Overview of Self-Management Skills and Associated Assessment Tools for Children with Inflammatory Bowel Disease
Abstract
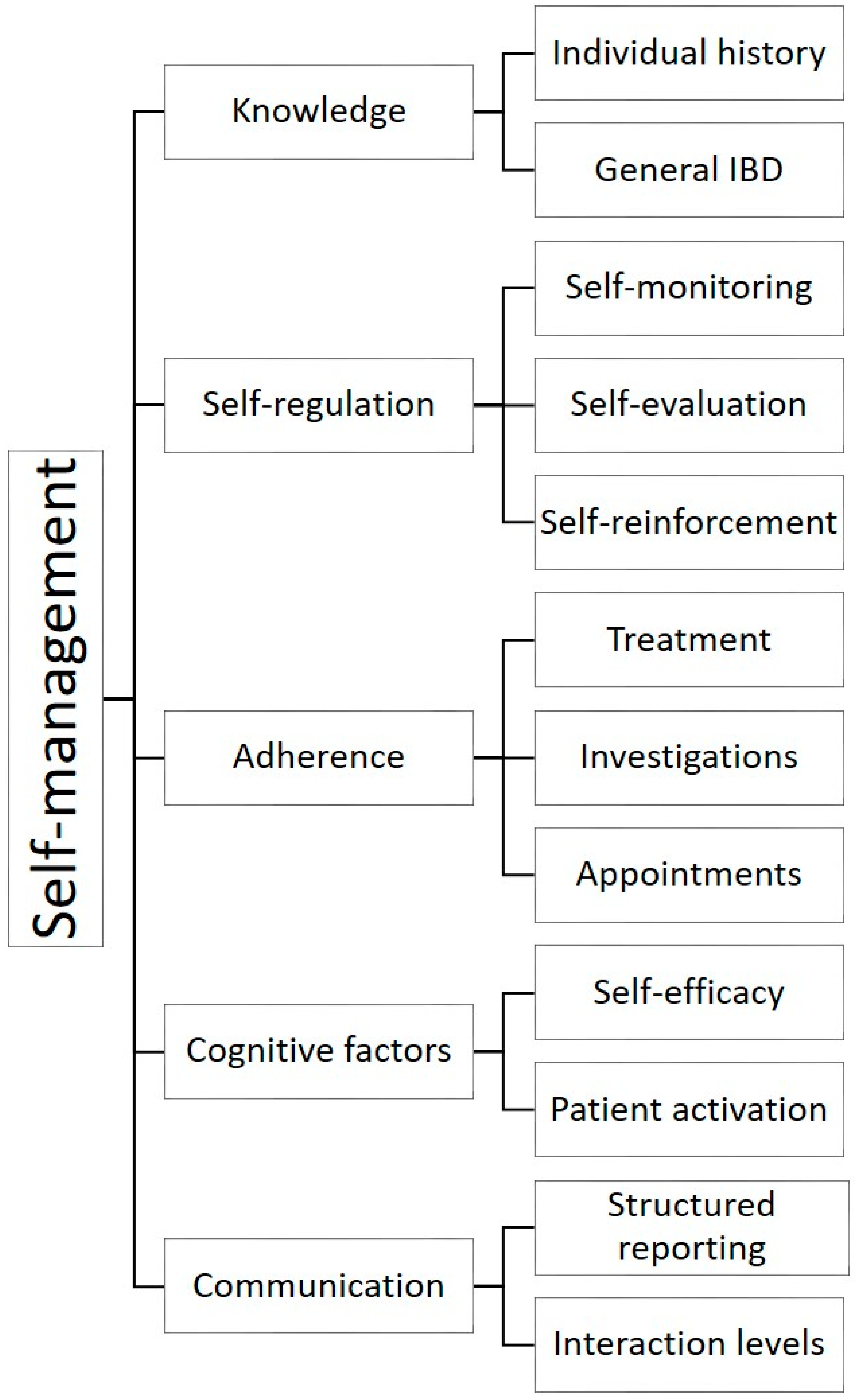
:1. Introduction
- Disease and treatment knowledge
- Self-regulation
- Adherence
- Communication
- Cognitive attributes
2. Self-Management Factors
2.1. Disease and Treatment Knowledge
- Individual IBD knowledge; diagnosis, disease location and extent, surgical history, medication history
- General IBD knowledge
- Disease monitoring procedures and investigations
- Preventive health
Knowledge Outcome Measures
2.2. Self-Regulation
2.2.1. Symptom Self-Monitoring
2.2.2. Self-Evaluation
2.2.3. Self-Reinforcement
2.2.4. Self-Regulation Outcome Measures
2.3. Adherence
2.3.1. Adherence and IBD Outcomes
2.3.2. Adherence Outcome Measures
- Patient or parent reports using interviews may be time consuming and subjective, and may overestimate adherence by up to 23% in adolescents with IBD when compared to objective measures [74,94,96,97,98]. The Medication Adherence Measure is a validated semi-structured interview that is widely used in pediatrics, and a correction factor for child and parent self-report data has been produced that should provide more accurate adherence rates from subjective reports [99].
- Daily adherence diaries are not validated and have a poor history of compliance, however, measuring the more universal concept of daily activities, incorporating medication taking, have better completion rates [97].
- Electronic medication monitoring devices can be used to track adherence to oral and inhaled drug regimens, thus providing objective, specific real time information on adherence [99]. This long-term monitoring method can reveal a spectrum of dosing problems, however, it relies on presumptive data on ingestion, is costly and prone to malfunctions [97,101].
- Pill counts involve totaling tablets (or liquid quantities) at two time intervals and comparing what is expected from the prescribed dosing regimen [70]. While this method is simple, feasible, and objective, it is also prone to inaccuracy and measures removal of the drugs from the container, not actual ingestion [70].
- Validated adherence scales are structured surveys that ask specific questions regarding adherence, with responses often measured using a Likert scale. None have been developed for children yet, but the most commonly used scale with adults is the Morisky scale [102], which has also been adapted for use with adults with IBD [103]. However, this scale measures barriers to adherence instead of nonadherence frequency, and may overestimate or undervalue adherence as items only account for daily medication regimens [98].
- A simple adherence visual analogue scale (VAS) provides a self-report method that is extremely quick to comprehend and complete. Studies comparing the Morisky scale to a simple VAS showed the VAS provides a more objective measure to quantify adherence [98].
- Pharmacy records regarding refill rates and the proportion of days covered by a filled prescription provide practical data on refill behaviors believed to correspond to medication taking. However, they do not directly estimate adherence and once again assume ingestion [31].
- The pediatric IBD disease activity indices (PUCAI and PCDAI) are frequently incorporated into adherence studies as a way of correlating symptoms with measured adherence.
