Dietary Patterns, Weight Perception and Obesity Status, among 10–12-Year-Old Children; an Epidemiological Study in Greece
Abstract
:1. Introduction
2. Materials and Methods
2.1. Design and Setting
2.2. Bioethics
2.3. Sample and Sampling Procedures
2.4. Statistical Power Analysis
2.5. Measurements
2.6. Children’s Weight Status Categorization
2.7. Assessment of Dietary Patterns
2.8. Assessment of Weight Perception
2.9. Statistical Analysis
3. Results
3.1. Prevalence of Overweight and Obesity
3.2. Weight Status Perception and Its Determinants
3.3. Dietary Pattern Analysis
3.4. Dietary Habits, Dietary Patterns, and Self-Perceived Agreement with Actual Weight Status
3.5. Dietary Patterns and Children’s Overweight/Obesity Status by Self-Perceived Agreement with Actual Weight Status
4. Discussion
Limitations
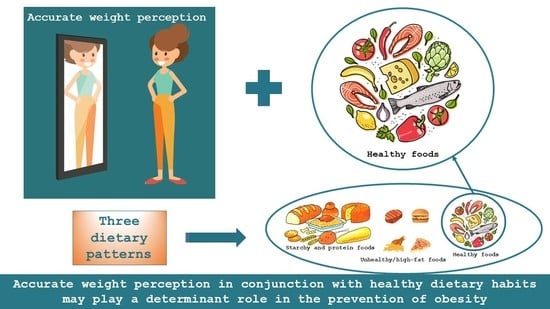
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Barroso, W.K.S.; Souza, A.L.L. Obesity, Overweight, Body Adiposity and Cardiovascular Risk in Children and Adolescents. Arq. Bras. Cardiol. 2020, 115, 172–173. [Google Scholar] [CrossRef]
- Kyle, T.K.; Dhurandhar, E.J.; Allison, D.B. Regarding obesity as a disease: Evolving policies and their implications. Endocrinol. Metab. Clin. North Am. 2016, 45, 511. [Google Scholar] [CrossRef] [Green Version]
- Bray, G.; Kim, K.; Wilding, J.; Federation, W.O. Obesity: A chronic relapsing progressive disease process. A position statement of the World Obesity Federation. Obes. Rev. 2017, 18, 715–723. [Google Scholar] [CrossRef] [Green Version]
- Kremers, S.P. Theory and practice in the study of influences on energy balance-related behaviors. Patient Educ. Couns. 2010, 79, 291–298. [Google Scholar] [CrossRef] [PubMed]
- Brug, J.; Lien, N.; Klepp, K.I.; van Lenthe, F.J. Exploring overweight, obesity and their behavioural correlates among children and adolescents: Results from the Health-promotion through Obesity Prevention across Europe project. Public Health Nutr. 2010, 13, 1676–1679. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Nelson, M.E.; Hamm, M.W.; Hu, F.B.; Abrams, S.A.; Griffin, T.S. Alignment of healthy dietary patterns and environmental sustainability: A systematic review. Adv. Nutr. 2016, 7, 1005–1025. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Panagiotakos, D.B.; Notara, V.; Kouvari, M.; Pitsavos, C. The Mediterranean and other dietary patterns in secondary cardiovascular disease prevention: A review. Curr. Vasc. Pharmacol. 2016, 14, 442–451. [Google Scholar] [CrossRef] [PubMed]
- Tapsell, L.C.; Neale, E.P.; Satija, A.; Hu, F.B. Foods, nutrients, and dietary patterns: Interconnections and implications for dietary guidelines. Adv. Nutr. 2016, 7, 445–454. [Google Scholar] [CrossRef]
- Gregory, C.O.; Blanck, H.M.; Gillespie, C.; Maynard, L.M.; Serdula, M.K. Health perceptions and demographic characteristics associated with underassessment of body weight. Obesity 2008, 16, 979–986. [Google Scholar] [CrossRef]
- Kim, K.H.c. Religion, weight perception, and weight control behavior. Eat. Behav. 2007, 8, 121–131. [Google Scholar] [CrossRef] [Green Version]
- Xie, B.; Liu, C.; Chou, C.p.; Xia, J.; Spruijt-Metz, D.; Gong, J.; Li, Y.; Wang, H.; Johnson, C.A. Weight perception and psychological factors in Chinese adolescents. J. Adolesc. Health 2003, 33, 202–210. [Google Scholar] [CrossRef]
