Psychological Effects of the COVID-19 Pandemic on Hungarian Adults
Abstract
:1. Introduction
2. Materials and Methods
2.1. Course of the Project
2.2. Measuring Instruments
2.3. Statistical Analyses
2.4. Participants
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- World Health Organization. Timeline of WHO’s Response to COVID-19. 2020. Available online: https://www.who.int/news/item/29-06-2020-covidtimeline (accessed on 14 November 2020).
- U.S. Embassy in Hungary. Health Alert—U.S. Embassy Budapest, Hungary 13 March 2020. 2020. Available online: https://hu.usembassy.gov/health-alert-u-s-embassy-budapest-hungary-march-13-2020/ (accessed on 14 November 2020).
- U.S. Embassy in Hungary. Health Alert—U.S. Embassy Budapest, Hungary 29 May 2020. 2020. Available online: https://hu.usembassy.gov/health-alert-u-s-embassy-budapest-hungary-may-29-2020/ (accessed on 14 November 2020).
- Holmes, E.A.; O’Connor, R.C.; Perry, V.H.; Tracey, I.; Wessely, S.; Arseneault, L.; Ballard, C.; Christensen, H.; Cohen Silver, R.; Everall, I.; et al. Multidisciplinary research priorities for the COVID-19 pandemic: A call for action for mental health science. Lancet Psychiatry 2020, 7, 547–560. [Google Scholar] [CrossRef]
- Li, W.; Yang, Y.; Liu, Z.H.; Zhao, Y.J.; Zhang, Q.; Zhang, L.; Cheung, T.; Xiang, Y.T. Progression of Mental Health Services during the COVID-19 Outbreak in China. Int. J. Biol. Sci. 2020, 16, 1732–1738. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Liu, S.; Yang, L.; Zhang, C.; Xiang, Y.T.; Liu, Z.; Hu, S.; Zhang, B. Online mental health services in China during the COVID-19 outbreak. Lancet Psychiatry 2020, 7, e17–e18. [Google Scholar] [CrossRef]
- Mazza, C.; Ricci, E.; Biondi, S.; Colasanti, M.; Ferracuti, S.; Napoli, C.; Roma, P. A Nationwide Survey of Psychological Distress among Italian People during the COVID-19 Pandemic: Immediate Psychological Responses and Associated Factors. Int. J. Environ. Res. Public Health 2020, 17, 3165. [Google Scholar] [CrossRef] [PubMed]
- Mesa Vieira, C.; Franco, O.H.; Gómez Restrepo, C.; Abel, T. COVID-19: The forgotten priorities of the pandemic. Maturitas 2020, 136, 38–41. [Google Scholar] [CrossRef]
- Ozamiz-Etxebarria, N.; Dosil-Santamaria, M.; Picaza-Gorrochategui, M.; Idoiaga-Mondragon, N. Stress, anxiety, and depression levels in the initial stage of the COVID-19 outbreak in a population sample in the northern Spain. Cad de Saude Publica 2020, 36, e00054020. [Google Scholar] [CrossRef]
- Ren, Y.; Zhou, Y.; Qian, W.; Li, Z.; Liu, Z.; Wang, R.; Qi, L.; Yang, J.; Song, X.; Zeng, L.; et al. Letter to the Editor “A longitudinal study on the mental health of general population during the COVID-19 epidemic in China”. Brain Behav. Immun. 2020, 87, 132–133. [Google Scholar] [CrossRef]
- Van Agteren, J.; Bartholomaeus, J.; Fassnacht, D.B.; Iasiello, M.; Ali, K.; Lo, L.; Kyrios, M. Using Internet-Based Psychological Measurement to Capture the Deteriorating Community Mental Health Profile During COVID-19: Observational Study. JMIR Ment. Health 2020, 7, e20696. [Google Scholar] [CrossRef]