2.4. Cognitive Attributes
2.4.1. Patient Activation
2.4.2. Self-Efficacy
2.4.3. Cognitive Attribute Outcome Measures
Patient Activation
Self-Efficacy
2.5. Communication
Communication Outcome Measures
2.6. Self-Management Skills
Self-Management Outcome Measures
3. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Sauer, C.G.; Kugathasan, S. Pediatric Inflammatory Bowel Disease: Highlighting Pediatric Differences in IBD. Med. Clin. N. Am. 2010, 94, 35–52. [Google Scholar] [CrossRef] [PubMed]
- Benchimol, E.I.; Fortinsky, K.J.; Gozdyra, P.; Van den Heuvel, M.; Van Limbergen, J.; Griffiths, A.M. Epidemiology of pediatric inflammatory bowel disease: A systematic review of international trends. Inflamm. Bowel Dis. 2011, 17, 423–439. [Google Scholar] [CrossRef]
- Sykora, J.; Pomahacova, R.; Kreslova, M.; Cvalinova, D.; Stych, P.; Schwarz, J. Current global trends in the incidence of pediatric-onset inflammatory bowel disease. World J. Gastroenterol. 2018, 24, 2741–2763. [Google Scholar] [CrossRef] [PubMed]
- Benchimol, E.I.; Walters, T.D.; Kaufman, M.; Frost, K.; Fiedler, K.; Chinea, Z.; Zachos, M. Assessment of knowledge in adolescents with inflammatory bowel disease using a novel transition tool. Inflamm. Bowel Dis. 2011, 17, 1131–1137. [Google Scholar] [CrossRef] [PubMed]
- Hait, E.; Arnold, J.H.; Fishman, L.N. Educate, communicate, anticipate-practical recommendations for transitioning adolescents with IBD to adult health care. Inflamm. Bowel Dis. 2006, 12, 70–73. [Google Scholar] [CrossRef]
- Oliveira, S.B.; Monteiro, I.M. Diagnosis and management of inflammatory bowel disease in children. BMJ 2017, 357, j2083. [Google Scholar] [CrossRef]
- Izaguirre, R.M.; Keefer, R.L. Development of a Self-Efficacy Scale for Adolescents and Young Adults With Inflammatory Bowel Disease. J. Pediatr. Gastroenterol. Nutr. 2014, 59, 29–32. [Google Scholar] [CrossRef] [PubMed]
- Ruemmele, F.M.; Veres, G.; Kolho, K.L.; Griffiths, A.; Levine, A.; Escher, J.C.; Amil Dias, J.; Barabino, A.; Braegger, C.P.; Bronsky, J.; et al. Consensus guidelines of ECCO/ESPGHAN on the medical management of pediatric Crohn’s disease. J. Crohn’s Colitis 2014, 8, 1179–1207. [Google Scholar] [CrossRef] [Green Version]
- Day, A.S.; Ledder, O.; Leach, S.T.; Lemberg, D.A. Crohn’s and colitis in children and adolescents. World J. Gastroenterol. 2012, 18, 5862–5869. [Google Scholar] [CrossRef]
- Modi, A.C.; Pai, A.L.; Hommel, K.A.; Hood, K.K.; Cortina, S.; Hilliard, M.E.; Guilfoyle, S.M.; Gray, W.N.; Drotar, D. Pediatric self-management: A framework for research, practice, and policy. Pediatrics 2012, 129, e473–e485. [Google Scholar] [CrossRef] [Green Version]
- Gray, W.N.; Denson, L.A.; Baldassano, R.N.; Hommel, K.A. Treatment Adherence in Adolescents with Inflammatory Bowel Disease: The Collective Impact of Barriers to Adherence and Anxiety/Depressive Symptoms. J. Paediatr. Psychol. 2012, 37, 282–291. [Google Scholar] [CrossRef]
- Schwartz, L.A.; Tuchman, L.K.; Hobbie, W.L.; Ginsberg, J.P. A social-ecological model of readiness for transition to adult-oriented care for adolescents and young adults with chronic health conditions. Child Care Health Dev. 2011, 37, 883–895. [Google Scholar] [CrossRef]
- Beacham, B.L.; Deatrick, J.A. Health Care Autonomy in Children with Chronic Conditions: Implications for Self-Care and Family Management. Nurs. Clin. N. Am. 2013, 48, 305–317. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Guevara, J.P.; Wolf, F.M.; Grum, C.M.; Clark, N.M. Effects of educational interventions for self management of asthma in children and adolescents: Systematic review and meta-analysis. BMJ 2003, 326, 1308–1309. [Google Scholar] [CrossRef] [Green Version]
- Kirk, S.; Beatty, S.; Callery, P.; Gellatly, J.; Milnes, L.; Pryjmachuk, S. The effectiveness of self-care support interventions for children and young people with long-term conditions: A systematic review. Child Care Health Dev. 2013, 39, 305–324. [Google Scholar] [CrossRef]
- Robinson, A.; Thompson, D.G.; Wilkin, D.; Roberts, C. Guided self-management and patient-directed follow-up of ulcerative colitis: A randomised trial. Lancet 2001, 358, 976–981. [Google Scholar] [CrossRef]
- Keefer, L.; Kiebles, J.L.; Martinovich, Z.; Cohen, E.; Van Denburg, A.; Barrett, T.A. Behavioral interventions may prolong remission in patients with inflammatory bowel disease. Behav. Res. Ther. 2011, 49, 145–150. [Google Scholar] [CrossRef] [Green Version]
- Kennedy, A.; Nelson, E.; Reeves, D.; Richardson, G.; Roberts, C.; Robinson, A.; Rogers, A.; Sculpher, M.; Thompson, D. A randomised controlled trial to assess the impact of a package comprising a patient-orientated, evidence-based self-help guidebook and patient-centred consultations on disease management and satisfaction in inflammatory bowel disease. Health Technol. Assess. 2003, 7. [Google Scholar] [CrossRef]
- Squires, S.I.; Boal, A.J.; Lamont, S.; Naismith, G.D. Implementing a self-management strategy in inflammatory bowel disease (IBD): Patient perceptions, clinical outcomes and the impact on service. Front. Gastroenterol. 2017, 8, 272–278. [Google Scholar] [CrossRef] [PubMed]
- Hueppe, A.; Langbrandtner, J.; Raspe, H. Inviting Patients with Inflammatory Bowel Disease to Active Involvement in Their Own Care: A Randomized Controlled Trial. Inflamm. Bowel Dis. 2014, 20, 1057–1069. [Google Scholar] [CrossRef] [PubMed]
