrument obtained satisfactory internal consistency of 0.83. The total score corresponds to the sum of the number of events reported by the child. Higher scores indicate a higher number of stress events (PSEs) [41].
2.3. Statistical Analysis
3. Results
3.1. Anthropometric and Sociodemographic: Characteristics of the Sample
3.2. Differences in Accumulation of Psychosocial Stress Events and Psychological Problems in children by Weight Status
3.2.1. Accumulation of Psychosocial Stress Events by Weight Status
3.2.2. Psychological Distress by Weight Status
3.3. Association between Psychosocial Stress Events, Weight Status and Childhood Mental Disorders
3.4. Predictive Model of Psychosocial Stress Events on Status of Weight via Psychological Problems: Multiple Linear Regression Model
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Compas, B.E. Stress and life events during childhood and adolescence. Clin. Psychol. Rev. 1987, 7, 275–302. [Google Scholar] [CrossRef]
- Grant, K.E.; Compas, B.E.; Stuhlmacher, A.F.; Thurm, A.E.; McMahon, S.D.; Halpert, J.A. Stressors and child and adolescent psychopathology: Moving from markers to mechanisms of risk. Psychol. Bull. 2003, 129, 447–466. [Google Scholar] [CrossRef] [Green Version]
- Sandín, B. El estrés: Un análisis basado en el papel de los factores sociales. Int. J. Clin. Health Psychol. 2003, 3, 141–157. [Google Scholar]
- Jiménez, L.; Menéndez, S.; Hidalgo, M. Un análisis de los acontecimientos vitales estresantes durante la adolescencia. Apunt. Psicol. 2012, 30, 523–531. [Google Scholar]
- Hughes, K.; Bellis, M.A.; Hardcastle, K.A.; Sethi, D.; Butchart, A.; Mikton, C.; Jones, L.; Dunne, M.P. The effect of multiple adverse childhood experiences on health: A systematic review and meta-analysis. Lancet Public Heal. 2017, 2, e356–e366. [Google Scholar] [CrossRef] [Green Version]
- Kerker, B.D.; Zhang, J.; Nadeem, E.; Stein, R.E.; Hurlburt, M.S.; Heneghan, A.; Landsverk, J.; Horwitz, S.M. Adverse Childhood Experiences and Mental Health, Chronic Medical Conditions, and Development in Young Children. Acad. Pediatr. 2015, 15, 510–517. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Delgado, A.O.; Morago, J.M.J.; Jimenez, A.P.; Sánchez-Queija, I. Acontecimientos vitales estresantes, resiliencia y ajuste adolescente. Rev. Psicopatología y Psicol. Clínica 2008, 13, 53–62. [Google Scholar] [CrossRef] [Green Version]
- Rey-Bruguera, M.; del Rosario Martínez Arias, M.; Calonge Romano, I. Situaciones estresantes cotidianas en la infancia y su relación con la sintomatología y la adaptación. Psicol. Conduct. 2017, 25, 483–502. [Google Scholar]
- Bright, M.A.; Knapp, C.; Hinojosa, M.S.; Alford, S.; Bonner, B. The Comorbidity of Physical, Mental, and Developmental Conditions Associated with Childhood Adversity: A Population Based Study. Matern. Child Heal. J. 2016, 20, 843–853. [Google Scholar] [CrossRef] [PubMed]
- Hunt, T.K.; Slack, K.S.; Berger, L.M. Adverse childhood experiences and behavioral problems in middle childhood. Child Abus. Negl. 2017, 67, 391–402. [Google Scholar] [CrossRef] [Green Version]
- Moreno-Encinas, A.; Sepúlveda, A.; Kurland, V.; Lacruz, T.; Nova, E.; Graell, M. Identifying psychosocial and familial correlates and the impact of the stressful life events in the onset of anorexia nervosa: Control-case study (ANOBAS). Psychiatry Res. 2020, 284, 112768. [Google Scholar] [CrossRef]
- Gundersen, C.; Mahatmya, D.; Garasky, S.; Lohman, B. Linking psychosocial stressors and childhood obesity. Obes. Rev. 2011, 12, e54–e63. [Google Scholar] [CrossRef]