- Wang, J.; Wang, J.X.; Yang, G.S. The Psychological Impact of COVID-19 on Chinese Individuals. Yonsei Med. J. 2020, 61, 438–440. [Google Scholar] [CrossRef]
- Wang, C.; Pan, R.; Wan, X.; Tan, Y.; Xu, L.; Ho, C.S.; Ho, R.C. Immediate Psychological Responses and Associated Factors during the Initial Stage of the 2019 Coronavirus Disease (COVID-19) Epidemic among the General Population in China. Int. J. Environ. Res. Public Health 2020, 17, 1729. [Google Scholar] [CrossRef] [Green Version]
- Roohafza, H.; Feizi, A.; Afshar, H.; Mazaheri, M.; Behnamfar, O.; Hassanzadeh-Keshteli, A.; Adibi, P. Path analysis of relationship among personality, perceived stress, coping, social support, and psychological outcomes. World J. Psychiatry 2016, 6, 248–256. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bäuerle, A.; Steinbach, J.; Schweda, A.; Beckord, J.; Hetkamp, M.; Weismüller, B.; Kohler, H.; Musche, V.; Dörrie, N.; Teufel, M.; et al. Mental Health Burden of the COVID-19 Outbreak in Germany: Predictors of Mental Health Impairment. J. Prim. Care Community Health 2020, 11, 2150132720953682. [Google Scholar] [CrossRef] [PubMed]
- American Psychological Associaton. Patient Health Questionnaire (PHQ-9 & PHQ-2). 2020. Available online: https://www.apa.org/pi/about/publications/caregivers/practice-settings/assessment/tools/patient-health (accessed on 6 December 2020).
- Kroenke, K.; Spitzer, R.L.; Williams, J.B.; Löwe, B. The Patient Health Questionnaire Somatic, Anxiety, and Depressive Symptom Scales: A systematic review. Gen. Hosp. Psychiatry 2010, 32, 345–359. [Google Scholar] [CrossRef] [PubMed]
- Duan, L.; Shao, X.; Wang, Y.; Huang, Y.; Miao, J.; Yang, X.; Zhu, G. An investigation of mental health status of children and adolescents in china during the outbreak of COVID-19. J. Affect. Disord. 2020, 275, 112–118. [Google Scholar] [CrossRef]
- Fu, W.; Wang, C.; Zou, L.; Guo, Y.; Lu, Z.; Yan, S.; Mao, J. Psychological health, sleep quality, and coping styles to stress facing the COVID-19 in Wuhan, China. Transl. Psychiatry 2020, 10, 225. [Google Scholar] [CrossRef]
- Li, Q. Psychosocial and coping responses toward 2019 coronavirus diseases (COVID-19): A cross-sectional study within the Chinese general population. QJM Mon. J. Assoc. Physicians 2020, 113, 731–738. [Google Scholar] [CrossRef]
- Widiger, T.A. Neuroticism. In Handbook of Individual Differences in Social Behavior; The Guilford Press: New York, NY, USA, 2009; pp. 129–146. [Google Scholar]
- Widiger, T.A.; Oltmanns, J.R. Neuroticism is a fundamental domain of personality with enormous public health implications. World Psychiatry Off. J. World Psychiatr. Assoc. (WPA) 2017, 16, 144–145. [Google Scholar] [CrossRef] [Green Version]
- ClinicalTrials.gov. National Library of Medicine (U.S.). Psychological Effects of the COVID-19 Pandemic on the Hungarian Adult Population. Identifier: NCT04426266. 2020. Available online: https://clinicaltrials.gov/ct2/show/NCT04426266 (accessed on 14 November 2020).
