Advances in Leukocyte Biology
Share This Topical Collection
Editors
 Prof. Dr. Mihnea Zdrenghea
Prof. Dr. Mihnea Zdrenghea
 Prof. Dr. Mihnea Zdrenghea
Prof. Dr. Mihnea Zdrenghea
E-Mail
Website
Collection Editor
Department of Hematology, Iuliu Hatieganu University of Medicine and Pharmacy, 8 Babes Str., 400012 Cluj-Napoca, Romania
Interests: hematology; immunohematology
Topical Collection Information
Dear Colleagues,
The immune system balances between homeostasis and inflammation, conditions associated with health and disease. For this, every organ and every cell of the body is adapted to perform one or more certain basic body functions. These regulatory mechanisms limit the entry of pathogens and limit immune reactivity against self and foreign antigens. White blood cells, also called leukocytes, are very important components of these orchestrated immune responses. Neutrophils are the largest subpopulation of human leukocytes (about 60% of human white blood cells), representing the innate immune system's first line of defense against a wide range of microorganisms. Neutrophils contribute to immunity by their unique antimicrobial ability, including phagocytosis and the secretion of hydrolytic enzymes, the formation of reactive oxygen and nitrogen species, and the release of antimicrobial proteins and peptides. In addition to phagocytosis, living neutrophils create a network of cytonemes to capture microorganisms, whereas dying neutrophils form neutrophil extracellular traps (NETs) equipped with bactericides from neutrophil granules adsorbed on DNA strands. Neutrophils, the main fraction of myeloid leukocytes is seen in the early stages of acute inflammation and play an important role in the innate immune response. Lymphocytes are presented by T and B cells, i.e., two major components of adaptive immunity and natural killer cells. Natural killer cells play central role in the antiviral response. B cells contribute to immunity by secreting antibodies and also promote the activation of T cells. T cells play a central role in adaptive immunity; these T cell responses are adapted to their respective cognate antigen and show a high degree of heterogeneity. T cells are essential for suppressing inflammatory immune responses. Our knowledge of the multifaceted functions of leukocytes in normal and pathological conditions is rapidly expanding. Recent biomedical research has shown that the neutrophil-to-lymphocyte ratio (NLR) is a useful prognostic marker in many diseases, including COVID-19. Addressing this and other key questions in leukocyte biology will provide a deeper understanding of the role of leukocytes in immunity, which will help develop effective therapeutic strategies.
Prof. Dr. Galina F. Sud’ina
Prof. Dr. Mihnea Zdrenghea
Collection Editor
Manuscript Submission Information
Manuscripts should be submitted online at www.mdpi.com by registering and logging in to this website. Once you are registered, click here to go to the submission form. Manuscripts can be submitted until the deadline. All submissions that pass pre-check are peer-reviewed. Accepted papers will be published continuously in the journal (as soon as accepted) and will be listed together on the collection website. Research articles, review articles as well as short communications are invited. For planned papers, a title and short abstract (about 100 words) can be sent to the Editorial Office for announcement on this website.
Submitted manuscripts should not have been published previously, nor be under consideration for publication elsewhere (except conference proceedings papers). All manuscripts are thoroughly refereed through a single-blind peer-review process. A guide for authors and other relevant information for submission of manuscripts is available on the Instructions for Authors page. Biomedicines is an international peer-reviewed open access monthly journal published by MDPI.
Please visit the Instructions for Authors page before submitting a manuscript.
The Article Processing Charge (APC) for publication in this open access journal is 2600 CHF (Swiss Francs).
Submitted papers should be well formatted and use good English. Authors may use MDPI's
English editing service prior to publication or during author revisions.