- Elsenburg, L.K.; Van Wijk, K.J.E.; Liefbroer, A.C.; Smidt, N. Accumulation of adverse childhood events and overweight in children: A systematic review and meta-analysis. Obesity 2017, 25, 820–832. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Di Cesare, M.; Sorić, M.; Bovet, P.; Miranda, J.J.; Bhutta, Z.; Stevens, G.A.; Laxmaiah, A.; Kengne, A.-P.; Bentham, J. The epidemiological burden of obesity in childhood: A worldwide epidemic requiring urgent action. BMC Med. 2019, 17, 1–20. [Google Scholar] [CrossRef] [Green Version]
- Shekar, M.; Popkin, B.M. Obesity: Health and Economic Consequences of an Impending Global Challenge; The World Bank: Washington, DC, USA, 2020. [Google Scholar] [CrossRef] [Green Version]
- Simmonds, M.; Burch, J.; Llewellyn, A.; Griffiths, C.; Yang, H.; Owen, C.; Duffy, S.; Woolacott, N. The use of measures of obesity in childhood for predicting obesity and the development of obesity-related diseases in adulthood: A systematic review and meta-analysis. Heal. Technol. Assess. 2015, 19, 1–336. [Google Scholar] [CrossRef] [Green Version]
- Harrison, K.; Bost, K.K.; McBride, B.A.; Donovan, S.M.; Grigsby-Toussaint, D.S.; Kim, J.; Liechty, J.M.; Wiley, A.; Teran-Garcia, M.; Jacobsohn, G.C. Toward a Developmental Conceptualization of Contributors to Overweight and Obesity in Childhood: The Six-Cs Model. Child Dev. Perspect. 2011, 5, 50–58. [Google Scholar] [CrossRef]
- Hemmingsson, E. A new model of the role of psychological and emotional distress in promoting obesity: Conceptual review with implications for treatment and prevention. Obes. Rev. 2014, 15, 769–779. [Google Scholar] [CrossRef]
- Siervo, M.; Wells, J.C.K.; Cizza, G. The Contribution of Psychosocial Stress to the Obesity Epidemic: An Evolutionary Approach. Horm. Metab. Res. 2009, 41, 261–270. [Google Scholar] [CrossRef] [Green Version]
- Flaherty, E.G.; Thompson, R.; Litrownik, A.J.; Zolotor, A.J.; Dubowitz, H.; Runyan, D.K.; English, D.J.; Everson, M.D. Adverse Childhood Exposures and Reported Child Health at Age 12. Acad. Pediatr. 2009, 9, 150–156. [Google Scholar] [CrossRef]
- McKelvey, L.M.; Saccente, J.E.; Swindle, T.M. Adverse Childhood Experiences in Infancy and Toddlerhood Predict Obesity and Health Outcomes in Middle Childhood. Child. Obes. 2019, 15, 206–215. [Google Scholar] [CrossRef]
- Burke, N.J.; Hellman, J.L.; Scott, B.G.; Weems, C.F.; Carrion, V.G. The impact of adverse childhood experiences on an urban pediatric population. Child Abus. Negl. 2011, 35, 408–413. [Google Scholar] [CrossRef] [Green Version]
- Pretty, C.; O’Leary, D.D.; Cairney, J.; Wade, T.J. Adverse childhood experiences and the cardiovascular health of children: A cross-sectional study. BMC Pediatr. 2013, 13, 208. [Google Scholar] [CrossRef] [Green Version]
- Weber, Z.A.; Shoben, A.; Anderson, S.E. Impact of Life Events on Short-Term Change in BMI in Early and Middle Childhood. Obes. 2020, 28, 347–352. [Google Scholar] [CrossRef] [PubMed]
- Turner, H.A.; Finkelhor, D.; Ormrod, R. The effect of lifetime victimization on the mental health of children and adolescents. Soc. Sci. Med. 2006, 62, 13–27. [Google Scholar] [CrossRef] [PubMed]
- Puder, J.J.; Munsch, S. Psychological correlates of childhood obesity. Int. J. Obes. 2010, 34, S37–S43. [Google Scholar] [CrossRef] [Green Version]