- Cohen, S.; Kamarck, T.; Mermelstein, R. A global measure of perceived stress. J. Health Soc. Behav. 1983, 24, 385–396. [Google Scholar] [CrossRef]
- Cole, S.R. Assessment of differential item functioning in the Perceived Stress Scale-10. J. Epidemiol. Community Health 1999, 53, 319–320. [Google Scholar] [CrossRef] [Green Version]
- Coons, S.J.; Rao, S.; Keininger, D.L.; Hays, R.D. A comparative review of generic quality-of-life instruments. Pharmacoeconomics 2000, 17, 13–35. [Google Scholar] [CrossRef]
- Ozsváth, K. Önjellemző panaszleltár neurotikusok szűrővizsgálatára [Self-administered complaint inventory for screening neurotics]. In Pszichodiagnosztikai Vademecum I/2; Mérei, F., Szakács, F., Eds.; Nemzeti Tankönyvkiadó: Budapest, Hungary, 1994; pp. 114–122. [Google Scholar]
- Folkman, S.; Lazarus, R.S. An analysis of coping in a middle-aged community sample. J. Health Soc. Behav. 1980, 21, 219–239. [Google Scholar] [CrossRef] [PubMed]
- Kopp, M.; Skrabski, Á. Alkalmazott Magatartástudomány, A megbírkózás Egyéni és Társadalmi Stratégiái [Applied Behavioural Science, Individual and Social Strategies for Coping]; Corvinus Kiadó: Budapest, Hungary, 1995. [Google Scholar]
- Gerald, B. A Brief Review of Independent, Dependent and One Sample t-test. Int. J. Appl. Math. Theor. Phys. 2018, 4, 50–54. [Google Scholar] [CrossRef] [Green Version]
- Wadhwa, R.R.; Marappa-Ganeshan, R. T Test. In StatPearls, © 2020; StatPearls Publishing LLC.: Treasure Island, FL, USA, 2020. [Google Scholar]
- Glen, S. T Test (Student’s T-Test): Definition and Examples. StatisticsHowTo.com, 2020. Available online: https://www.statisticshowto.com/probability-and-statistics/t-test/ (accessed on 6 December 2020).
- Laerd Statistics. One-Sample T-Test Using SPSS Statistics. 2018. Available online: https://statistics.laerd.com/spss-tutorials/one-sample-t-test-using-spss-statistics.php (accessed on 6 December 2020).
- Chodkiewicz, J.; Talarowska, M.; Miniszewska, J.; Nawrocka, N.; Bilinski, P. Alcohol Consumption Reported during the COVID-19 Pandemic: The Initial Stage. Int. J. Environ. Res. Public Health 2020, 17, 4677. [Google Scholar] [CrossRef] [PubMed]
- González-Sanguino, C.; Ausín, B.; Castellanos, M.; Saiz, J.; López-Gómez, A.; Ugidos, C.; Muñoz, M. Mental health consequences during the initial stage of the 2020 Coronavirus pandemic (COVID-19) in Spain. Brain Behav. Immunity 2020, 87, 172–176. [Google Scholar] [CrossRef]
- Nwachukwu, I.; Nkire, N.; Shalaby, R.; Hrabok, M.; Vuong, W.; Gusnowski, A.; Surood, S.; Urichuk, L.; Greenshaw, A.J.; Agyapong, V.I.O. COVID-19 Pandemic: Age-Related Differences in Measures of Stress, Anxiety and Depression in Canada. Int. J. Environ. Res. Public Health 2020, 17, 6366. [Google Scholar] [CrossRef]
- Pedrozo-Pupo, J.C.; Pedrozo-Cortés, M.J.; Campo-Arias, A. Perceived stress associated with COVID-19 epidemic in Colombia: An online survey. Cad de Saude Publica 2020, 36, e00090520. [Google Scholar] [CrossRef]
- Shen, W.; Long, L.M.; Shih, C.H.; Ludy, M.J. A Humanities-Based Explanation for the Effects of Emotional Eating and Perceived Stress on Food Choice Motives during the COVID-19 Pandemic. Nutrients 2020, 12, 2712. [Google Scholar] [CrossRef]
- Speth, M.M.; Singer-Cornelius, T.; Oberle, M.; Gengler, I.; Brockmeier, S.J.; Sedaghat, A.R. Mood, Anxiety and Olfactory Dysfunction in COVID-19: Evidence of Central Nervous System Involvement? Laryngoscope 2020. [Google Scholar] [CrossRef]