Keywords
- leukocyte
- immunity
- inflammation
- neutrophil
- eosinophil
- basophil
- monocyte
- B cell
- T cell
- natural killer cells
- lymphocyte
Published Papers (5 papers)
Open AccessArticle
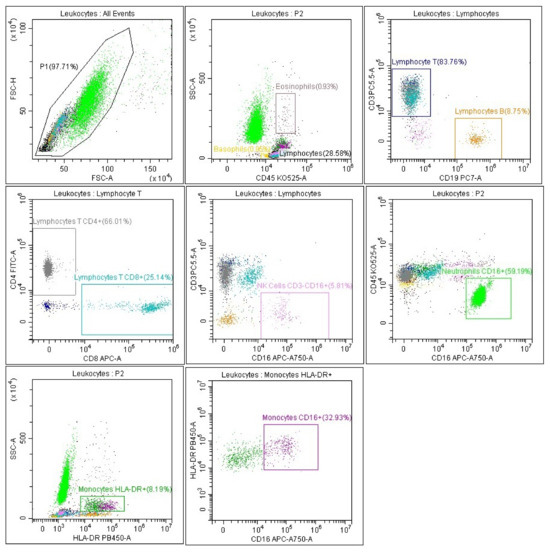
Analysis of Leukocyte Subpopulations by Flow Cytometry during Hospitalization Depending on the Severity of COVID-19 Course
by
Elżbieta Rutkowska, Iwona Kwiecień, Ewa Pietruszka-Wałęka, Ewa Więsik-Szewczyk, Piotr Rzepecki and Karina Jahnz-Różyk
Cited by 1 | Viewed by 1085
Abstract
The mechanisms underlying the immune response to coronavirus disease 2019 (COVID-19) and the recovery process have not been fully elucidated. The aim of the study was to analyze leukocyte subpopulations in patients at significant time points (at diagnosis, and 3 and 6 months
[...] Read more.
The mechanisms underlying the immune response to coronavirus disease 2019 (COVID-19) and the recovery process have not been fully elucidated. The aim of the study was to analyze leukocyte subpopulations in patients at significant time points (at diagnosis, and 3 and 6 months after infection) selected according to the analysis of changes in the lungs by the CT classification system, considering the severity of the disease. The study groups consisted of severe and non-severe COVID-19 patients. There was a significant decrease in CD8+ T cells, NK and eosinophils, with an increasing percentage of neutrophils during hospitalization. We noticed lower levels of CD4 and CD8 T lymphocytes, eosinophils, basophils, and CD16+ monocytes and elevated neutrophil levels in severe patients relative to non-severe patients. Three months after infection, we observed higher levels of basophils, and after 6 months, higher CD4/CD8 ratios and T cell levels in the severe compared to non-severe group. Non-severe patients showed significant changes in the leukocyte populations studied at time of hospitalization and both within 3 months and 6 months of onset. The CT CSS classification with parameters of the flow cytometry method used for COVID-19 patients determined changes that proved useful in the initial evaluation of patients.
Full article
►▼
Show Figures
Open AccessReview
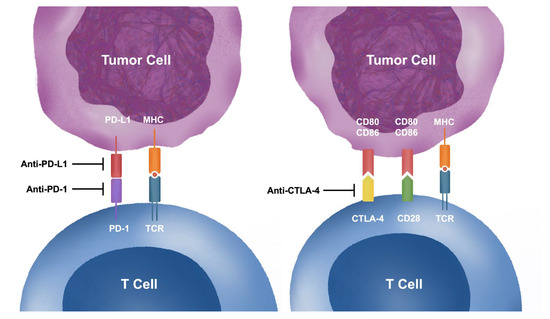
Immunopathogenesis of Immune Checkpoint Inhibitor Induced Myocarditis: Insights from Experimental Models and Treatment Implications
by
Chun-Ka Wong, Tsun-Ho Lam, Song-Yan Liao, Yee-Man Lau, Hung-Fat Tse and Benjamin Y. F. So
Cited by 5 | Viewed by 2319
Abstract
Despite the extraordinary success of immune checkpoint inhibitors (ICIs) in cancer treatment, their use is associated with a high incidence of immune-related adverse events (IRAEs), resulting from therapy-related autoimmunity against various target organs. ICI-induced myocarditis is one of the most severe forms of
[...] Read more.
Despite the extraordinary success of immune checkpoint inhibitors (ICIs) in cancer treatment, their use is associated with a high incidence of immune-related adverse events (IRAEs), resulting from therapy-related autoimmunity against various target organs. ICI-induced myocarditis is one of the most severe forms of IRAE, which is associated with risk of hemodynamic compromise and mortality. Despite increasing recognition and prompt treatment by clinicians, there remain significant gaps in knowledge regarding the pathophysiology, diagnosis and treatment of ICI-induced myocarditis. As the newly emerged disease entity is relatively rare, it is challenging for researchers to perform studies involving patients at scale. Alternatively, mouse models have been developed to facilitate research understanding of the pathogenesis of ICI-induced myocarditis and drug discovery. Transgenic mice with immune checkpoint genes knocked out allow induction of myocarditis in a highly reproducible manner. On the other hand, it has not been possible to induce ICI-induced myocarditis in wild type mice by injecting ICIs monotherapy alone. Additional interventions such as combinational ICI, tumor inoculation, cardiac sarcomere immunization, or cardiac irradiation are necessary to mimic the underlying pathophysiology in human cancer patients and to induce ICI-induced myocarditis successfully. This review focuses on the immunopathogenesis of ICI-induced myocarditis, drawing insights from human studies and animal models, and discusses the potential implications for treatment.
