3D Guided Dental Implant Placement: Impact on Surgical Accuracy and Collateral Damage to the Inferior Alveolar Nerve
Abstract
:1. Introduction
2. Materials and Methods
2.1. Eligibility Criteria for the Selection of Cases
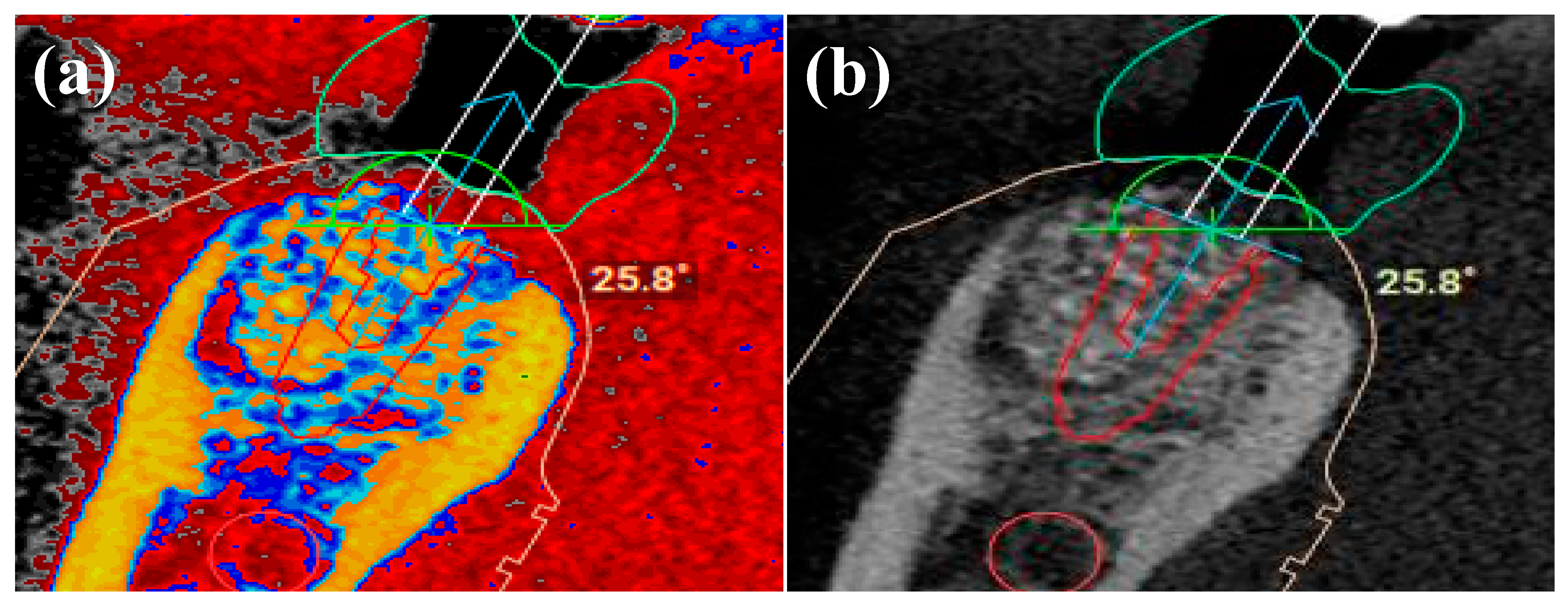
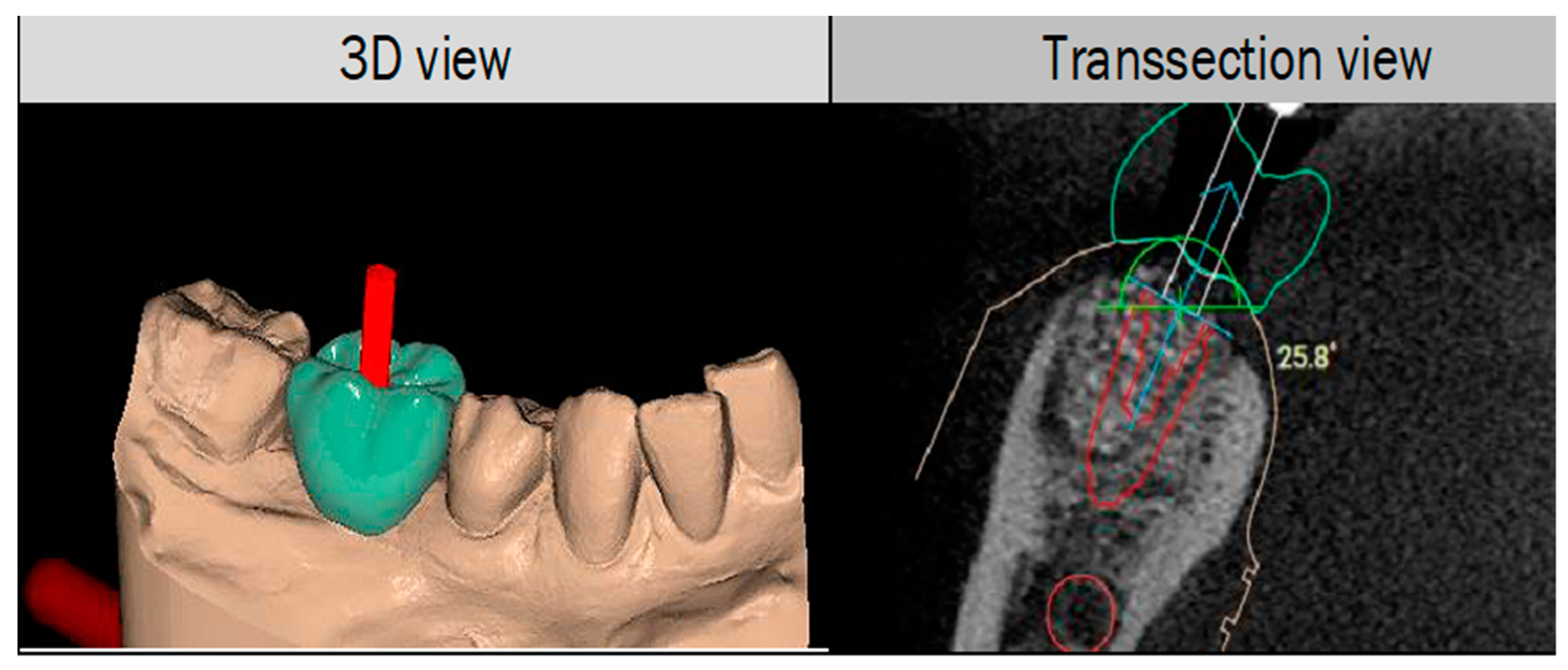
2.2. 3D Protocol Planning
2.3. In-Vitro Implant Placement
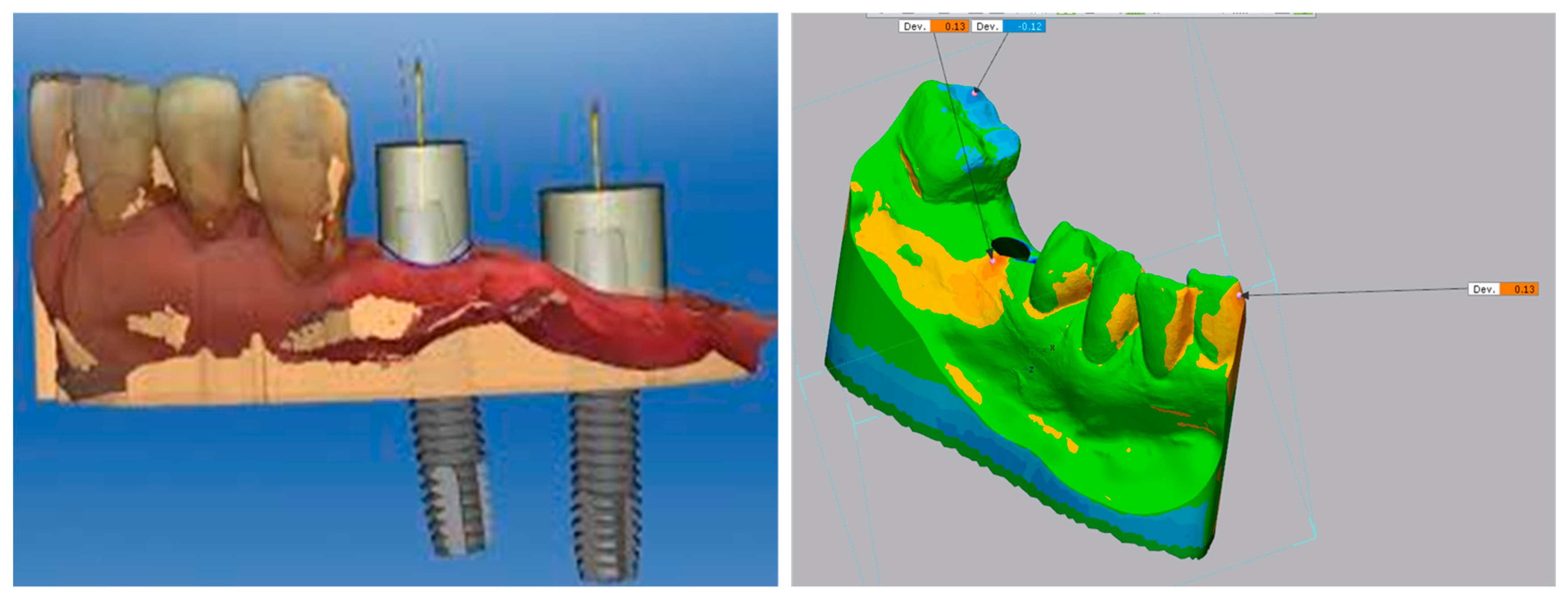
2.4. Digital Scanning of the Implants Using IOS
2.5. Scan Analysis Using EXOCAD®
2.6. Measurement of Deviations in Implant Position
2.7. Data Analysis
3. Results and Discussion
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Buser, D.; Arx, T. Surgical procedures in partially edentulous patients with ITI implants. Clin. Oral Implant. Res. 2000, 11, 83–100. [Google Scholar] [CrossRef]
- Renton, T. Prevention of Iatrogenic Inferior Alveolar Nerve Injuries in Relation to Dental Procedures. Dent. Update 2010, 37, 350–363. [Google Scholar] [CrossRef] [PubMed]
- Yilmaz, Z.; Ucer, C.; Scher, E.; Suzuki, J.; Renton, T. A Survey of the Opinion and Experience of UK Dentists. Implant. Dent. 2016, 25, 638–645. [Google Scholar] [CrossRef] [Green Version]
- Lin, C.-C.; Wu, C.-Z.; Huang, M.-S.; Huang, C.-F.; Cheng, H.-C.; Wang, D.P. Fully Digital Workflow for Planning Static Guided Implant Surgery: A Prospective Accuracy Study. J. Clin. Med. 2020, 9, 980. [Google Scholar] [CrossRef] [Green Version]
- De Angelis, P.; Manicone, P.F.; De De Angelis, S.; Grippaudo, C.; Gasparini, G.; Liguori, M.G.; Camodeca, F.; Piccirillo, G.B.; DeSantis, V.; D’Amato, G.; et al. Patient and Operator Centered Outcomes in Implant Dentistry: Comparison between Fully Digital and Conventional Workflow for Single Crown and Three-Unit Fixed-Bridge. Materials 2020, 13, 2781. [Google Scholar] [CrossRef]
- Walker-Finch, K.; Ucer, C. Five-year survival rates for implants placed using digitally-designed static surgical guides: A systematic review. Br. J. Oral Maxillofac. Surg. 2020, 58, 268–276. [Google Scholar] [CrossRef]