- Stauder, A.; Konkoly-Thege, B. Az észlelt stressz kérdőív (PSS) magyar verziójának jellemzői [Characteristics of the Hungarian version of the Perceived Stress Scale (PSS)]. Mentálhigiéné és Pszichoszomatika 2006, 7, 203–216. [Google Scholar] [CrossRef] [Green Version]
- Dalgard, F.J.; Gieler, U.; Tomas-Aragones, L.; Lien, L.; Poot, F.; Jemec, G.B.E.; Misery, L.; Szabo, C.; Linder, D.; Sampogna, F.; et al. The psychological burden of skin diseases: A cross-sectional multicenter study among dermatological out-patients in 13 European countries. J. Investig. Dermatol. 2015, 135, 984–991. [Google Scholar] [CrossRef] [Green Version]
- Szabó, C.; Altmayer, A.; Kemény, L.; Dalgard, F. Magyar bőrgyógyászati járóbetegek pszichológiai jellemzői [Psychological attributes of Hungarian dermatology outpatients]. Bőrgyógyászati és Venerológiai Szle. 2016, 92, 263. [Google Scholar]
- Dalgard, F.J.; Bewley, A.; Evers, A.W.; Gieler, U.; Lien, L.; Sampogna, F.; Ständer, S.; Tomas-Aragones, L.; Vulink, N.; Kupfer, J. Stigmatisation and body image impairment in dermatological patients: Protocol for an observational multicentre study in 16 European countries. BMJ Open 2018, 8, e024877. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Szabó, C.; Altmayer, A.; Kemény, L.; Dalgard, F.; Kupfer, J. Magyar bőrgyógyászati járóbetegek pszichológiai jellemzői a második európai (ESDAP) pszichodermatológiai vizsgálat alapján[Psychological attributes of Hungarian dermatology outpatients based on the 2nd European (ESDaP) psychodermatology study]. Bőrgyógyászati és Venerológiai Szemle 2019, 95, 282. [Google Scholar]
- Szende, A.; Németh, R. Health-related quality of life of the Hungarian population. Orv. Hetil. 2003, 144, 1667–1674. [Google Scholar]
- Zhao, X.; Lan, M.; Li, H.; Yang, J. Perceived stress and sleep quality among the non-diseased general public in China during the 2019 coronavirus disease: A moderated mediation model. Sleep Med. 2020. [Google Scholar] [CrossRef]
- World Health Organization. Depression and Other Common Mental Disorders—Global Health Estimates. 2017. Available online: https://apps.who.int/iris/bitstream/handle/10665/254610/WHO-MSD-MER-2017.2-eng.pdf (accessed on 14 November 2020).
- EuroStat. Share of the Population Reporting that They Had Chronic Depression, 2017. 2020. Available online: https://ec.europa.eu/eurostat/statistics-explained/index.php?title=File:Share_of_the_population_reporting_that_they_had_chronic_depression,_2017_(%25)_Health20.png (accessed on 14 November 2020).
- Purebl, G.; Balog, P. A depressziós tünetegyüttes jelentősege az esélyteremtes szempontjából [Significance of depressive syndrome in terms of creating opportunities]. In Magyar Lelkiállapot, 2008: Esélyerősítés es Életminőseg a mai Magyar Társadalomban; Kopp, M., Ed.; Semmelweis Kiadó: Budapest, Hungary, 2008; pp. 584–591. [Google Scholar]
- EuroStat. Share of the population aged 15 years and over reporting that they had consulted a psychologist, psychotherapist or psychiatrist, 2014. 2020. Available online: https://ec.europa.eu/eurostat/statistics-explained/index.php?title=File:Share_of_the_population_aged_15_years_and_over_reporting_that_they_had_consulted_a_psychologist,_psychotherapist_or_psychiatrist,_2014_(%25)_Health20.png (accessed on 14 November 2020).