Full article
►▼
Show Figures
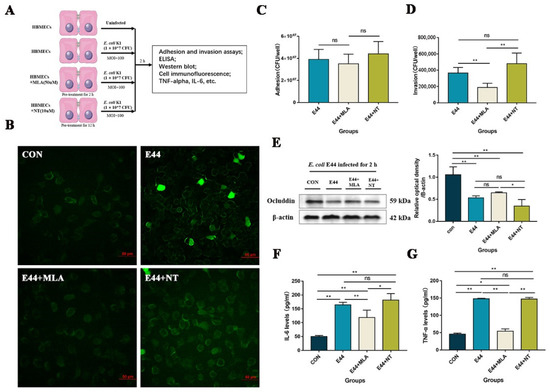
Open AccessArticle
Alpha7 Nicotinic Acetylcholine Receptor Antagonists Prevent Meningitic Escherichia coli-Induced Blood–Brain Barrier Disruptions by Targeting the CISH/JAK2/STAT5b Axis
by
Zelong Gong, Xuefeng Gao, Yubin Li, Jinhu Zou, Jingxian Lun, Jie Chen, Chengxing Zhou, Xiaolong He and Hong Cao
Cited by 2 | Viewed by 1523
Abstract
Despite the availability of antibiotics over the last several decades, excessive antibiotic treatments for bacterial sepsis and meningitis (BSM) in children may result in several adverse outcomes. Hematogenous pathogens may directly induce permeability increases in human brain microvascular endothelial cells (HBMECs) and blood–brain
[...] Read more.
Despite the availability of antibiotics over the last several decades, excessive antibiotic treatments for bacterial sepsis and meningitis (BSM) in children may result in several adverse outcomes. Hematogenous pathogens may directly induce permeability increases in human brain microvascular endothelial cells (HBMECs) and blood–brain barrier (BBB) dysfunctions. Our preliminary studies demonstrated that the alpha7 nicotinic acetylcholine receptor (α7nAChR) played an important role in the pathogenesis of BSM, accompanied by increasing cytokine-inducible SH2-containing protein (CISH) at the transcriptome level, but it has remained unclear how α7nAChR-CISH works mechanistically. The study aims to explore the underlying mechanism of α7nAChR and CISH during
E. coli-induced BSM in vitro (HBMECs) and in vivo (α7nAChR-KO mouse). We found that in the stage of
E. coli K1-induced BBB disruptions, α7nAChR functioned as the key regulator that affects the integrity of HBMECs by activating the JAK2–STAT5 signaling pathway, while CISH inhibited JAK2–STAT5 activation and exhibited protective effects against
E. coli infection. Notably, we first validated that the expression of CISH could be regulated by α7nAChR in HBMECs. In addition, we determined the protective effects of MLA (methyllycaconitine citrate) and MEM (memantine hydrochloride) (functioning as α7nAChR antagonists) on infected HBMECs and suggested that the α7nAChR–CISH axis could explain the protective effects of the two small-molecule compounds on
E. coli-induced HBMECs injuries and BBB disruptions. In conclusion, we dissected the α7nAChR/CISH/JAK2/STAT5 axis as critical for the pathogenesis of
E. coli-induced brain microvascular leakage and BBB disruptions and provided novel evidence for the development of α7nAChR antagonists in the prevention of pediatric
E. coli BSM.
Full article
►▼
Show Figures
Open AccessReview
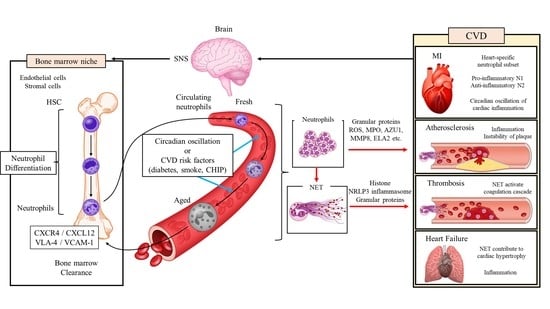
Neutrophils and Neutrophil Extracellular Traps in Cardiovascular Disease: An Overview and Potential Therapeutic Approaches
by
Kohsuke Shirakawa and Motoaki Sano
Cited by 11 | Viewed by 3268
Abstract
Recent advances in pharmacotherapy have markedly improved the prognosis of cardiovascular disease (CVD) but have not completely conquered it. Therapies targeting the NOD-like receptor family pyrin domain containing 3 inflammasome and its downstream cytokines have proven effective in the secondary prevention of cardiovascular
[...] Read more.