- Sepúlveda, A.R.; Solano, S.; Blanco, M.; Lacruz, T.; Graell, M. Prevalence of childhood mental disorders in overweight and obese Spanish children: Identifying loss of control eating. Psychiatry Res. 2018, 267, 175–181. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Vila, G.; Zipper, E.; Dabbas, M.; Bertrand, C.; Robert, J.J.; Ricour, C.; Mouren-Siméoni, M.C. Mental Disorders in Obese Children and Adolescents. Psychosom. Med. 2004, 66, 387–394. [Google Scholar] [CrossRef]
- Evans, G.W.; Fuller-Rowell, T.E.; Doan, S.N. Childhood Cumulative Risk and Obesity: The Mediating Role of Self-Regulatory Ability. Pediatrics 2011, 129, e68–e73. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sepúlveda, A.R.; Lacruz, T.; Solano, S.; Blanco, M.; Moreno, A.; Rojo, M.; Beltrán, L.; Graell, M. Identifying Loss of Control Eating within Childhood Obesity: The Importance of Family Environment and Child Psychological Distress. Children 2020, 7, 225. [Google Scholar] [CrossRef] [PubMed]
- Hartmann, A.S.; Czaja, J.; Rief, W.; Hilbert, A. Psychosocial risk factors of loss of control eating in primary school children: A retrospective case-control study. Int. J. Eat. Disord. 2012, 45, 751–758. [Google Scholar] [CrossRef]
- Hayden-Wade, H.A.; Stein, R.I.; Ghaderi, A.; Saelens, B.E.; Zabinski, M.F.; Wilfley, D.E. Prevalence, Characteristics, and Correlates of Teasing Experiences among Overweight Children vs. Non-overweight Peers. Obes. Res. 2005, 13, 1381–1392. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Van Geel, M.; Vedder, P.; Tanilon, J. Are overweight and obese youths more often bullied by their peers? A meta-analysis on the relation between weight status and bullying. Int. J. Obes. 2014, 38, 1263–1267. [Google Scholar] [CrossRef]
- Blanco, M.; Solano, S.; Alcántara, A.I.; Parks, M.; Román, F.J.; Sepúlveda, A.R. Psychological well-being and weight-related teasing in childhood obesity: A case–control study. Eat. Weight. Disord.—Stud. Anorexia Bulim. Obes. 2020, 25, 751–759. [Google Scholar] [CrossRef] [PubMed]
- Neumarksztainer, D.; Falkner, N.H.; Story, M.; Perry, C.L.; Hannan, P.J.; Mulert, S. Weight-teasing among adolescents: Correlations with weight status and disordered eating behaviors. Int. J. Obes. 2002, 26, 123–131. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- López, C.C.; Raimann, T.X.; Gaete, M.V. Prevención de los trastornos de conducta alimentaria en la era de la obesidad: Rol del clínico. Rev. Médica Clínica Las Condes 2015, 26, 24–33. [Google Scholar] [CrossRef] [Green Version]
- Cole, T.J.; Lobstein, T. Extended international (IOTF) body mass index cut-offs for thinness, overweight and obesity. Pediatr. Obes. 2012, 7, 284–294. [Google Scholar] [CrossRef]
- Sobradillo, B.; Aguirre, A.; Aresti, U.; Bilbao, A.; Fernández-Ramos, C.; Lizarraga, A.; Lorenzo, H.; Madariaga, L.; Rica, I.; Ruiz, I.; et al. Curvas y Tablas de Crecimiento. (Estudio Longitudinal y Transversal); Fundación Faustino Orbegozo: Bilbao, Spain, 2004. [Google Scholar]
- Hollingshead, A.B.; Redlich, F.C. Social Class and Mental Illness: Community Study; John Wiley & Sons Inc.: Hoboken, NJ, USA, 1958. [Google Scholar]
- De la Peña, F.R.; Villavicencio, L.R.; Palacio, J.D.; Félix, F.J.; Larraguibel, M.; Viola, L.; Ortiz, S.; Rosetti, M.; Abadi, A.; Montiel, C.; et al. Validity and reliability of the kiddie schedule for affective disorders and schizophre-nia present and lifetime version DSM-5 (K-SADS-PL-5) Spanish version. BMC Psych. 2018, 18, 193. [Google Scholar]
- Rojo, M.; Beltrán, L.; Moll, A.; Solano, S.; Martínez, M.; Gutiérrez, A. Desarrollo y validación de una escala en castellano para evaluar sucesos vitales estresantes en el contexto familiar y socio-escolar durante la primera infancia. Status: (unpublished).