- Monje, A.; Insua, A.; Wang, H.-L. Understanding Peri-Implantitis as a Plaque-Associated and Site-Specific Entity: On the Local Predisposing Factors. J. Clin. Med. 2019, 8, 279. [Google Scholar] [CrossRef] [Green Version]
- Pauwels, R.; Jacobs, R.; Singer, S.; Mupparapu, M. CBCT-based bone quality assessment: Are Hounsfield units applicable? Dentomaxillofac. Radiol. 2015, 44, 20140238. [Google Scholar] [CrossRef] [Green Version]
- Beuer, F.; Schweiger, J.; Edelhoff, D. Digital dentistry: An overview of recent developments for CAD/CAM generated restorations. Br. Dent. J. 2008, 204, 505–511. [Google Scholar] [CrossRef]
- Van Noort, R. The future of dental devices is digital. Dent. Mater. 2012, 28, 3–12. [Google Scholar] [CrossRef]
- Greenstein, G.; Tarnow, D. The Mental Foramen and Nerve: Clinical and Anatomical Factors Related to Dental Implant Placement: A Literature Review. J. Periodontol. 2006, 77, 1933–1943. [Google Scholar] [CrossRef]
- Wareing, J.; Singh, N.; Jaffa, N.; Yankova, Z.; Cox, B.; McCaul, J. The role of CBCT in OMFS practice. Br. J. Oral Maxillofac. Surg. 2016, 54, e93–e94. [Google Scholar] [CrossRef]
- NowakA, R.; ZawiślakB, E.; BatyckiB, J. Factors affecting for the injury of lingual and inferior alveolar nerve during third lower molar surgery in the mandible. Dent. Med. Probl. 2014, 51, 225–230. [Google Scholar]
- Eggert, F.-M.; Levin, L. Biology of teeth and implants: The external environment, biology of structures, and clinical aspects. Quintessence Int. 2018, 49, 301–312. [Google Scholar]
- McAllister, P.; Watson, M.; Burke, E. A Cost-Effective, In-House, Positioning and Cutting Guide System for Orthognathic Surgery. J. Maxillofac. Oral Surg. 2017, 17, 112–114. [Google Scholar] [CrossRef] [PubMed]
- Parnia, F.; Yazdani, J.; Javaherzadeh, V.; Dizaj, S.M. Overview of Nanoparticle Coating of Dental Implants for Enhanced Osseointegration and Antimicrobial Purposes. J. Pharm. Pharm. Sci. 2017, 20, 148–160. [Google Scholar] [CrossRef]
- Tarnow, D.; Cho, S.-C.; Wallace, S. The Effect of Inter-Implant Distance on the Height of Inter-Implant Bone Crest. J. Periodontol. 2000, 71, 546–549. [Google Scholar] [CrossRef] [Green Version]
