Association between Female Reproductive Health and Mancozeb: Systematic Review of Experimental Models
Abstract
:1. Introduction
2. Materials and Methods
2.1. Search Strategy
2.2. Search Terms
2.3. Inclusion and Exclusion Criteria
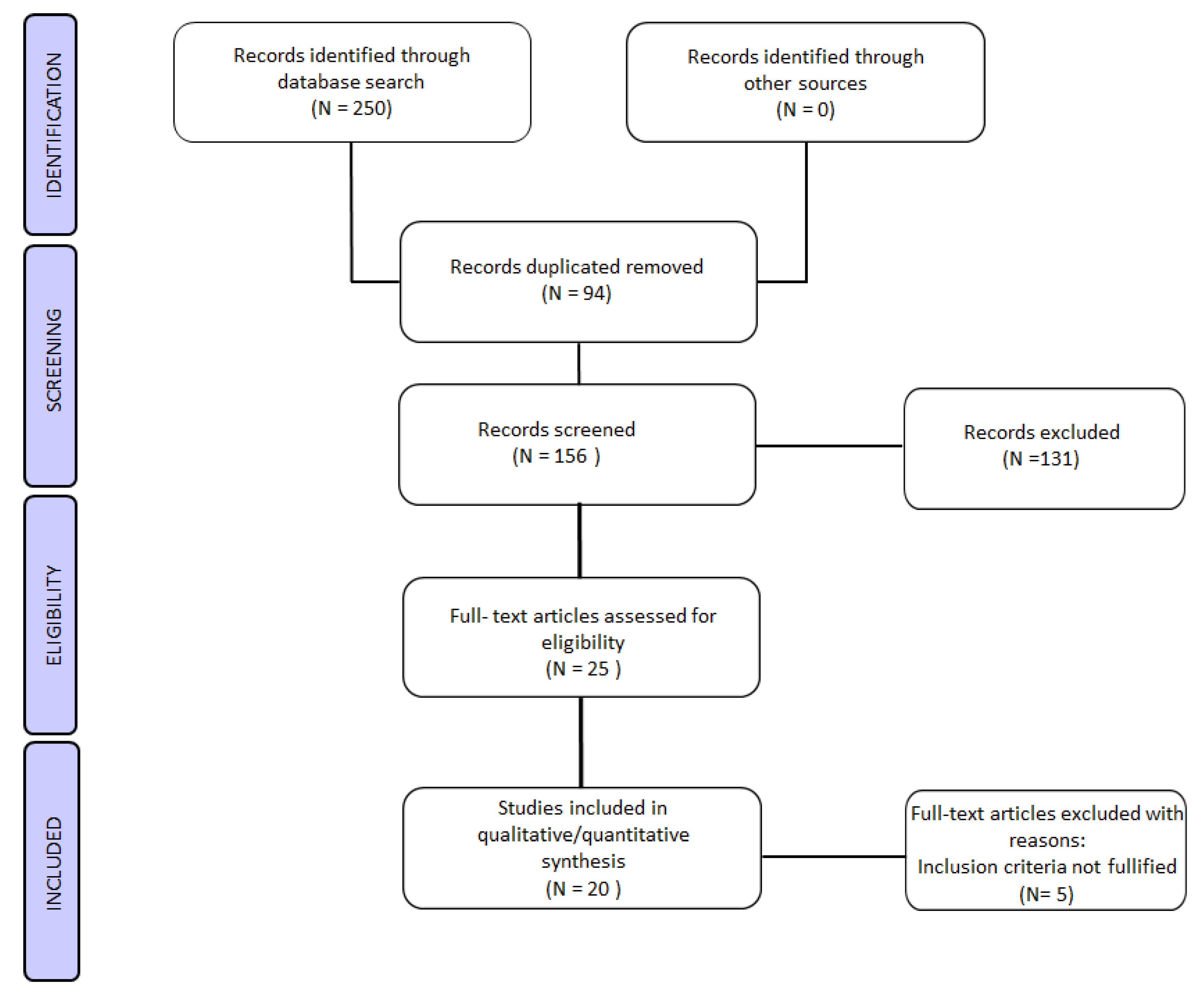
2.4. Study Selection
2.5. Data and Quality of Data Evaluation Strategy
3. Results
3.1. In Vitro Experimental Studies
3.2. In Vivo Experimental Studies
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Talmor, A.; Dunphy, B. Female obesity and infertility. Best Pr. Res. Clin. Obs. Gynaecol. 2015, 29, 498–506. [Google Scholar] [CrossRef]
- Nottola, S.A.; Macchiarelli, G.; Coticchio, G.; Bianchi, S.; Cecconi, S.; De Santis, L.; Scaravelli, G.; Flamigni, C.; Borini, A. Ultrastructure of human mature oocytes after slow cooling cryopreservation using different sucrose concentrations. Hum. Reprod. 2007, 22, 1123–1133. [Google Scholar] [CrossRef] [Green Version]
- Nottola, S.A.; Coticchio, G.; De Santis, L.; Macchiarelli, G.; Maione, M.; Bianchi, S.; Iaccarino, M.; Flamigni, C.; Borini, A. Ultrastructure of human mature oocytes after slow cooling cryopreservation with ethylene glycol. Reprod. Biomed. Online 2008, 17, 368–377. [Google Scholar] [CrossRef]
- Nottola, S.A.; Coticchio, G.; Sciajno, R.; Gambardella, A.; Maione, M.; Scaravelli, G.; Bianchi, S.; Macchiarelli, G.; Borini, A. Ultrastructural markers of quality in human mature oocytes vitrified using cryoleaf and cryoloop. Reprod. Biomed. Online 2009, 19, 17–27. [Google Scholar] [CrossRef]
- Khalili, M.A.; Maione, M.; Palmerini, M.G.; Bianchi, S.; Macchiarelli, G.; Nottola, S.A. Ultrastructure of human mature oocytes after vitrification. Eur. J. Histochem. 2012, 56, e38. [Google Scholar] [CrossRef]