- Havnen, A.; Anyan, F.; Hjemdal, O.; Solem, S.; Gurigard Riksfjord, M.; Hagen, K. Resilience Moderates Negative Outcome from Stress during the COVID-19 Pandemic: A Moderated-Mediation Approach. Int. J. Environ. Res. Public Health 2020, 17, 6461. [Google Scholar] [CrossRef]


| Author and Year | Time of Assessment | Location | The Assessment Tools (Relevant to Present Study) | Participants (Relevant to Present Study) | Age | Female | The Main Outcomes (Relevant to Present Study) |
|---|---|---|---|---|---|---|---|
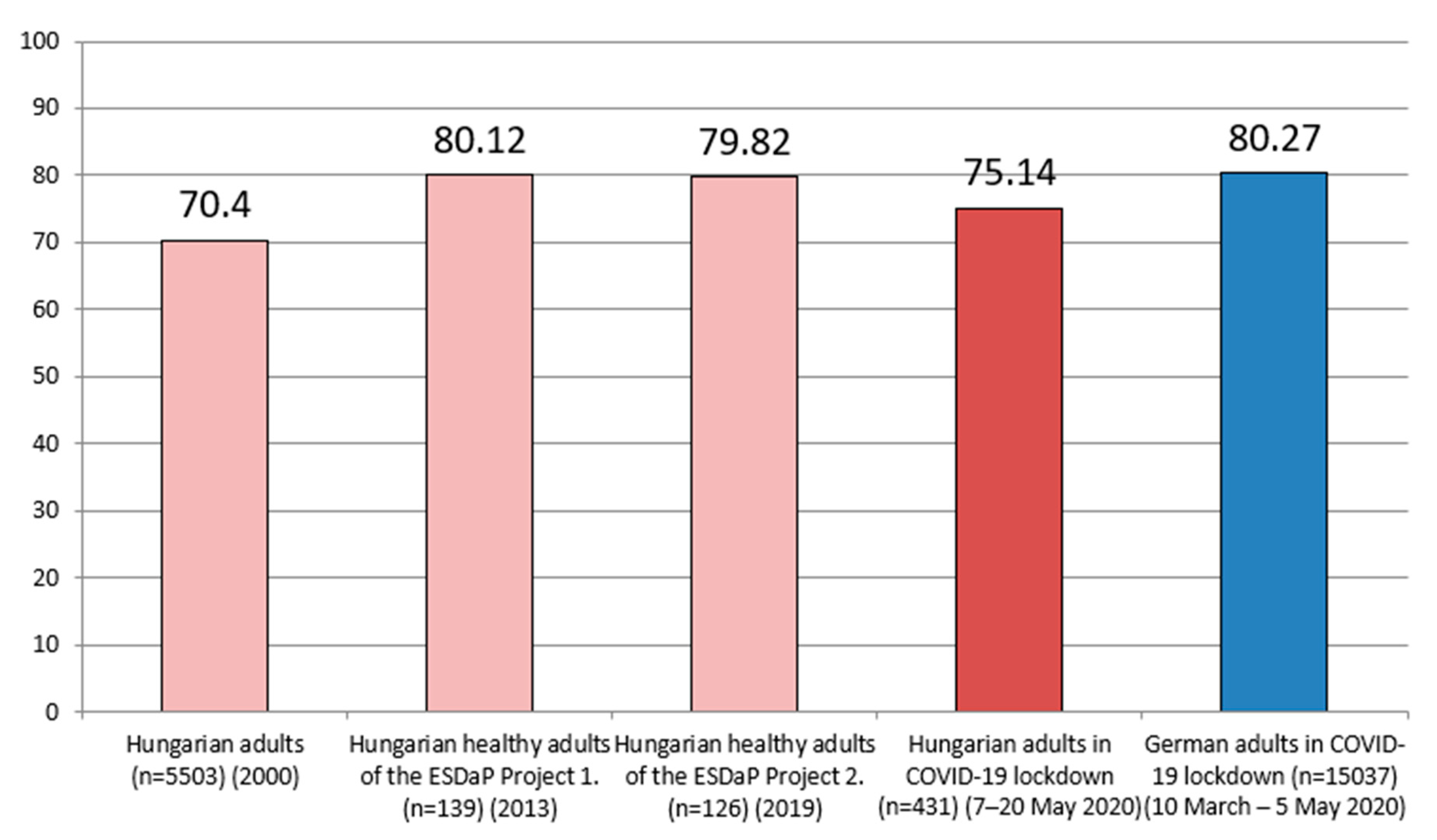
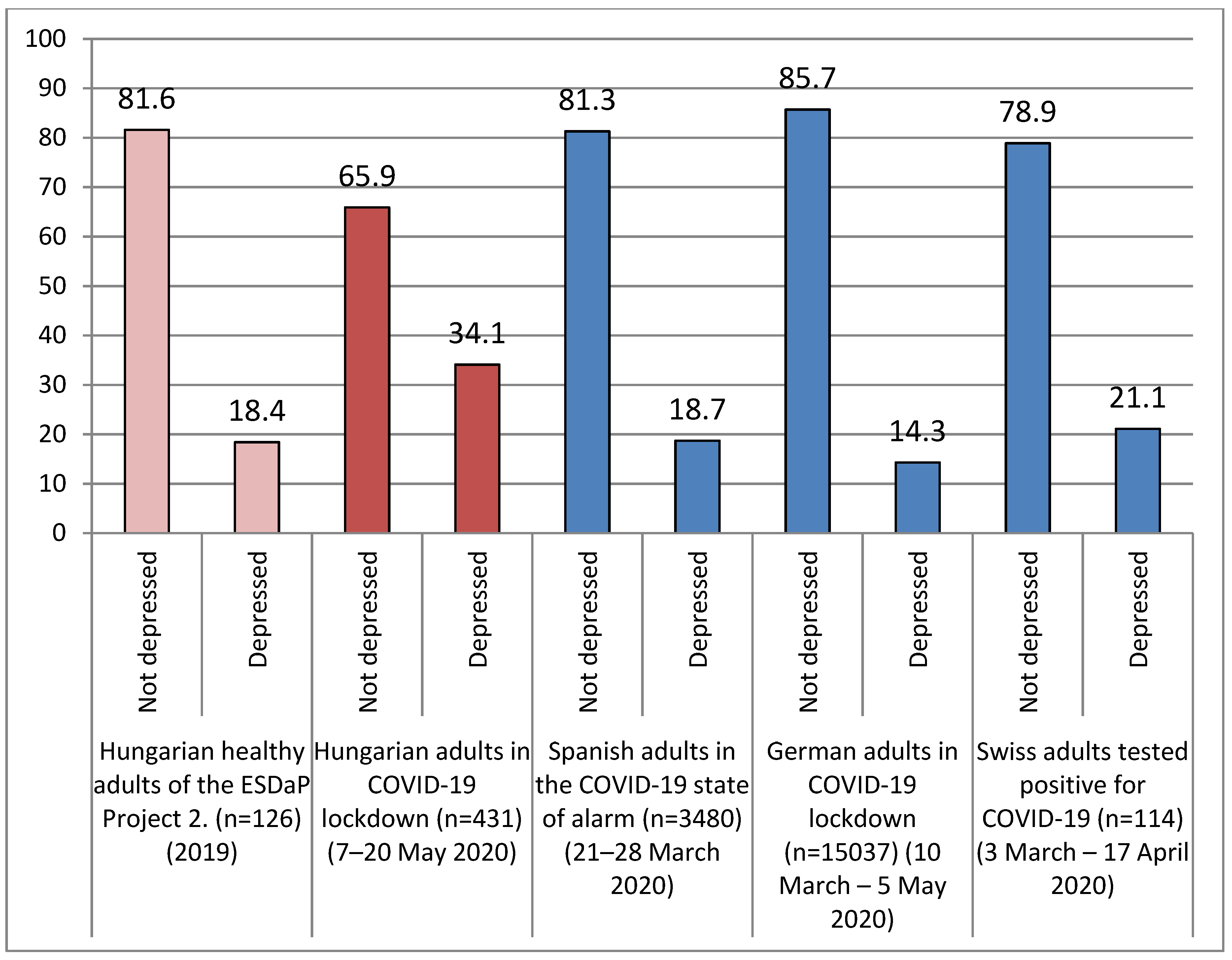
| Bäuerle et al., (2020) [15] | 10 March–5 May 2020 | Germany | EQ-VAS; PHQ-2; GAD-2 | adults residing in Germany in COVID-19 lockdown (n = 15037) | NA | 70.07% | EQ-VAS = 80.27; PHQ-2: prevalence of 14.3% for depression; GAD-2: prevalence of 19.7% for anxiety |
| Chodkiewicz et al., (2020) [34] | 10–20 April 2020 | Poland | PSS-10 | adult population in COVID-19 lockdown (n = 443) | 31.9 ± 11.31 | 78.6% | PSS-10 = 19.22 |
| González-Sanguino et al., (2020) [35] | 21–28 March 2020 | Spain | PHQ-2; GAD-2 | general adult population in the COVID-19 state of alarm (n = 3480) | 37.92 | 75% | PHQ-2: prevalence of 18.7% for depression; GAD-2: prevalence of 21.6% for anxiety |
| Nwachukwu et al., (2020) [36] | 23 March–3 May 2020 | Canada | PSS-10 | adult population during the COVID-19 pandemic (n = 8267) | 42.09 ± 3.44 | 87.1% | PSS-10 = 20.81 ± 6.83 |