Recent advances in pharmacotherapy have markedly improved the prognosis of cardiovascular disease (CVD) but have not completely conquered it. Therapies targeting the NOD-like receptor family pyrin domain containing 3 inflammasome and its downstream cytokines have proven effective in the secondary prevention of cardiovascular events, suggesting that inflammation is a target for treating residual risk in CVD. Neutrophil-induced inflammation has long been recognized as important in the pathogenesis of CVD. Circadian rhythm-related and disease-specific microenvironment changes give rise to neutrophil diversity. Neutrophils are primed by various stimuli, such as chemokines, cytokines, and damage-related molecular patterns, and the activated neutrophils contribute to the inflammatory response in CVD through degranulation, phagocytosis, reactive oxygen species generation, and the release of neutrophil extracellular traps (NETs). In particular, NETs promote immunothrombosis through the interaction with vascular endothelial cells and platelets and are implicated in the development of various types of CVD, such as acute coronary syndrome, deep vein thrombosis, and heart failure. NETs are promising candidates for anti-inflammatory therapy in CVD, and their efficacy has already been demonstrated in various animal models of the disease; however, they have yet to be clinically applied in humans. This narrative review discusses the diversity and complexity of neutrophils in the trajectory of CVD, the therapeutic potential of targeting NETs, and the related clinical issues.
Full article
►▼
Show Figures
Open AccessArticle
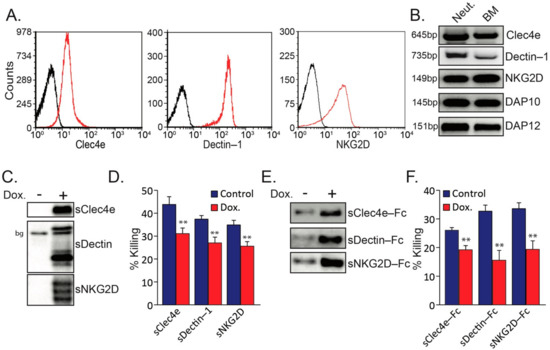
Recognition of Tumor Nidogen-1 by Neutrophil C-Type Lectin Receptors
by
Ronit Vogt Sionov, Chrystelle Lamagna and Zvi Granot
Cited by 2 | Viewed by 2187
Abstract
Neutrophil-mediated cytotoxicity toward tumor cells requires cell contact and is mediated by hydrogen peroxide. We have recently shown that Cathepsin G expressed on the neutrophil surface interacts with tumor RAGE, and this interaction facilitates neutrophil cytotoxicity. Interruption of the Cathepsin G–RAGE interaction led
[...] Read more.
Neutrophil-mediated cytotoxicity toward tumor cells requires cell contact and is mediated by hydrogen peroxide. We have recently shown that Cathepsin G expressed on the neutrophil surface interacts with tumor RAGE, and this interaction facilitates neutrophil cytotoxicity. Interruption of the Cathepsin G–RAGE interaction led to 50–80% reduction in cytotoxicity, suggesting that additional interactions are also involved. Here we show that blocking antibodies to the C-type lectin receptors (CLRs) Clec4e and Dectin-1, but not those to NKG2D, attenuated murine neutrophil cytotoxicity towards murine tumor cells, suggesting a contributing role for these CLRs in neutrophil recognition of tumor cells. We further observed that the CLRs interact with tumor Nidogen-1 and Hspg2, two sulfated glycoproteins of the basement membrane. Both Nidogen-1 and Hspg2 were found to be expressed on the tumor cell surface. The knockdown of Nidogen-1, but not that of Hspg2, led to reduced susceptibility of the tumor cells to neutrophil cytotoxicity. Altogether, this study suggests a role for CLR–Nidogen-1 interaction in the recognition of tumor cells by neutrophils, and this interaction facilitates neutrophil-mediated killing of the tumor cells.
Full article
►▼
Show Figures