- Henry, H.K.; Schor, E.L. Supporting self-management of chronic health problems. Pediatrics 2015, 135, 789–792. [Google Scholar] [CrossRef] [Green Version]
- Lesch, W.; Specht, K.; Lux, A.; Frey, M.; Utens, E.; Bauer, U. Disease-specific knowledge and information preferences of young patients with congenital heart disease. Cardiol. Young 2014, 24, 321–330. [Google Scholar] [CrossRef]
- Sattoe, J.N.T.; Bal, M.I.; Roelofs, P.; Bal, R.; Miedema, H.S.; van Staa, A. Self-management interventions for young people with chronic conditions: A systematic overview. Patient Educ. Couns. 2015, 98, 704–715. [Google Scholar] [CrossRef] [Green Version]
- Trivedi, I.; Keefer, L. The Emerging Adult with Inflammatory Bowel Disease: Challenges and Recommendations for the Adult Gastroenterologist. Gastroenterol. Res. Pract. 2015, 2015, 11. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Eaden, J.A.; Abrams, K.; Mayberry, J.F. The Crohn’s and Colitis Knowledge Score: A test for measuring patient knowledge in inflammatory bowel disease. Am. J. Gastroenterol. 1999, 94, 3560–3566. [Google Scholar] [CrossRef] [PubMed]
- Haaland, D.; Day, A.S.; Otley, A. Development and validation of a pediatric IBD knowledge inventory device: The IBD-KID. J. Pediatr. Gastroenterol. Nutr. 2014, 58, 313–319. [Google Scholar] [CrossRef]
- Lozano, P.; Houtrow, A. Supporting Self-Management in Children and Adolescents with Complex Chronic Conditions. Pediatrics 2018, 141, S233–S241. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Eltorai, A.; Ghanian, S.; Adams, C.; Born, C.; Daniels, A. Readability of Patient Education Materials on the American Association for Surgery of Trauma Website. Arch. Trauma Res. 2014, 3. [Google Scholar] [CrossRef] [Green Version]
- Swartz, E. The readability of paediatric patient information materials: Are families satisfied with our handouts and brochures? Paediatr. Child Health 2010, 15, 509. [Google Scholar] [CrossRef] [Green Version]
- Doak, L.; Doak, C. Writing for readers with a wide range of reading skills. Am. Med. Writ. Assoc. J. 2010, 25, 149. [Google Scholar]
- Hommel, K.A.; Greenley, R.N.; Maddux, M.H.; Gray, W.N.; Mackner, L.M. Self-management in pediatric inflammatory bowel disease: A clinical report of the North American Society for Pediatric Gastroenterology, Hepatology, and Nutrition. J. Pediatr. Gastroenterol. Nutr. 2013, 57, 250–257. [Google Scholar] [CrossRef] [Green Version]
- Fishman, L.N.; Barendse, R.M.; Hait, E.; Burdick, C.; Arnold, J. Self-management of older adolescents with inflammatory bowel disease: A pilot study of behavior and knowledge as prelude to transition. Clin. Pediatr. 2010, 49, 1129–1133. [Google Scholar] [CrossRef] [PubMed]
- Fishman, L.N.; Houtman, D.; van Groningen, J.; Arnold, J.; Ziniel, S. Medication knowledge: An initial step in self-management for youth with inflammatory bowel disease. J. Pediatr. Gastroenterol. Nutr. 2011, 53, 641–645. [Google Scholar] [CrossRef] [PubMed]
- Van Rheenen, P.; Aloi, M.; Biron, I.; Carlsen, K.; Cooney, R.; Cucchiara, S.; Cullen, G.; Escher, J.; Kierkus, J.; Lindsay, J.; et al. European Crohn’s and Colitis Organisation Topical Review on Transitional Care in Inflammatory Bowel Disease. J. Crohn’s Colitis 2017, 11, 1032–1038. [Google Scholar] [CrossRef] [PubMed]
- Gumidyala, P.A.; Plevinsky, M.J.; Poulopoulos, A.N.; Kahn, N.S.; Walkiewicz, N.D.; Greenley, N.R. What Teens Do Not Know Can Hurt Them: An Assessment of Disease Knowledge in Adolescents and Young Adults with IBD. Inflamm. Bowel Dis. 2017, 23, 89–96. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hait, E.J.; Barendse, R.M.; Arnold, J.H.; Valim, C.; Sands, B.E.; Korzenik, J.R.; Fishman, L.N. Transition of adolescents with inflammatory bowel disease from pediatric to adult care: A survey of adult gastroenterologists. J. Pediatr. Gastroenterol. Nutr. 2009, 48, 61–65. [Google Scholar] [CrossRef] [PubMed]
- Schulman-Green, D.; Jaser, S.S.; Park, C.; Whittemore, R. A metasynthesis of factors affecting self-management of chronic illness. J. Adv. Nurs. 2016, 72, 1469–1489. [Google Scholar] [CrossRef]
- Tung, J.; Grunow, J.E.; Jacobs, N. Pilot Development of an Electronic Pediatric Inflammatory Bowel Disease Quiz Game. J. Pediatr. Gastroenterol. Nutr. 2015, 61, 292–296. [Google Scholar] [CrossRef]
- Day, A.S.; Mylvaganam, G.; Shalloo, N.; Clarkson, C.; Leach, S.T.; Lemberg, D.A. Assessment of disease-specific knowledge in Australian children with inflammatory bowel disease and their parents. J. Paediatr. Child Health 2017, 53, 778. [Google Scholar] [CrossRef]
- Day, A.S.; Lemberg, D.A.; Nichol, A.; Clarkson, C.; Otley, A.R. Generalisability of the inflammatory bowel disease knowledge inventory device to assess disease-related knowledge in Australian children. J. Paediatr. Child Health 2014, 50, 591–595. [Google Scholar] [CrossRef]
- Vernon-Roberts, A.; Otley, A.; Frampton, C.; Gearry, R.B.; Day, A.S. Validation of a Revised Knowledge Assessment Tool for Children with Inflammatory Bowel Disease (IBD-KID2). Inflamm. Intest. Dis. 2020, 5, 70–77. [Google Scholar] [CrossRef]
- Baars, J.E.; Siegel, C.A.; Van’t Spijker, A.; Markus, T.; Kuipers, E.J.; van der Woude, C.J. Inflammatory bowel disease-patients are insufficiently educated about the basic characteristics of their disease and the associated risk of colorectal cancer. Dig. Liver Dis. 2010, 42, 777–784. [Google Scholar] [CrossRef]