| Pedrozo-Pupo et al., (2020) [37] | 21–23 March 2020 | Colombia | PSS-10-C | adult population in COVID-19 lockdown (n = 406) | 43.9 ± 12.4 | 61.8% | PSS-10-C = 16.5 ± 7.3 |
| Shen et al., (2020) [38] | 1–27 June 2020 | USA | PSS-10 | adults residing in the US during the COVID-19 pandemic (n = 800) | NA | 83% | PSS-10= 18.27 ± 7.34 |
| Speth et al., (2020) [39] | 3 March–17 April 2020 | Switzerland (Aarau, Kantonsspital Aarau) | PHQ-2; GAD-2 | adults tested positive for COVID-19 (n = 114) | 44.6 ± 16.1 | 54.4% | PHQ-2: prevalence of 21.1% for depression; GAD-2: prevalence of 10.5% for anxiety |
| Stauder & Konkoly-Thege (2006) [40] | 2006 | Hungary (Budapest) | PSS-10 | adult participants of a behavioral-based stress management program (n = 69) | NA | NA | PSS-10 = 17.5 ± 6.0 |
| Szabó et al., (2016) [41,42] | 2011–2013 | Hungary (Szeged) | EQ-VAS | hospital employees at the research institution (n = 139) | 39.53 ± 2.01 | 75% | EQ-VAS = 80.12 ± 17.76 |
| Szabó et al., (2019) [43,44] | 2017–2019 | Hungary (Szeged) | EQ-VAS; PHQ-2; GAD-2; PSS-10 | hospital staff members of the research institution (n = 126) | 38.94 ± 2.31 | 82% | EQ-VAS = 79.82 ± 16.13; PSS-10 = 17.76 ± 5.39; PHQ-2: prevalence of 18.4% for depression; GAD-2: prevalence of 24% for anxiety |
| Szende & Németh (2000) [45] | 2000 | Hungary | EQ-VAS | survey was part of the National Health Survey conducted on a representative sample of members of the general population (n = 5503) | NA | NA | EQ-VAS = 70.4 |
| Zhao et al., (2020) [46] | 18–25 February 2020 | China | PSS-10 | non-diseased members of the general public in COVID-19 lockdown (n = 1630) | 29.17 ± 10.58 | NA | PSS-10 = 15.82 ± 5.56 |