- Halliday, J.A.; Palma, C.L.; Mellor, D.J.; Green, J.M.; Renzaho, A.M.N. The relationship between family functioning and child and adolescent overweight and obesity: A systematic review. Int. J. Obes. 2014, 38, 480–493. [Google Scholar] [CrossRef]
- Jang, M.; Owen, B.; Lauver, D.R. Different types of parental stress and childhood obesity: A systematic review of observational studies. Obes. Rev. 2019, 20, 1740–1758. [Google Scholar] [CrossRef] [PubMed]
| OBG (n = 85) | OWG (n = 65) | NWG (n = 50) | F/ᵪ2(p) * | |
|---|---|---|---|---|
| Children variables | ||||
| Age (M (SD)) | 10.38 (1.34) | 10.45 (1.19) | 10.14 (1.48) | 0.84 |
| Sex (% (n)) | 15.76 ** | |||
| Male | 40.0 (34) | 66.2 (43) | 32.0 (16) | |
| Female | 60.0 (51) | 33.8 (22) | 68.0 (34) | |
| † BMI z-score (M (SD)) | 3.08 (0.83) | 1.35 (0.46) | −0.33 (0.76) | 371.84 ** |
| Family variables | ||||
| Civil status (% (n)) | 0.32 | |||
| Married/Living together | 70.7 (58) | 73.3 (449) | 70.0 (35) | |
| Divorced/Separated/Single | 28.0 (23) | 25.0 (15) | 28.0 (14) | |
| Widowed | 1.2 (1) | 1.7 (1) | 2.0 (1) | |
| Mother’s level of education (% (n)) | 9.51 * | |||
| No studies/Primary | 8.6 (7) | 5.0 (3) | - | |
| Secondary/Baccalaureate | 70.4 (57) | 56.7 (34) | 69.4 (34) | |
| Higher Ed./University/Postgraduate | 21.0 (17) | 38.3 (23) | 26.5 (13) | |
| Mother’s work situation (% (n)) | 3.93 | |||
| Full-time/Part-time Work | 78.0 (64) | 64.4 (38) | 67.3 (33) | |
| Unemploy/Medical leave/Retirement | 15.9 (13) | 23.7 (14) | 24.5 (12) | |
| Housework | 6.1 (5) | 11.9 (7) | 8.2 (4) | |
| SES (% (n)) | 14.28 | |||
| I Lowest | 7.5 (6) | 12.9 (8) | 4.0 (2) | |
| II | 21.3 (17) | 12.9 (8) | 12.0 (6) | |
| III | 46.3 (37) | 41.9 (26) | 50.0 (25) | |
| IV | 17.5 (14) | 17.7 (11) | 32.0 (16) | |
| V Highest | 7.5 (6) | 14.5 (9) | 2.0 (1) |
| OBG (n = 85) | OWG (n = 65) | NWG (n = 50) | F/ χ2 Overall p-Value | Post Hoc p-Values | |
|---|---|---|---|---|---|
| Total PSE M (SD) | 3.25 (2.25) | 2.36 (1.82) | 1.26 (1.69) | 15.88 p < 0.001 | p < 0.001 |
| Cut-off point ≥ 4 PSE % (n) | 41.2 (35) | 26.2 (17) | 10 (5) | 15.28 p < 0.001 | - |
| Prevalence of psychiatric diagnoses % (n) | 69.41% (59) | 53.84% (35) | 2.0% (1) | 58.92 p < 0.001 | - |
| Model | B | Exp (B) | p |
|---|---|---|---|
| Factor 1: ≥4 PSE | 1.58 | 4.83 | 0.001 |
| Factor 2: Sex | −0.07 | 0.93 | 0.229 |
| Predictors on BMI z-Score | F (p) | R2 Adjusted | β | t (p) |
|---|---|---|---|---|
| PSE Total | 3.10 (0.01) | - | 0.21 | 35.44 (0.001) |
| Interaction PSE & Presence of a psychiatric diagnosis | 6.01 (0.001) | 0.262 | 0.40 | 6.01 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Rojo, M.; Solano, S.; Lacruz, T.; Baile, J.I.; Blanco, M.; Graell, M.; Sepúlveda, A.R. Linking Psychosocial Stress Events, Psychological Disorders and Childhood Obesity. Children 2021, 8, 211. https://0-doi-org.brum.beds.ac.uk/10.3390/children8030211
Rojo M, Solano S, Lacruz T, Baile JI, Blanco M, Graell M, Sepúlveda AR. Linking Psychosocial Stress Events, Psychological Disorders and Childhood Obesity. Children. 2021; 8(3):211. https://0-doi-org.brum.beds.ac.uk/10.3390/children8030211
Chicago/Turabian StyleRojo, Marta, Santos Solano, Tatiana Lacruz, José I. Baile, Miriam Blanco, Montserrat Graell, and Ana Rosa Sepúlveda. 2021. "Linking Psychosocial Stress Events, Psychological Disorders and Childhood Obesity" Children 8, no. 3: 211. https://0-doi-org.brum.beds.ac.uk/10.3390/children8030211