- O’Sullivan, M.; O’Morain, C. Patient knowledge in inflammatory bowel disease. Am. J. Gastroenterol. 2000, 95, 2128–2129. [Google Scholar] [CrossRef]
- Jones, S.C.; Gallacher, B.; Lobo, A.J.; Axon, A.T. A patient knowledge questionnaire in inflammatory bowel disease. J. Clin. Gastroenterol. 1993, 17, 21–24. [Google Scholar] [CrossRef]
- Yoon, H.; Yang, S.-K.; So, H.; Lee, K.E.; Park, S.H.; Jung, S.-A.; Choh, J.H.; Shin, C.M.; Park, Y.S.; Kim, N.; et al. Development, validation, and application of a novel tool to measure disease-related knowledge in patients with inflammatory bowel disease. Korean J. Intern Med. 2019, 34, 81–89. [Google Scholar] [CrossRef] [PubMed]
- Casellas, F.; Navarro, E.; Amil, P.; Barber, C.; Marin, L.; Guardiola, J.; Espin, E.; Sainz, E.; Aldeguer, X.; Gallego, M.; et al. Development and validation of the QUECOMIICAT questionnaire: A tool to assess disease-related knowledge in patients with inflammatory bowel disease. Rev. Esp. Enferm Dig. 2019, 111, 586–592. [Google Scholar] [CrossRef] [PubMed]
- Keegan, D.; McDermott, E.; Byrne, K.; Moloney, D.; Doherty, G.A.; Mulcahy, H.E. Development, validation and clinical assessment of a short questionnaire to assess disease-related knowledge in inflammatory bowel disease patients. Scand. J. Gastroenterol. 2013, 48, 183–188. [Google Scholar] [CrossRef] [PubMed]
- Maddux, M.; Gordy, A.; Schurman, C.; Cole, T.; Staggs, V. Initial Validation of IBD KNOW-IT: Measuring Patient and Caregiver Knowledge of a Child’s Disease and Treatment Regimen. J. Clin. Psychol. Med. Settings 2020, 27, 480–489. [Google Scholar] [CrossRef] [PubMed]
- Vernon-Roberts, A.; Otley, A.; Frampton, C.; Gearry, R.B.; Day, A.S. Response pattern analysis of IBD-KID: A knowledge assessment tool for children with inflammatory bowel disease. J. Paediatr. Child Health 2019, 55. [Google Scholar] [CrossRef]
- Vernon-Roberts, A.; Gearry, R.; Day, A. Assessment of knowledge levels following an education program for parents of children with inflammatory bowel disease. Front. Paediatr. Paediatr. Gastroenterol. Hepatol. Nutr. 2020, 8. [Google Scholar] [CrossRef]
- Vernon-Roberts, A.; Gearry, R.; Day, A. The level of public knowledge regarding inflammatory bowel disease in Christchurch, New Zealand. Inflamm. Intest. Dis. 2020, 5, 205–211. [Google Scholar] [CrossRef]
- Schunk, D.H. Progress Self-Monitoring. J. Exp. Educ. 1982, 51, 89–93. [Google Scholar] [CrossRef]
- Blok, A.C. A Middle-Range Explanatory Theory of Self-Management Behavior for Collaborative Research and Practice. Nurs. Forum 2017, 52, 138–146. [Google Scholar] [CrossRef] [PubMed]
- Silver, E.; Wallenstein, S.; Levy, A. Inward and Outward: The Role of Patient Self-Monitoring and Patient Communities in IBD: P-74. Inflamm. Bowel Dis. 2012, 18, S45–S46. [Google Scholar] [CrossRef]
- Lackner, J.M.; Jaccard, J.; Keefer, L.; Firth, R.; Carosella, A.M.; Sitrin, M.; Brenner, D. The accuracy of patient-reported measures for GI symptoms: A comparison of real time and retrospective reports. Neurogastroenterol. Motil. 2014, 26, 1802–1811. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Flood, E.; Silberg, D.; Romero, B.; Beusterien, K.; Erder, M.H.; Cuffari, C. Development of the pediatric daily ulcerative colitis signs and symptoms scale (DUCS): Qualitative research findings. BMC Res. Notes 2017, 10, 491. [Google Scholar] [CrossRef] [Green Version]
- Diederen, J.K.; Gerritsma, G.P.J.; Koot, M.B.; Tabbers, A.M.; Benninga, A.M.; Kindermann, A.A. Do Children and Adolescents with Inflammatory Bowel Disease Complete Clinical Disease Indices Similar to Physicians? J. Pediatr. Gastroenterol. Nutr. 2018, 66, 410–416. [Google Scholar] [CrossRef]
- Bellini, M.; Bove, A.; Sormani, M.P.; Battaglia, E.; Bocchini, R.; Alduini, P.; Bassotti, G.; Bruzzi, P.; Pucciani, F. The daily diary and the questionnaire are not equivalent for the evaluation of bowel habits. Dig. Liver Dis. 2010, 42, 99–102. [Google Scholar] [CrossRef] [PubMed]
- Watson, A.; Patience, L.; Pisano, U.; Heaney, D. OC-044 Introduction of an inflammatory bowel disease smart phone ‘app’: A qualitative study. Gut 2015, 64, A23. [Google Scholar] [CrossRef]
- Spiegel, B.M.R.; Hays, R.D.; Bolus, R.; Melmed, G.Y.; Chang, L.; Whitman, C.; Khanna, P.P.; Paz, S.H.; Hays, T.; Reise, S.; et al. Development of the NIH Patient-Reported Outcomes Measurement Information System (PROMIS) Gastrointestinal Symptom Scales. Am. J. Gastroenterol. 2014, 109, 1804–1814. [Google Scholar] [CrossRef] [Green Version]
- Hyams, S.J.; Ferry, D.G.; Mandel, S.F.; Gryboski, D.J.; Kibort, M.P.; Kirschner, S.B.; Griffiths, M.A.; Katz, J.A.; Grand, J.R.; Boyle, T.J.; et al. Development and Validation of a Pediatric Crohnʼs Disease Activity Index. J. Pediatr. Gastroenterol. Nutr. 1991, 12, 439–447. [Google Scholar] [CrossRef]
- Turner, D.; Otley, A.; Mack, D.; Hyams, J.; de Bruijne, J.; Uusoue, K.; Walters, T.; Zachos, M.; Mamula, P.; Beaton, D.; et al. Development, Validation, and Evaluation of a Pediatric Ulcerative Colitis Activity Index: A Prospective Multicenter Study. Gastroenterology 2007, 133, 423–432. [Google Scholar] [CrossRef]
- Lee, J.J.; Colman, J.R.; Mitchell, D.P.; Atmadja, L.M.; Bousvaros, R.A.; Lightdale, R.J. Agreement Between Patient- and Physician-completed Pediatric Ulcerative Colitis Activity Index Scores. J. Pediatr. Gastroenterol. Nutr. 2011, 52, 708–713. [Google Scholar] [CrossRef] [PubMed]