| Hungarian Adult Participants n (%) | ||
|---|---|---|
| Gender | Male | 44 (10%) |
| Female | 387 (90%) | |
| Age | Mean ± SD | 47.53 ± 11.66 |
| Range | 18–73 years | |
| Marital status * | Single | 61 (14%) |
| Married/In a relationship | 291 (68%) | |
| Divorced | 54 (13%) | |
| Widowed | 18 (4%) | |
| Other | 1 (0.2%) | |
| Level of education * | Primary school (1–8 grades) | 5 (1.1%) |
| Vocational school (9–12 grades) | 34 (8%) | |
| High school (9–12 grades) | 53 (12%) | |
| Secondary school (9–12 grades) | 97 (23%) | |
| University, college | 226 (52%) | |
| PhD, DLA | 6 (1.4%) | |
| Other | 5 (1.1%) | |
| Employment status | Currently employed | 298 (69%) |
| Student | 5 (1%) | |
| On sick leave | 6 (1%) | |
| Retired | 72 (17%) | |
| Unemployed | 50 (12%) |
| Mean | SD | Range of Subscale | Average Percentage (Mean/Total Score of Subscale × 100) | |
|---|---|---|---|---|
| Problem analysis | 5.43 | 1.78 | 0–9 | 60 |
| Goal-oriented behavior | 5.78 | 2.78 | 0–12 | 48 |
| Emotion-based behavior | 3.13 | 2.35 | 0–12 | 26 |
| Adaptation | 4.92 | 1.82 | 0–12 | 41 |
| Asking for help | 2.64 | 1.42 | 0–6 | 44 |
| Seeking emotional balance | 2.8 | 1.35 | 0–6 | 47 |
| Withdrawal | 4.13 | 1.89 | 0–9 | 46 |
| Problem-focused coping | 11.21 | 3.90 | 0–21 | 53 |
| Emotion-focused coping | 17.62 | 5.24 | 0–45 | 39 |
| Perceived Stress | Level of Anxiety | Level of Depression | Health Status | Number of Complaints | Problem-Focused Coping | Emotion-Focused Coping | |