- Buscemi, S.; Marventano, S.; Castellano, S.; Nolfo, F.; Rametta, S.; Giorgianni, G.; Matalone, M.; Marranzano, M.; Mistretta, A. Role of anthropometric factors, self-perception, and diet on weight misperception among young adolescents: A cross-sectional study. Eat. Weight Disord. 2018, 23, 107–115. [Google Scholar] [CrossRef]
- Mbogori, T.; Arthur, T.M. Perception of Body Weight Status Is Associated with the Health and Food Intake Behaviors of Adolescents in the United States. Am. J. Lifestyle Med. 2021, 15, 347–355. [Google Scholar] [CrossRef]
- Khambalia, A.; Hardy, L.L.; Bauman, A. Accuracy of weight perception, life-style behaviours and psychological distress among overweight and obese adolescents. J. Paediatr. Child Health 2012, 48, 220–227. [Google Scholar] [CrossRef] [PubMed]
- Brechan, I.; Kvalem, I.L. Relationship between body dissatisfaction and disordered eating: Mediating role of self-esteem and depression. Eat. Behav. 2015, 17, 49–58. [Google Scholar] [CrossRef]
- Fan, M.; Jin, Y. The effects of weight perception on adolescents’ weight-loss intentions and behaviors: Evidence from the youth risk behavior surveillance survey. Int. J. Environ. Res. Public Health 2015, 12, 14640–14668. [Google Scholar] [CrossRef] [Green Version]
- Fredrickson, J.; Kremer, P.; Swinburn, B.; de Silva, A.; McCabe, M. Weight perception in overweight adolescents: Associations with body change intentions, diet and physical activity. J. Health Psychol. 2015, 20, 774–784. [Google Scholar] [CrossRef] [PubMed]
- Goldschmidt, A.B.; Wall, M.M.; Loth, K.A.; Neumark-Sztainer, D. Risk factors for disordered eating in overweight adolescents and young adults. J. Pediatric Psychol. 2015, 40, 1048–1055. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tang, J.; Yu, Y.; Du, Y.; Ma, Y.; Zhu, H.; Liu, Z. Association between actual weight status, perceived weight and depressive, anxious symptoms in Chinese adolescents: A cross-sectional study. BMC Public Health 2010, 10, 594. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Klein, E.G.; Lytle, L.A.; Chen, V. Social ecological predictors of the transition to overweight in youth: Results from the Teens Eating for Energy and Nutrition at Schools (TEENS) study. J. Am. Diet. Assoc. 2008, 108, 1163–1169. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sutin, A.R.; Terracciano, A. Body weight misperception in adolescence and incident obesity in young adulthood. Psychol. Sci. 2015, 26, 507–511. [Google Scholar] [CrossRef] [PubMed]
- Edwards, N.M.; Pettingell, S.; Borowsky, I.W. Where perception meets reality: Self-perception of weight in overweight adolescents. Pediatrics 2010, 125, e452–e458. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Southerland, J.; Wang, L.; Richards, K.; Pack, R.; Slawson, D.L. On Academics Misperceptions of Overweight: Associations of Weight Misperception with Health-Related Quality of Life among Normal-Weight College Students. Public Health Rep. 2013, 128, 562–568. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Thunfors, P.; Hanlon, A.; Collins, B. Weight status misperception and the health behaviors of obese adolescents. Available online: https://print.ispub.com/api/0/ispub-article/11452 (accessed on 11 June 2021).