- Grunder, U.; Gracis, S.; Capelli, M. Influence of the 3-D bone-to-implant relationship on esthetics. Int. J. Periodontics Restor. Dent. 2005, 25, 113–119. [Google Scholar]
- Burke, R.; Richardsen, A. Increasing Occupational Health and Safety in Workplaces. In Increasing Occupational Health and Safety in Workplaces; Edward Elgar Publishing: Cheltenham, UK, 2019. [Google Scholar] [CrossRef]
- Smitkarn, P.; Subbalekha, K.; Mattheos, N.; Pimkhaokham, A. The accuracy of single-tooth implants placed using fully digital-guided surgery and freehand implant surgery. J. Clin. Periodontol. 2019, 46, 949–957. [Google Scholar] [CrossRef]
- Jacobs, R.; Salmon, B.; Codari, M.; Hassan, B.; Bornstein, M.M. Cone beam computed tomography in implant dentistry: Recommendations for clinical use. BMC Oral Health 2018, 18, 1–16. [Google Scholar] [CrossRef] [Green Version]
- Jang, D.; Son, K.; Lee, K.-B. A Comparative Study of the Fitness and Trueness of a Three-Unit Fixed Dental Prosthesis Fabricated Using Two Digital Workflows. Appl. Sci. 2019, 9, 2778. [Google Scholar] [CrossRef] [Green Version]
- Kim, S.-M.; Son, K.; Kim, D.-Y.; Lee, K.-B. Digital Evaluation of the Accuracy of Computer-Guided Dental Implant Placement: An In Vitro Study. Appl. Sci. 2019, 9, 3373. [Google Scholar] [CrossRef] [Green Version]
- Huang, L.; Zhang, X.; Mo, A. A Retrospective Study on the Transferring Accuracy of a Fully Guided Digital Template in the Anterior Zone. Materials 2021, 14, 4631. [Google Scholar] [CrossRef]
- Kühl, S.; Zürcher, S.; Mahid, T.; Müller-Gerbl, M.; Filippi, A.; Cattin, P. Accuracy of full guided vs. half-guided implant surgery. Clin. Oral Implant. Res. 2012, 24. [Google Scholar] [CrossRef] [PubMed]
- Scherer, U.; Stoetzer, M.; Ruecker, M.; Gellrich, N.-C.; Von See, C. Template-guided vs. non-guided drilling in site preparation of dental implants. Clin. Oral Investig. 2015, 19, 1339–1346. [Google Scholar] [CrossRef]
- Gluckman, H.; Du Toit, J.; Salama, M. Guided bone regeneration of a fenestration complication at immediate implant placement simultaneous to the socket-shield technique. Int. Dent. 2015, 5, 58–66. [Google Scholar]