- Bianchi, S.; Macchiarelli, G.; Micara, G.; Linari, A.; Boninsegna, C.; Aragona, C.; Rossi, G.; Cecconi, S.; Nottola, S.A. Ultrastructural markers of quality are impaired in human metaphase II aged oocytes: A comparison between reproductive and in vitro aging. J. Assist. Reprod. Genet. 2015, 32, 1343–1358. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Giusti, I.; Bianchi, S.; Nottola, S.A.; Macchiarelli, G.; Dolo, V. Clinical electron microscopy in the study of human ovarian tissues. Euromediterranean Biomed. J. 2019, 14, 145–151. [Google Scholar]
- Conforti, A.; Mascia, M.; Cioffi, G.; De Angelis, C.; Coppola, G.; De Rosa, P.; Pivonello, R.; Alviggi, C.; De Placido, G. Air pollution and female fertility: A systematic review of literature. Reprod. Biol. Endocrinol. 2018, 16, 117. [Google Scholar] [CrossRef]
- National Collaborating Centre for Ws, Children’s H. National Institute for Health and Clinical Excellence: Guidance. Fertility: Assessment and Treatment for People with Fertility Problems; Royal College of Obstetricians & Gynaecologists National Collaborating Centre for Women’s and Children’s Health: London, UK, 2013. [Google Scholar]
- D’Argenio, V.; Nunziato, M.; D’Uonno, N.; Borrillo, F.; Vallone, R.; Conforti, A. Indications and limitations for preimplantation genetic diagnosis. Biochim. Clin. 2017, 41, 314–321. [Google Scholar]
- Mahalingaiah, S.; Hart, J.E.; Laden, F.; Farland, L.V.; Hewlett, M.M.; Chavarro, J.; Aschengrau, A.; Missmer, S.A. Adult air pollution exposure and risk of infertility in the Nurses’ Health Study II. Hum. Reprod. 2016, 3, 638–647. [Google Scholar] [CrossRef] [PubMed]
- Nieuwenhuijsen, M.J.; Basagaña, X.; Dadvand, P.; Martinez, D.; Cirach, M.; Beelen, R.; Jacquemin, B. Air pollution and human fertility rates. Environ. Int. 2014, 70, 9–14. [Google Scholar] [CrossRef] [PubMed]