- Gaylis, J.B.; Levy, S.S.; Hong, M.Y. Relationships between body weight perception, body mass index, physical activity, and food choices in Southern California male and female adolescents. Int. J. Adolesc. Youth 2020, 25, 264–275. [Google Scholar] [CrossRef] [Green Version]
- Kanellopoulou, A.; Notara, V.; Antonogeorgos, G.; Chrissini, M.; Rojas-Gil, A.P.; Kornilaki, E.N.; Lagiou, A.; Panagiotakos, D.B. Inverse Association Between Health Literacy and Obesity Among Children in Greece: A School-Based, Cross-Sectional Epidemiological Study. Health Educ. Behav. 2021. [Google Scholar] [CrossRef]
- Antonogeogros, G.; Grigoropoulou, D.; Papadimitriou, A.; Priftis, K.; Anthracopoulos, M.; Nicolaidou, P.; Panagiotakos, D. Validation of a Food Frequency Questionnaire designed for children 10-12 years: The Panacea-FFQ. Pediatric Res. 2011, 70, 778. [Google Scholar] [CrossRef] [Green Version]
- Argiropoulou, E.C.; Michalopoulou, M.; Aggeloussis, N.; Avgerinos, A. Validity and reliability of physical activity measures in Greek high school age children. J. Sports Sci. Med. 2004, 3, 147. [Google Scholar]
- Cole, T.J.; Bellizzi, M.C.; Flegal, K.M.; Dietz, W.H. Establishing a standard definition for child overweight and obesity worldwide: International survey. BMJ 2000, 320, 1240. [Google Scholar] [CrossRef] [Green Version]
- Martin, M.A.; Frisco, M.L.; May, A.L. Gender and race/ethnic differences in inaccurate weight perceptions among US adolescents. Women’s Health Issues 2009, 19, 292–299. [Google Scholar] [CrossRef] [Green Version]
- Liberali, R.; Kupek, E.; Assis, M.A.A.d. Dietary patterns and childhood obesity risk: A systematic review. Child. Obes. 2020, 16, 70–85. [Google Scholar] [CrossRef]
- Cairns, G.; Angus, K.; Hastings, G.; Caraher, M. Systematic reviews of the evidence on the nature, extent and effects of food marketing to children. Retrosp. Summary. Appet. 2013, 62, 209–215. [Google Scholar] [CrossRef]
- Jackson, S.E.; Johnson, F.; Croker, H.; Wardle, J. Weight perceptions in a population sample of English adolescents: Cause for celebration or concern? Int. J. Obes. 2015, 39, 1488–1493. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Patte, K.A.; Laxer, R.; Qian, W.; Leatherdale, S.T. Weight perception and weight-control intention among youth in the COMPASS study. Am. J. Health Behav. 2016, 40, 614–623. [Google Scholar] [CrossRef] [PubMed]
- Aloufi, A.D.; Najman, J.M.; Al Mamun, A. Predictors of persistent body weight misclassification from adolescence period to adulthood: A longitudinal study. J. Epidemiol. Glob. Health 2019, 9, 116. [Google Scholar] [CrossRef] [Green Version]
- Dixey, R.; Sahota, P.; Atwal, S.; Turner, A. “Ha ha, you’ re fat, we’re strong”; A qualitative study of boys’ and girls’ perceptions of fatness, thinness, social pressures and health using focus groups. Health Educ. 2001. [Google Scholar] [CrossRef]
- Fredrickson, J.; Kremer, P.; Swinburn, B.; de Silva-Sanigorski, A.; McCabe, M. Biopsychosocial correlates of weight status perception in Australian adolescents. Body Image 2013, 10, 552–557. [Google Scholar] [CrossRef]
- Blanchet, R.; Kengneson, C.C.; Bodnaruc, A.M.; Gunter, A.; Giroux, I. Factors Influencing Parents’ and Children’s Misperception of Children’s Weight Status: A Systematic Review of Current Research. Curr. Obes. Rep. 2019, 8, 373–412. [Google Scholar] [CrossRef] [PubMed]
- Fan, M.; Jin, Y.; Khubchandani, J. Overweight misperception among adolescents in the United States. J. Pediatric Nurs. 2014, 29, 536–546. [Google Scholar] [CrossRef]