- Davidowitz, G.; Kotick, P.G. The Use of CAD/CAM in Dentistry. Dent. Clin. N. Am. 2011, 55, 559–570. [Google Scholar] [CrossRef] [PubMed]
- Tahmaseb, A.; Wu, V.; Wismeijer, D.; Coucke, W.; Evans, C. The accuracy of static computer-aided implant surgery: A systematic review and meta-analysis. Clin. Oral Implant. Res. 2018, 29, 416–435. [Google Scholar] [CrossRef] [Green Version]
- Fürhauser, R.; Mailath-Pokorny, G.; Haas, R.; Busenlechner, D.; Watzek, G.; Pommer, B. Esthetics of Flapless Single-Tooth Implants in the Anterior Maxilla Using Guided Surgery: Association of Three-Dimensional Accuracy and Pink Esthetic Score. Clin. Implant. Dent. Relat. Res. 2015, 17, e427–e433. [Google Scholar] [CrossRef]
- Schnutenhaus, S.; Edelmann, C.; Rudolph, H.; Luthardt, R.G. Retrospective study to determine the accuracy of template-guided implant placement using a novel nonradiologic evaluation method. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. 2016, 121, e72–e79. [Google Scholar] [CrossRef]
- Vercruyssen, M.; Coucke, W.; Naert, I.; Jacobs, R.; Teughels, W.; Quirynen, M. Depth and lateral deviations in guided implant surgery: An RCT comparing guided surgery with mental navigation or the use of a pilot-drill template. Clin. Oral Implant. Res. 2014, 26, 1315–1320. [Google Scholar] [CrossRef]
- Younes, F.; Cosyn, J.; De Bruyckere, T.; Cleymaet, R.; Bouckaert, E.; Eghbali, A. A randomized controlled study on the accuracy of free-handed, pilot-drill guided and fully guided implant surgery in partially edentulous patients. J. Clin. Periodontol. 2018, 45, 721–732. [Google Scholar] [CrossRef]
- Baab, D.A.; Ammons, W.F.; Selipsky, H. Blood Loss During Periodontal Flap Surgery. J. Periodontol. 1977, 48, 693–698. [Google Scholar] [CrossRef]
- Vasconcelos, J.D.A.; Avila, G.B.; Ribeiro, J.C.; Dias, S.C.; Pereira, L.J. Inferior alveolar nerve transposition with involvement of the mental foramen for implant placement. Med. Oral Patol. Oral Y Cir. Bucal 2008, 13, 722–725. [Google Scholar]