- Merklinger-Gruchala, A.; Jasienska, G.; Kapiszewska, M. Effect of air pollution on menstrual cycle length-a prognostic factor of women’s reproductive health. Int. J. Environ. Res. Public Health 2017, 14, 816. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Nobles, C.J.; Schisterman, E.F.; Ha, S.; Buck Louis, G.M.; Sherman, S.; Mendola, P. Time-varying cycle average and daily variation in ambient air pollution and fecundability. Hum. Reprod. 2018, 33, 166–176. [Google Scholar] [CrossRef] [PubMed]
- Chiang, C.; Mahalingam, S.; Flaws, J.A. Environmental Contaminants Affecting Fertility and Somatic Health. Semin. Reprod. Med. 2017, 35, 241–249. [Google Scholar] [CrossRef]
- Annamalai, J.; Namasivayam, V. Endocrine disrupting chemicals in the atmosphere: Their effects on humans and wildlife. Environ. Int. 2015, 76, 78–97. [Google Scholar] [CrossRef]
- Bianchi, S.; Bernardi, S.; Belli, M.; Varvara, G.; Macchiarelli, G. Exposure to persistent organic pollutants during tooth formation: Molecular mechanisms and clinical findings. Rev. Environ. Health 2020. [Google Scholar] [CrossRef]
- Chevrier, C.; Warembourg, C.; Gaudreau, E.; Monfort, C.; Le Blanc, A.; Guldner, L.; Cordier, S. Organochlorine pesticides, polychlorinated biphenyls, seafood consumption, and time-to-pregnancy. Epidemiology 2013, 24, 251–260. [Google Scholar] [CrossRef]
- Rattan, S.; Zhou, C.; Chiang, C.; Mahalingam, S.; Brehm, E.; Flaws, J.A. Exposure to endocrine disruptors during adulthood: Consequences for female fertility. J. Endocrinol. 2017, 233, R109–R129. [Google Scholar] [CrossRef] [Green Version]
- Sifakis, S.; Androutsopoulos, V.P.; Tsatsakis, A.M.; Spandidos, D.A. Human exposure to endocrine disrupting chemicals: Effects on the male and female reproductive systems. Environ. Toxicol. Pharm. 2017, 51, 56–70. [Google Scholar] [CrossRef] [PubMed]
- Runkle, J.; Flocks, J.; Economos, J.; Dunlop, A.L. A systematic review of Mancozeb as a reproductive and developmental hazard. Environ. Int. 2017, 99, 29–42. [Google Scholar] [CrossRef]
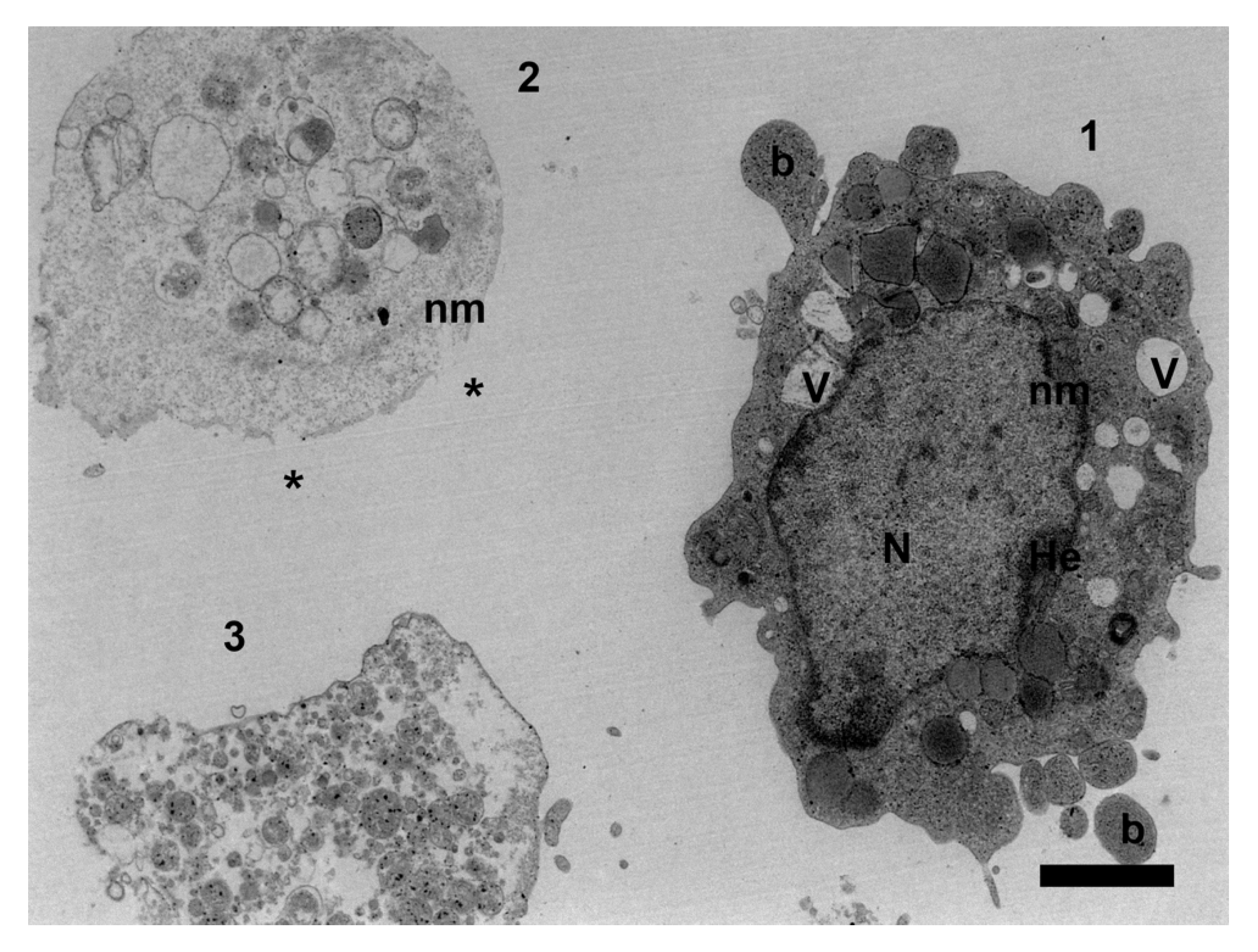