- Stephen, E.M.; Rose, J.S.; Kenney, L.; Rosselli-Navarra, F.; Weissman, R.S. Prevalence and correlates of unhealthy weight control behaviors: Findings from the national longitudinal study of adolescent health. J. Eat. Disord. 2014, 2, 16. [Google Scholar] [CrossRef] [Green Version]
- Deschamps, V.; Salanave, B.; Chan-Chee, C.; Vernay, M.; Castetbon, K. Body-weight perception and related preoccupations in a large national sample of adolescents. Pediatric Obes. 2015, 10, 15–22. [Google Scholar] [CrossRef]
- Haynes, A.; Kersbergen, I.; Sutin, A.; Daly, M.; Robinson, E. A systematic review of the relationship between weight status perceptions and weight loss attempts, strategies, behaviours and outcomes. Obes. Rev. 2018, 19, 347–363. [Google Scholar] [CrossRef]
- Roberts, R.E.; Duong, H.T. Perceived weight, not obesity, increases risk for major depression among adolescents. J. Psychiatr. Res. 2013, 47, 1110–1117. [Google Scholar] [CrossRef] [Green Version]
- Chung, A.E.; Perrin, E.M.; Skinner, A.C. Accuracy of child and adolescent weight perceptions and their relationships to dieting and exercise behaviors: A NHANES study. Acad. Pediatrics 2013, 13, 371–378. [Google Scholar] [CrossRef] [Green Version]
- Aller, E.E.; Abete, I.; Astrup, A.; Martinez, J.A.; Baak, M.A.v. Starches, sugars and obesity. Nutrients 2011, 3, 341–369. [Google Scholar] [CrossRef] [Green Version]
- Koletzko, B.; Demmelmair, H.; Grote, V.; Prell, C.; Weber, M. High protein intake in young children and increased weight gain and obesity risk. Am. J. Clin. Nutr. 2016, 103, 303–304. [Google Scholar] [CrossRef] [Green Version]
- Wilcox, G. Insulin and insulin resistance. Clin. Biochem. Rev. 2005, 26, 19. [Google Scholar] [PubMed]
- Knowles, G.; Ling, F.C.; Thomas, G.N.; Adab, P.; McManus, A.M. Body size dissatisfaction among young Chinese children in Hong Kong: A cross-sectional study. Public Health Nutr. 2015, 18, 1067–1074. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Pallan, M.J.; Hiam, L.C.; Duda, J.L.; Adab, P. Body image, body dissatisfaction and weight status in South Asian children: A cross-sectional study. BMC Public Health 2011, 9, 11–21. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Perrin, E.M.; Boone-Heinonen, J.; Field, A.E.; Coyne-Beasley, T.; Gordon-Larsen, P. Perception of overweight and self-esteem during adolescence. Int. J. Eat. Disord. 2010, 43, 447–454. [Google Scholar] [CrossRef]
- Patte, K.A.; Laxer, R.E.; Qian, W.; Leatherdale, S.T. An analysis of weight perception and physical activity and dietary behaviours among youth in the COMPASS study. SSM-Popul. Health 2016, 2, 841–849. [Google Scholar] [CrossRef] [Green Version]
- Jáuregui-Lobera, I.; Bolaños-Ríos, P.; Santiago-Fernández, M.J.; Garrido-Casals, O.; Sánchez, E. Perception of weight and psychological variables in a sample of Spanish adolescents. Diabetes Metab. Syndr. Obes. Targets Ther. 2011, 4, 245. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Robinson, E.; Hunger, J.; Daly, M. Perceived weight status and risk of weight gain across life in US and UK adults. Int. J. Obes. 2015, 39, 1721–1726. [Google Scholar] [CrossRef] [PubMed]


| Children’s Characteristics | Overall (n = 1700) | Normal Weight ** (n = 1233) | Overweight and Obese ** (n = 467) | p * |
|---|---|---|---|---|
| Age | 11.21 (0.79) | 11.23 (0.79) | 11.15 (0.78) | 0.058 |
| Gender (boys/girls) | ||||
| Boys | 781 (45.9%) | 528 (42.8%) | 253 (54.2%) | <0.001 |
| Girls | 919 (54.1%) | 705 (57.2%) | 214 (45.8%) | |
| Physical activity (yes) | 1243 (73.1%) | 923 (80.8%) | 320 (73.1%) | <0.001 |
| Children’s dietary habits (times/week), mean (SD) | ||||
| Dairy | 3.76 (1.65) | 3.77 (1.65) | 3.73 (1.65) | 0.623 |
| Soft drinks and Concentrated juices | 1.24 (1.56) | 1.19 (1.46) | 1.36 (1.80) | 0.079 |