- Garcés, M.A.S.; Escoda-Francolí, J.; Gay-Escoda, C. Implant Complications. In Implant Dentistry—The Most Promising Discipline of Dentistry; IntechOpen: London, UK, 2011. [Google Scholar] [CrossRef] [Green Version]
- Hegedus, F.; Diecidue, R.J. Trigeminal nerve injuries after mandibular implant placement—Practical knowledge for clinicians. Int. J. Oral Maxillofac. Implant. 2006, 21, 111–116. [Google Scholar]
- Vercruyssen, M.; Laleman, I.; Jacobs, R.; Quirynen, M. Computer-supported implant planning and guided surgery: A narrative review. Clin. Oral Implant. Res. 2015, 26, 69–76. [Google Scholar] [CrossRef]
- Misch, C.E.; Resnik, R. Mandibular Nerve Neurosensory Impairment After Dental Implant Surgery: Management and Protocol. Implant. Dent. 2010, 19, 378–386. [Google Scholar] [CrossRef]

| Case Number | Selected Cases Description |
|---|---|
| Case 1 | Missing LR first molar, bound saddle, socket preservation, IAN inferior |
| Case 2 | Missing LR first molar, bound saddle, socket preservation, IAN inferolateral |
| Case 3 | Missing LR first molar, socket preservation, IAN inferior |
| Case 4 | Missing LL second molar, socket preservation, IAN inferior, LL first molar also missing, larger guide span between bound saddles |
| Case 5 | Missing LR first molar, bound saddle, socket preservation, IAN inferolateral, laterally inclined lingual bone |
| Case 6 | Missing LL first molar, bound saddle, socket preservation, no lingual fossa, IAN inferolateral, and close to the planned position |
| Free Hand | Planned Distance to IAN (mm) | Distance to IAN (mm) | Deviation (mm) | Coronal Deviation (mm) | Apical Deviation (mm) | Angular Deviation (°) |
|---|---|---|---|---|---|---|
| 1 | 3.21 | 4.28 | +1.07 | 1.00 | 2.02 | 8.00 |
| 2 | 2.50 | 2.79 | +0.29 | 0.87 | 2.17 | 9.12 |
| 3 | 6.29 | 7.91 | +1.62 | 1.88 | 2.03 | 1.99 |
| 4 | 4.70 | 4.93 | +0.23 | 0.70 | 0.93 | 4.88 |
| 5 | 4.18 | 6.73 | +2.55 | 1.69 | 3.38 | 11.78 |
| 6 | 1.29 | 1.22 | −0.07 | 0.44 | 0.78 | 2.82 |
| Mean | 3.70 ± 1.76 | 4.64 ± 2.47 | 0.95 ± 1.00 | 1.10 ± 0.57 | 1.88 ± 0.95 | 6.43 ± 3.82 |