- Palmerini, M.G.; Belli, M.; Nottola, S.A.; Miglietta, S.; Bianchi, S.; Bernardi, S.; Antonouli, S.; Cecconi, S.; Familiari, G.; Macchiarelli, G. Mancozeb impairs the ultrastructure of mouse granulosa cells in a dose-dependent manner. J. Reprod. Dev. 2018, 64, 75–82. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Goldner, W.S.; Sandler, D.P.; Yu, F.; Hoppin, J.A.; Kamel, F.; Levan, T.D. Pesticide use and thyroid disease among women in the agricultural health study. Am. J. Epidemiol. 2010, 171, 455–464. [Google Scholar] [CrossRef]
- EPA Environmental Protection Agency; Mancozeb Reregistration Eligibility Decision (RED). Available online: https://www.federalregister.gov/documents/2005/12/28/05-24465/mancozeb-reregistration-eligibility-decision (accessed on 28 December 2005).
- Paro, R.; Tiboni, G.M.; Buccione, R.; Rossi, G.; Cellini, V.; Canipari, R.; Cecconi, S. The fungicide mancozeb induces toxic effects on mammalian granulosa cells. Toxicol. Appl. Pharm. 2012, 260, 155–161. [Google Scholar] [CrossRef] [PubMed]
- Srivastava, A.K.; Ali, W.; Singh, R.; Bhui, K.; Tyagi, S.; Al-Khedhairy, A.A.; Srivastava, P.K.; Musarrat, J.; Shukla, Y. Mancozeb-induced genotoxicity and apoptosis in cultured human lymphocytes. Life Sci. 2012, 90, 815–824. [Google Scholar] [CrossRef]
- Moher, D.; Altman, D.G.; Liberati, A.; Tetzlaff, J.; Altman, D.G.; PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. PLoS Med. 2009, 6, e1000097. [Google Scholar]
- Rooney, A.A.; Boyles, A.L.; Wolfe, M.S.; Bucher, J.R.; Thayer, K.A. Systematic review and evidence integration for literature-based environmental health science assessments. Environ. Health Perspect. 2014, 122, 711–718. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- National toxicology Program, U.S. Department of Health and Human Services. Handbook for Conducting a Literature-Based Health Assessment. Available online: https://ntp.niehs.nih.gov/ntp/ohat/pubs/handbookjan2015_508.pdf (accessed on 9 January 2015).