- Marcovitch, M.L.; Nissan, M.A.; Mack, M.D.; Otley, M.A.; Hussey, M.S.; McLean, M.B.; Lewis, M.M.; Croft, M.N.; Barakat, M.F.; Griffiths, M.A.; et al. Item Generation and Reduction Toward Developing a Patient-reported Outcome for Pediatric Ulcerative Colitis (TUMMY-UC). J. Pediatr. Gastroenterol. Nutr. 2017, 64, 373–377. [Google Scholar] [CrossRef] [PubMed]
- Crane, M.B.; Grant, A.; Hyams, J.; Croft, N.; Mack, D.R.; Hussey, S.; Sylvester, F.; Huynh, H.Q.; Turner, D.; Otley, A. A132 Development of the TUMMY-CD, a symptoms-based disease activity patient reported outcome (PRO) for pediatric crohn’s disease. J. Can. Assoc. Gastroenterol. 2018, 1, 197–198. [Google Scholar] [CrossRef] [Green Version]
- Vernon-Roberts, A.; Lopez, R.N.; Frampton, C.; Gearry, R.B.; Lemberg, D.A.; Day, A.S. A Symptom Self-report Tool for Children With Inflammatory Bowel Disease (IBDnow). J. Pediatr. Gastroenterol. Nutr. 2019, 69, e7–e12. [Google Scholar] [CrossRef]
- Brown, M.T.; Bussell, J.K. Medication Adherence: WHO Cares? Mayo Clin. Proc. 2011, 86, 304–314. [Google Scholar] [CrossRef] [Green Version]
- Hommel, K.A.; Davis, C.M.; Baldassano, R.N. Objective versus subjective assessment of oral medication adherence in pediatric inflammatory bowel disease. Inflamm. Bowel Dis. 2009, 15, 589–593. [Google Scholar] [CrossRef]
- De Civita, M.; Dobkin, P.L. Pediatric Adherence as a Multidimensional and Dynamic Construct, Involving a Triadic Partnership. J. Paediatr. Psychol. 2004, 29, 157–169. [Google Scholar] [CrossRef] [Green Version]
- Rapoff, M.A. Adherence to Paediatric Medical Regimens, 2nd ed.; Springer: New York, NY, USA, 2010. [Google Scholar]
- Mackner, M.L.; Crandall, V.W. Oral Medication Adherence in Pediatric Inflammatory Bowel Disease. Inflamm. Bowel Dis. 2005, 11, 1006–1012. [Google Scholar] [CrossRef] [PubMed]
- Oliva-Hemker, M.M.; Abadom, V.; Cuffari, C.; Thompson, R.E. Nonadherence with thiopurine immunomodulator and mesalamine medications in children with Crohn disease. J. Pediatr. Gastroenterol. Nutr. 2007, 44, 180–184. [Google Scholar] [CrossRef]
- Kitney, L.; Turner, J.M.; Spady, D.; Malik, B.; El-Matary, W.; Persad, R.; Huynh, H.Q. Predictors of medication adherence in pediatric inflammatory bowel disease patients at the Stollery Children’s Hospital. Can. J. Gastroenterol. 2009, 23, 811–815. [Google Scholar] [CrossRef]
- Hommel, A.K.; Mackner, M.L.; Denson, A.L.; Crandall, V.W. Treatment Regimen Adherence in Pediatric Gastroenterology. J. Pediatr. Gastroenterol. Nutr. 2008, 47, 526–543. [Google Scholar] [CrossRef] [Green Version]
- Reed-Knight, B.; Lewis, J.D.; Blount, R.L. Association of Disease, Adolescent, and Family Factors with Medication Adherence in Pediatric Inflammatory Bowel Disease. J. Paediatr. Psychol. 2011, 36, 308–317. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Nguyen, C.G.; Croitoru, S.K.; Silverberg, H.M.; Steinhart, V.A.; Weizman, V.A. Use of Complementary and Alternative Medicine for Inflammatory Bowel Disease Is Associated with Worse Adherence to Conventional Therapy: The COMPLIANT Study. Inflamm. Bowel Dis. 2016, 22, 1412–1417. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wall, C.L.; Day, A.S.; Gearry, R.B. Use of exclusive enteral nutrition in adults with Crohn’s disease: A review. World J. Gastroenterol. 2013, 19, 7652–7660. [Google Scholar] [CrossRef]
- Rodrigues, A.F.; Johnson, T.; Davies, P.; Murphy, M.S. Does polymeric formula improve adherence to liquid diet therapy in children with active Crohn’s disease? Arch. Dis. Child 2007, 92, 767–770. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Day, A.S.; Stephenson, T.; Stewart, M.; Otley, A.R. Exclusive enteral nutrition for children with Crohn’s disease: Use in Australia and attitudes of Australian paediatric gastroenterologists. J. Paediatr. Child Health 2009, 45, 337–341. [Google Scholar] [CrossRef]
- Paine, C.W.; Stollon, N.B.; Lucas, M.S.; Brumley, L.D.; Poole, E.S.; Peyton, T.; Grant, A.W.; Jan, S.; Trachtenberg, S.; Zander, M.; et al. Barriers and facilitators to successful transition from pediatric to adult inflammatory bowel disease care from the perspectives of providers. Inflamm. Bowel Dis. 2014, 20, 2083–2091. [Google Scholar] [CrossRef] [Green Version]
- Cole, R.; Ashok, D.; Razack, A.; Azaz, A.; Sebastian, S. Evaluation of Outcomes in Adolescent Inflammatory Bowel Disease Patients Following Transfer From Pediatric to Adult Health Care Services: Case for Transition. J. Adolesc. Health 2015, 57, 212–217. [Google Scholar] [CrossRef]
- Otto, C.; Tárnok, A.; Erős, A.; Szakács, Z.; Vincze, Á.; Farkas, N.; Sarlós, P. Planned Transition of Adolescent Patients with Inflammatory Bowel Disease Results in Higher Remission Rates. J. Paediatr. Nurs. 2019, 45, 62–66. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Fu, N.; Jacobson, K.; Round, A.; Evans, K.; Qian, H.; Bressler, B. Transition clinic attendance is associated with improved beliefs and attitudes toward medicine in patients with inflammatory bowel disease. World J. Gastroenterol. 2017, 23, 5405–5411. [Google Scholar] [CrossRef] [PubMed]
- Samson, M.C.; Mager, M.D.; Frazee, M.S.; Yu, M.F. Remission in Pediatric Inflammatory Bowel Disease Correlates With Prescription Refill Adherence Rates. J. Pediatr. Gastroenterol. Nutr. 2017, 64, 575–579. [Google Scholar] [CrossRef]