| Fully Guided | Planned Distance to IAN (mm) | Distance to IAN (mm) | Deviation (mm) | Coronal Deviation (mm) | Apical Deviation (mm) | Angular Deviation (°) |
|---|---|---|---|---|---|---|
| 1 | 3.21 | 2.96 | −0.25 | 0.43 | 0.53 | 0.97 |
| 2 | 2.50 | 3.13 | + 0.63 | 0.79 | 0.92 | 0.98 |
| 3 | 6.29 | 6.33 | + 0.04 | 0.14 | 0.14 | 0.16 |
| 4 | 4.70 | 4.80 | + 0.10 | 0.22 | 0.22 | 0.95 |
| 5 | 4.18 | 4.35 | + 0.17 | 0.21 | 0.21 | 0.97 |
| 6 | 1.29 | 1.08 | −0.21 | 0.29 | 0.29 | 0.69 |
| Mean | 3.70 ± 1.76 | 3.78 ± 1.80 | 0.08 ± 0.32 | 0.35 ± 0.24 | 0.43 ± 0.27 | 0.78 ± 0.33 |
| Mean Deviation from Planned Position | ||
|---|---|---|
| Study | Free-Hand | Guided |
| Fürhauser et al. (2015) [30] | - | Entry 0.8 mm Apex 1.2 mm Angle 2.7° |
| Schnutenhaus et al. (2016) [31] | - | Entry 1.0 mm Apex 1.6 mm Angle 5.0° |
| Tahmaseb et al. (2018) [29] | - | Entry 0.9 mm Apex 1.2 mm Angle 3.3° |
| Vercruyssen et al. (2015) [32] | Entry 2.8 mm Apex 3.1 mm Angle 9.1° | Entry 1.4 mm Apex 1.6 mm Angle 3.0° |
| Younes et al. (2018) [33] | Entry 1.5 mm Apex 2.1 mm Angle 7.0° | Entry 0.7 mm Apex 1.0 mm Angle 2.3° |
| Mistry et al. (2021) | Entry 1.1 mm Apex 1.9 mm Angle 6.4° | Entry 0.4 mm Apex 0.4 mm Angle 0.8° |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mistry, A.; Ucer, C.; Thompson, J.D.; Khan, R.S.; Karahmet, E.; Sher, F. 3D Guided Dental Implant Placement: Impact on Surgical Accuracy and Collateral Damage to the Inferior Alveolar Nerve. Dent. J. 2021, 9, 99. https://0-doi-org.brum.beds.ac.uk/10.3390/dj9090099
Mistry A, Ucer C, Thompson JD, Khan RS, Karahmet E, Sher F. 3D Guided Dental Implant Placement: Impact on Surgical Accuracy and Collateral Damage to the Inferior Alveolar Nerve. Dentistry Journal. 2021; 9(9):99. https://0-doi-org.brum.beds.ac.uk/10.3390/dj9090099
Chicago/Turabian StyleMistry, Amit, Cemal Ucer, John D. Thompson, Rabia Sannam Khan, Emina Karahmet, and Farooq Sher. 2021. "3D Guided Dental Implant Placement: Impact on Surgical Accuracy and Collateral Damage to the Inferior Alveolar Nerve" Dentistry Journal 9, no. 9: 99. https://0-doi-org.brum.beds.ac.uk/10.3390/dj9090099