| Fish | 0.67 (0.87) | 0.67 (0.84) | 0.66 (0.95) | 0.862 |
| Meat and products | 1.60 (1.27) | 1.57 (1.24) | 1.68 (1.35) | 0.102 |
| Legumes | 1.83 (1.68) | 1.84 (1.66) | 1.82 (1.75) | 0.812 |
| Starchy | 1.64 (1.09) | 1.62 (1.05) | 1.67 (1.16) | 0.421 |
| Ultra-processed food | 1.41 (1.63) | 1.36 (1.57) | 1.54 (1.77) | 0.050 |
| Vegetables | 2.06 (1.54) | 2.06 (1.50) | 2.07 (1.65) | 0.839 |
| Natural juices | 3.71 (2.69) | 3.79 (2.69) | 3.50 (2.69) | 0.050 |
| Fruits | 2.66 (1.69) | 2.67 (1.67) | 2.63 (1.75) | 0.740 |
| Bread | 2.17 (1.67) | 2.20 (1.69) | 2.10 (1.64) | 0.325 |
| Actual Body Weight Status (IOTF) | ||||||
|---|---|---|---|---|---|---|
| Underweight | Normal | Overweight/Obese | % Agreement | |||
| All children | Self-perceived body weight | Low weight | 77 (55.4%) | 344 (33.8%) | 126 (29.4%) | 52.5% |
| Normal | 61 (43.9%) | 609 (59.9%) | 157 (36.6%) | |||
| Overweight/Obese | 1 (0.7%) | 64 (6.3%) | 146 (34.0%) | |||
| Boys | Low weight | 29 (50.9%) | 160 (36.9%) | 69 (30.4%) | 50.3% | |
| Normal | 28 (49.1%) | 255 (58.8%) | 81 (35.7%) | |||
| Overweight/Obese | 0 (0.0%) | 19 (4.4%) | 77 (33.9%) | |||
| Girls | Low weight | 48 (58.5%) | 184 (31.6%) | 57 (28.2%) | 54.3% | |
| Normal | 33 (40.2%) | 354 (60.7%) | 76 (37.6%) | |||
| Overweight/Obese | 1 (1.2%) | 45 (7.7%) | 69 (34.2%) | |||
| Underestimation (n = 627) | Accuracy (n = 832) | Overestimation (n = 126) | p * | |
|---|---|---|---|---|
| Children’s dietary habits (times/week), mean (SD) | ||||
| Dairy | 3.93 (1.66) * | 3.71 (1.61) | 3.60 (1.82) | 0.025 |
| Soft drinks and Concentrated juices | 1.24 (1.44) | 1.25 (1.66) | 1.14 (1.25) | 0.762 |
| Fish | 0.74 (0.97) | 0.62 (0.81) | 0.64 (0.65) | 0.116 |
| Meat and products | 1.67 (1.32) * | 1.52 (1.18) | 1.81 (1.45) * | 0.014 |
| Legumes | 1.88 (1.70) | 1.75 (1.61) | 2.13 (1.97) * | 0.047 |
| Starchy | 1.69 (1.13) | 1.60 (1.08) | 1.65 (0.89) | 0.353 |
| Ultra-processed food | 1.38 (1.54) | 1.42 (1.67) | 1.33 (1.56) | 0.776 |
| Vegetables | 2.12 (1.62) | 1.99 (1.46) | 2.10 (1.47) | 0.307 |
| Natural juices | 3.75 (2.71) | 3.70 (2.68) | 3.69 (2.73) | 0.944 |
| Fruits | 2.56 (1.66) | 2.70 (1.71) | 2.91 (1.73) | 0.216 |
| Bread | 2.17 (1.69) | 2.16 (1.68) | 2.14 (1.55) | 0.982 |
| Children’s dietary patterns, mean factor score (SD) | ||||
| Starchy and protein food | 0.06 (1.05) * | −0.07 (0.94) | 0.12 (0.94) * | 0.013 |
| Unhealthy/high-fat foods | 0.01 (0.04) | 0.01 (1.06) | −0.08 (0.81) | 0.621 |
| Healthy foods | 0.04 (0.98) | −0.01 (1.01) | −0.05 (1.05) | 0.483 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kanellopoulou, A.; Kosti, R.I.; Notara, V.; Antonogeorgos, G.; Rojas-Gil, A.P.; Kornilaki, E.N.; Lagiou, A.; Yannakoulia, M.; Panagiotakos, D.B. Dietary Patterns, Weight Perception and Obesity Status, among 10–12-Year-Old Children; an Epidemiological Study in Greece. Children 2021, 8, 626. https://0-doi-org.brum.beds.ac.uk/10.3390/children8080626
Kanellopoulou A, Kosti RI, Notara V, Antonogeorgos G, Rojas-Gil AP, Kornilaki EN, Lagiou A, Yannakoulia M, Panagiotakos DB. Dietary Patterns, Weight Perception and Obesity Status, among 10–12-Year-Old Children; an Epidemiological Study in Greece. Children. 2021; 8(8):626. https://0-doi-org.brum.beds.ac.uk/10.3390/children8080626
Chicago/Turabian StyleKanellopoulou, Aikaterini, Rena I. Kosti, Venetia Notara, George Antonogeorgos, Andrea Paola Rojas-Gil, Ekaterina N. Kornilaki, Areti Lagiou, Mary Yannakoulia, and Demosthenes B. Panagiotakos. 2021. "Dietary Patterns, Weight Perception and Obesity Status, among 10–12-Year-Old Children; an Epidemiological Study in Greece" Children 8, no. 8: 626. https://0-doi-org.brum.beds.ac.uk/10.3390/children8080626