- Zacur, G.M.; Saeed, S.A.; Loreaux, K.; Rausch, J.R.; Williams, E.R.; Gray, W.; Hommel, K.A. Su2009 Medication Non-Adherence and Disease Severity in Pediatric Inflammatory Bowel Disease. Gastroenterology 2013, 144, S530–S531. [Google Scholar] [CrossRef]
- McGrady, M.E.; Hommel, K.A. Medication adherence and health care utilization in pediatric chronic illness: A systematic review. Pediatrics 2013, 132, 730–740. [Google Scholar] [CrossRef] [Green Version]
- Hommel, K.A.; Davis, C.M.; Baldassano, R.N. Medication adherence and quality of life in pediatric inflammatory bowel disease. J. Paediatr. Psychol. 2008, 33, 867–874. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Severs, M.; Fidder, H.H.; Mangen, M.-J.J.; van Der Valk, M.E.; van Der Have, M.; van Bodegraven, A.A.; Clemens, C.H.; Dijkstra, G.; Jeroen, M.; De Jong, D.J.; et al. Sa1944 Non-Adherence to Medical Therapy Is Associated With Hospitalizations and the Development of Active Disease in Inflammatory Bowel Disease. Gastroenterology 2016, 150, S412. [Google Scholar] [CrossRef]
- Severs, M.; Mangen, M.-J.J.; Fidder, H.H.; van der Valk, M.E.; van der Have, M.; van Bodegraven, A.A.; Clemens, C.H.; Dijkstra, G.; Jeroen, M.; De Jong, D.J.; et al. Sa1945 Lower Quality of Life, More Active Disease and Increased Healthcare Costs Due to Non-Adherence in Inflammatory Bowel Disease. Gastroenterology 2016, 150, S412. [Google Scholar] [CrossRef]
- Schurman, J.V.; Cushing, C.C.; Carpenter, E.; Christenson, K. Volitional and Accidental Nonadherence to Pediatric Inflammatory Bowel Disease Treatment Plans: Initial Investigation of Associations with Quality of Life and Disease Activity. J. Paediatr. Psychol. 2011, 36, 116–125. [Google Scholar] [CrossRef] [Green Version]
- Leleiko, S.N.; Lobato, J.D.; Hagin, J.S.; McQuaid, J.E.; Seifer, J.R.; Kopel, J.S.; Boergers, J.J.; Nassau, J.J.; Suorsa, J.K.; Shapiro, J.J.; et al. Rates and Predictors of Oral Medication Adherence in Pediatric Patients with IBD. Inflamm. Bowel Dis. 2013, 19, 832–839. [Google Scholar] [CrossRef] [Green Version]
- Marcum, Z.A.; Sevick, M.; Handler, S.M. Medication nonadherence: A diagnosable and treatable medical condition. JAMA 2013, 309, 2105–2106. [Google Scholar] [CrossRef]
- Maddux, M.; Ricks, S.; Delurgio, S.; Hommel, K. A Pilot Study Evaluating the Impact of an Adherence-promoting Intervention Among Nonadherent Youth With Inflammatory Bowel Disease. J. Paediatr. Nurs. 2017, 35, 72–77. [Google Scholar] [CrossRef]
- Greenley, R.N.; Karazsia, B.; Schurman, J.V.; Gumidyala, A.P.; Nguyen, E.U.; Thomason, M.M.; Walter, J.G.; Noe, J.; Werlin, S.; Kahn, S.A. Trajectories of Oral Medication Adherence in Youth With Inflammatory Bowel Disease. Health Psychol. 2015, 34, 514–521. [Google Scholar] [CrossRef] [PubMed]
- Wu, Y.P.; Rohan, J.M.; Martin, S.; Hommel, K.; Greenley, R.N.; Loiselle, K.; Ambrosino, J.; Fredericks, E.M. Pediatric Psychologist Use of Adherence Assessments and Interventions. J. Paediatr. Psychol. 2013, 38, 595–604. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mulder, D.J.; Noble, A.J.; Justinich, C.J.; Duffin, J.M. A tale of two diseases: The history of inflammatory bowel disease. J. Crohn’s Colitis 2014, 8, 341–348. [Google Scholar] [CrossRef] [Green Version]
- Quittner, A.L.; Modi, A.C.; Lemanek, K.L.; Ievers-Landis, C.E.; Rapoff, M.A. Evidence-based assessment of adherence to medical treatments in pediatric psychology. J. Paediatr. Psychol. 2008, 33, 916–936. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Severs, M.; Zuithoff, P.N.; Mangen, M.J.; van der Valk, M.E.; Siersema, P.D.; Fidder, H.H.; Oldenburg, B. Assessing Self-reported Medication Adherence in Inflammatory Bowel Disease: A Comparison of Tools. Inflamm. Bowel Dis. 2016, 22, 2158–2164. [Google Scholar] [CrossRef] [PubMed]
- Wu, Y.P.; Pai, A.L.H.; Gray, W.N.; Denson, L.A.; Hommel, K.A. Development and Reliability of a Correction Factor for Family-Reported Medication Adherence: Pediatric Inflammatory Bowel Disease as an Exemplar. J. Paediatr. Psychol. 2013, 38, 893–901. [Google Scholar] [CrossRef] [Green Version]
- Graves, M.M.; Roberts, M.C.; Rapoff, M.; Boyer, A. The Efficacy of Adherence Interventions for Chronically Ill Children: A Meta-Analytic Review. J. Paediatr. Psychol. 2010, 35, 368–382. [Google Scholar] [CrossRef] [PubMed]
- Ingerski, L.M.; Hente, E.A.; Modi, A.C.; Hommel, K.A. Electronic measurement of medication adherence in pediatric chronic illness: A review of measures. J. Paediatr. 2011, 159, 528–534. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Morisky, E.D.; Green, W.L.; Levine, M.D. Concurrent and Predictive Validity of a Self-reported Measure of Medication Adherence. Med. Care 1986, 24, 67–74. [Google Scholar] [CrossRef]
- Trindade, J.A.; Ehrlich, A.A.; Kornbluth, A.A.; Ullman, A.T. Are your patients taking their medicine? Validation of a new adherence scale in patients with inflammatory bowel disease and comparison with physician perception of adherence. Inflamm. Bowel Dis. 2011, 17, 599–604. [Google Scholar] [CrossRef] [PubMed]
- Alsous, M. Medication Adherence in Children. J. Health Commun. 2017, 2, 2. [Google Scholar] [CrossRef] [Green Version]
- Barnes, E.L.; Long, M.D.; Kappelman, M.D.; Martin, C.F.; Sandler, R.S. High Patient Activation Is Associated With Remission in Patients With Inflammatory Bowel Disease. Inflamm. Bowel Dis. 2019, 25, 1248–1254. [Google Scholar] [CrossRef] [PubMed]