|---|---|---|---|---|---|---|---|
| Perceived stress | - | 0.821 ** | 0.778 ** | −0.448 ** | 0.626 ** | −0.330 ** | 0.400 ** |
| Level of anxiety | 0.821 ** | - | 0.753 ** | −0.399 ** | 0.544 ** | −0.240 ** | 0.357 ** |
| Level of depression | 0.778 ** | 0.753 ** | - | −0.416 ** | 0.501 ** | −0.243 ** | 0.329 ** |
| Health status | −0.448 ** | −0.399 ** | −0.416 ** | - | −0.496 ** | 0.210 ** | −0.195 ** |
| Number of complaints | 0.626 ** | 0.544 ** | 0.501 ** | −0.496 ** | - | −0.304 ** | 0.372 ** |
| Problem-focused coping | −0.330 ** | −0.240 ** | −0.243 ** | 0.210 ** | −0.304 ** | - | 0.161 ** |
| Emotion-focused coping | 0.400 ** | 0.357 ** | 0.329 ** | −0.195 ** | 0.372 ** | 0.161 ** | - |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Szabó, C.; Pukánszky, J.; Kemény, L. Psychological Effects of the COVID-19 Pandemic on Hungarian Adults. Int. J. Environ. Res. Public Health 2020, 17, 9565. https://0-doi-org.brum.beds.ac.uk/10.3390/ijerph17249565
Szabó C, Pukánszky J, Kemény L. Psychological Effects of the COVID-19 Pandemic on Hungarian Adults. International Journal of Environmental Research and Public Health. 2020; 17(24):9565. https://0-doi-org.brum.beds.ac.uk/10.3390/ijerph17249565
Chicago/Turabian StyleSzabó, Csanád, Judit Pukánszky, and Lajos Kemény. 2020. "Psychological Effects of the COVID-19 Pandemic on Hungarian Adults" International Journal of Environmental Research and Public Health 17, no. 24: 9565. https://0-doi-org.brum.beds.ac.uk/10.3390/ijerph17249565