- Hendriks, M.; Rademakers, J. Relationships between patient activation, disease-specific knowledge and health outcomes among people with diabetes; a survey study. BMC Health Serv. Res. 2014, 14, 393. [Google Scholar] [CrossRef] [Green Version]
- Keefer, L.L.; Kiebles, H.J.; Taft, H.T. The role of self-efficacy in inflammatory bowel disease management: Preliminary validation of a disease-specific measure. Inflamm. Bowel Dis. 2011, 17, 614–620. [Google Scholar] [CrossRef] [Green Version]
- Zijlstra, M.; De Bie, C.; Breij, L.; van Pieterson, M.; van Staa, A.; de Ridder, L.; van der Woude, J.; Escher, J. Self-efficacy in adolescents with inflammatory bowel disease: A pilot study of the “IBD-yourself”, a disease-specific questionnaire. J. Crohns Coliti 2013, 7, e375–e385. [Google Scholar] [CrossRef]
- Hibbard, J.H.; Stockard, J.; Mahoney, E.R.; Tusler, M. Development of the Patient Activation Measure (PAM): Conceptualizing and Measuring Activation in Patients and Consumers. Health Serv. Res. 2004, 39, 1005–1026. [Google Scholar] [CrossRef] [Green Version]
- Hibbard, J.H.; Mahoney, E.R.; Stockard, J.; Tusler, M. Development and Testing of a Short Form of the Patient Activation Measure. Health Serv. Res. 2005, 40, 1918–1930. [Google Scholar] [CrossRef] [Green Version]
- Martin, M.; Garcia, M.; Christofferson, M.; Bensen, R.; Yeh, A.M.; Park, K.T. Spanish and English Language Symposia to Enhance Activation in Pediatric Inflammatory Bowel Disease. J. Pediatr. Gastroenterol. Nutr. 2016, 63, 508–511. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Pennarola, B.W.; Rodday, A.M.; Mayer, D.K.; Ratichek, S.J.; Davies, S.M.; Syrjala, K.L.; Patel, S.; Bingen, K.; Kupst, M.J.; Schwartz, L.; et al. Factors Associated With Parental Activation in Pediatric Hematopoietic Stem Cell Transplant. Med. Care Res. Rev. 2012, 69, 194–214. [Google Scholar] [CrossRef] [PubMed]
- Graff, A.L.; Sexton, A.K.; Walker, R.J.; Clara, E.I.; Targownik, N.L.; Bernstein, N.C. Validating a Measure of Patient Self-efficacy in Disease Self-management Using a Population-based IBD Cohort: The IBD Self-efficacy Scale. Inflamm. Bowel Dis. 2016, 22, 2165–2172. [Google Scholar] [CrossRef] [Green Version]
- Izaguirre, R.M.; Taft, R.T.; Keefer, R.L. Validation of a Self-efficacy Scale for Adolescents and Young Adults With Inflammatory Bowel Disease. J. Pediatr. Gastroenterol. Nutr. 2017, 65, 546–550. [Google Scholar] [CrossRef]
- Cahill, P.; Papageorgiou, A. Triadic communication in the primary care paediatric consultation: A review of the literature. Br. J. Gen. Pract. 2007, 57, 904–911. [Google Scholar] [CrossRef] [Green Version]
- Tates, K.; Meeuwesen, L. Doctor–parent–child communication. A (re)view of the literature. Soc. Sci. Med. 2001, 52, 839–851. [Google Scholar] [CrossRef]
- Howells, R.; Lopez, T. Better communication with children and parents. Paediatr. Child Health 2008, 18, 381–385. [Google Scholar] [CrossRef]
- Varni, J.W.; Dark, C.V.; Bendo, C.B.; Pohl, J.F.; Shulman, R.J.; Self, M.M.; Zacur, G.M.; Saeed, S.A.; Patel, A.S.; Nurko, S.; et al. Patient Health Communication Mediating Effects Between Gastrointestinal Symptoms and Gastrointestinal Worry in Pediatric Inflammatory Bowel Disease. Inflamm. Bowel Dis. 2017, 23, 704–711. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hensinger, N.R. Communication Between the Doctor and the Child. J. Paediatr. Orthop. 2010, 30, 213–215. [Google Scholar] [CrossRef]
- Plevinsky, J.; Greenley, R.N.; Fishman, L. Self-management in patients with inflammatory bowel disease: Strategies, outcomes, and integration into clinical care. Clin. Exp. Gastroenterol. 2016, 9, 259–267. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Dunn, P.; Conard, S. Improving health literacy in patients with chronic conditions: A call to action. Int. J. Cardiol. 2018, 273, 249–251. [Google Scholar] [CrossRef] [PubMed]
- Kremer, A.; Mitchell, R.; Westwood, N.; Younge, L.; Ghosh, S. Talking about life and IBD: A paradigm for improving patient-physician communication. J. Crohn’s Colitis 2009, 3, 1–3. [Google Scholar] [CrossRef]
- Annunziato, R.A.; Bucuvalas, J.C.; Yin, W.; Arnand, R.; Alonso, E.M.; Mazariegos, G.V.; Venick, R.S.; Stuber, M.L.; Shneider, B.L.; Shemesh, E. Self-Management Measurement and Prediction of Clinical Outcomes in Pediatric Transplant. J. Paediatr. 2018, 193, 128–133. [Google Scholar] [CrossRef] [PubMed]
- Osborne, R.H.; Elsworth, G.R.; Whitfield, K. The Health Education Impact Questionnaire (heiQ): An outcomes and evaluation measure for patient education and self-management interventions for people with chronic conditions. Patient Educ. Couns. 2007, 66, 192–201. [Google Scholar] [CrossRef] [PubMed]
- NASPGHAN. Transitioning a Patient with IBD from Pediatric to Adult Care; Children’s Digestive Health and Nutrition Foundation: Flourtown, PA, USA, 2010. [Google Scholar]
- Whitfield, P.E.; Fredericks, M.E.; Eder, J.S.; Shpeen, H.B.; Adler, H.J. Transition Readiness in Pediatric Patients with Inflammatory Bowel Disease: Patient Survey of Self-Management Skills. J. Pediatr. Gastroenterol. Nutr. 2015, 60, 36–41. [Google Scholar] [CrossRef] [Green Version]
- Crandall, D.W.; Kappelman, B.M.; Colletti, E.R.; Leibowitz, I.I.; Grunow, H.J.; Ali, A.S.; Baron, J.H.; Berman, C.J.; Boyle, S.B.; Cohen, T.S.; et al. ImproveCareNow: The development of a pediatric inflammatory bowel disease improvement network. Inflamm. Bowel Dis. 2011, 17, 450–457. [Google Scholar] [CrossRef]
- Crandall, M.W.; Hommel, A.K.; Perez, M.E. Living well with inflammatory bowel disease. A self-management handbook for patients and families with IBD. In ImpoveCareNow; Nationwide Children’s Hospital & Cincinnati Children’s Hospital Medical Center: Cincinnati, OH, USA, 2011. [Google Scholar]
- Cohen, S.E.; Hooper, S.R.; Javalkar, K.; Haberman, C.; Fenton, N.; Lai, H.; Mahan, J.D.; Massengill, S.; Kelly, M.; Cantú, G.; et al. Self-Management and Transition Readiness Assessment: Concurrent, Predictive and Discriminant Validation of the STARx Questionnaire. J. Paediatr. Nurs. 2015, 30, 668–676. [Google Scholar] [CrossRef]
- Ferris, M.; Cohen, S.; Haberman, C.; Javalkar, K.; Massengill, S.; Mahan, J.D.; Kim, S.; Bickford, K.; Cantu, G.; Medeiros, M.; et al. Self-Management and Transition Readiness Assessment: Development, Reliability, and Factor Structure of the STARx Questionnaire. J. Paediatr. Nurs. 2015, 30, 691–699. [Google Scholar] [CrossRef]
- Ferris, M.E.; Harward, D.H.; Bickford, K.; Layton, J.B.; Ferris, M.T.; Hogan, S.L.; Gipson, D.S.; McCoy, L.P.; Hooper, S.R. A Clinical Tool to Measure the Components of Health-Care Transition from Pediatric Care to Adult Care: The UNCTRxANSITION Scale. Ren. Fail. 2012, 34, 744–753. [Google Scholar] [CrossRef]
- Klassen, A.F.; Grant, C.; Barr, R.; Brill, H.; Kraus De Camargo, O.; Ronen, G.M.; Samaan, M.C.; Mondal, T.; Cano, S.J.; Schlatman, A.; et al. Development and validation of a generic scale for use in transition programmes to measure self-management skills in adolescents with chronic health conditions: The TRANSITION-Q. Child Care Health Dev. 2015, 41, 547–558. [Google Scholar] [CrossRef] [PubMed]
- Williams, T.; Sherman, E.; Mah, J.K.; Blackman, M.; Latter, J.; Mohammed, I.; Slick, D.; Thornton, N. Measurement of medical self-management and transition readiness among Canadian adolescents with special health care needs. Int. J. Child Adolesc. Health 2010, 3, 527–535. [Google Scholar]
- Vernon-Roberts, A.; Frampton, C.; Gearry, R.; Day, A. Development and validation of a self-management skills assessment tool for children with Inflammatory Bowel Disease. J. Pediatr. Gastroenterol. Nutr. 2020, 72, 67–73. [Google Scholar] [CrossRef] [PubMed]
| First Author | Name | Year | Population | Items | Validity Tested | Reliability Tested | Readability Tested * | Transition Items ** | |
|---|---|---|---|---|---|---|---|---|---|
| General IBD knowledge | Eaden [25] | CCKNOW | 1999 | Adults | 30 | Yes | Yes | Yes E 77.9, Gr 4.4 | Yes |
| Jones [44] | KQ | 1993 | Adults | 9 | Yes | No | No | Yes | |
| Yoon [45] | IBD-KNOW | 2019 | Adults | 24 | Yes | Yes | Yes Gr 4.0 | Yes | |
| Keegan [47] | None | 2013 | Adults | 10 | Yes | Yes | No | Yes | |
| Casellas [46] | QUECOMIICAT | 2019 | Adults | 25 | Yes | Yes | No | Yes | |
| Tung [38] | Emma Quiz | 2015 | Children | 16 | No | No | No | No | |
| Haaland [26] | IBD-KID | 2014 | Children | 23 | Yes | Yes | Yes E 69, Gr 6.3 | No | |
| Vernon-Roberts [41] | IBD-KID2 | 2020 | Children | 15 | Yes | Yes | Yes E 77.2 | No | |
| Individual knowledge | Fishman [33] | None | 2011 | Children | No | No | No | No | |
| Gumidyala [35] | None | 2017 | Children | 12 | No | No | No | Yes | |
| Benchimol [4] | Health Passport | 2011 | Children | 28 | No | No | No | No | |
| Maddux [48] | IBD KNOW-IT | 2019 | Children | 23 | Yes | Yes | Yes E 75.5, Gr 6.3 | No |
| First Author | Name of Tool | Year | Origin | Topic | Age Range | Items | Validity Tested | Reliability Tested | Readability Tested | Insurance * | Transition ** |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Hait [5] | None | 2006 | US | IBD T | 11–23 | 17 | No | No | No | Yes | No |
| Fishman [32] | None | 2010 | US | IBD SM, T | 16–18 | 19 | No | No | No | No | No |
| Whitfield [126] | None | 2015 | US | IBD SM | 10–21 | 23 | No | No | No | No | Yes |
| NASPGHAN [125] | None | 2010 | US, CAN | IBD T | 12–17 | 27 | No | No | No | Yes | Yes |
| Klassen [132] | Transition-Q | 2014 | CAN | SM T | 12–18 | 14 | Yes | Yes | Yes Gr 4.4 | No | No |
| Ferris [130] | StarX | 2015 | US | SM T | 12–25 | 18 | Yes | Yes | Yes Gr 4.4 | No | Yes |
| Ferris [131] | UNX-Transition Scale | 2012 | US | SM T | 12–20 | 33 | Yes | Yes | No | Yes | Yes |
| Williams [133] | None | 2010 | CAN | SM T | 11–18 | 21 | Yes | Yes | Yes Gr 4.9 | Yes | Yes |
| Vernon-Roberts [134] | IBD-STAR | 2020 | NZ | IBD SM | 10–18 | 18 | Yes | Yes | Yes E 91, Gr 3.1 | No | No |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Vernon-Roberts, A.; Gearry, R.B.; Day, A.S. Overview of Self-Management Skills and Associated Assessment Tools for Children with Inflammatory Bowel Disease. Gastrointest. Disord. 2021, 3, 61-77. https://0-doi-org.brum.beds.ac.uk/10.3390/gidisord3020007
Vernon-Roberts A, Gearry RB, Day AS. Overview of Self-Management Skills and Associated Assessment Tools for Children with Inflammatory Bowel Disease. Gastrointestinal Disorders. 2021; 3(2):61-77. https://0-doi-org.brum.beds.ac.uk/10.3390/gidisord3020007
Chicago/Turabian StyleVernon-Roberts, Angharad, Richard B. Gearry, and Andrew S. Day. 2021. "Overview of Self-Management Skills and Associated Assessment Tools for Children with Inflammatory Bowel Disease" Gastrointestinal Disorders 3, no. 2: 61-77. https://0-doi-org.brum.beds.ac.uk/10.3390/gidisord3020007