- Using OHAT Approach for Systematic Review and Evidence Integration. National Institute of Environmental Health Sciences, National Toxicology Program, Office of Health Assessment and Translation (OHAT). Available online: http://ntp.niehs.nih.gov/ntp/ohat/pubs/handbookjan2015_508.pdf (accessed on 9 January 2015).
- Fejes, S.; Budai, P.; Várnagy, L.; Molnár, T.; Szabó, R.; Fáncsi, T. Toxicity of a mancozeb containing fungicide formulation and CU-sulphate to chicken embryos after administration as single compounds or in combination. Meded. Rijksuniv Gent. Fak. Landbouwkd. Toegep. Biol. Wet. 2002, 67, 105–109. [Google Scholar] [PubMed]
- Greenlee, A.R.; Ellis, T.M.; Berg, R.L. Low-dose agrochemicals and lawn-care pesticides induce developmental toxicity in murine preimplantation embryos. Environ. Health Perspect. 2004, 112, 703–709. [Google Scholar] [CrossRef] [PubMed]
- Abdoon, A.S.S.; Kandil, O.M.; Sabraa, R.M.; Said, A.A. Effect of direct exposure to mancozeb fungicide on the developmental competnce of buffalo Oocytes in vitro. Glob. Vet. 2011, 7, 242–248. [Google Scholar]
- Iorio, R.; Castellucci, A.; Rossi, G.; Cinque, B.; Cifone, M.G.; Macchiarelli, G.; Cecconi, S. Mancozeb affects mitochondrial activity, redox status and ATP production in mouse granulosa cells. Toxicol. Vitr. 2015, 30, 438–445. [Google Scholar] [CrossRef]
- Atmaca, N.; Arikan, S.; Essiz, D.; Kalender, H.; Simsek, O.; Bilmen, F.S.; Kabakci, R. Effects of mancozeb, metalaxyl and tebuconazole on steroid production by bovine luteal cells in vitro. Environ. Toxicol. Pharm. 2018, 59, 114–118. [Google Scholar] [CrossRef]
- Khera, K.S. Ethylenethiourea: Teratogenicity study in rats and rabbits. Teratology 1973, 7, 243–252. [Google Scholar] [CrossRef]
- Castro, V.L.; Tambasco, A.J.; Paraíba, L.C.; Tambasco, D.D. Cytogenetic and teratological effects of mancozeb pre natal exposure on rats. Braz. Arch. Biol. Technol. 1999, 42. [Google Scholar] [CrossRef] [Green Version]
- Mahadevaswami, M.P.; Jadaramkunti, U.C.; Hiremath, M.B.; Kaliwal, B.B. Effect of mancozeb on ovarian compensatory hypertrophy and biochemical constituents in hemicastrated albino rat. Reprod. Toxicol. 2000, 14, 127–134. [Google Scholar] [CrossRef]
- Baligar, P.N.; Kaliwal, B.B. Induction of gonadal toxicity to female rats after chronic exposure to mancozeb. Ind. Health 2001, 39, 235–243. [Google Scholar] [CrossRef] [PubMed]
- Baligar, P.N.; Kaliwal, B.B. Morphometric Analysis of Follicular Growth and Biochemical Constituents in Albino Rats Exposed to Mancozeb. J. Basic. Clin. Physiol. Pharm. 2004, 15, 241–262. [Google Scholar] [CrossRef] [PubMed]
- Rossi, G.; Buccione, R.; Baldassarre, M.; Macchiarelli, G.; Palmerini, M.G.; Cecconi, S. Mancozeb exposure in vivo impairs mouse oocyte fertilizability. Reprod. Toxicol. 2006, 21, 216–219. [Google Scholar] [CrossRef]
- Hass, U.; Boberg, J.; Christiansen, S.; Jacobsen, P.R.; Vinggaard, A.M.; Taxvig, C.; Poulsen, M.E.; Herrmann, S.S.; Jensen, B.H.; Petersen, A.; et al. Adverse effects on sexual development in rat offspring after low dose exposure to a mixture of endocrine disrupting pesticides. Reprod Toxicol. 2012, 34, 261–274. [Google Scholar] [CrossRef]
- Jacobsen, P.R.; Axelstad, M.; Boberg, J.; Isling, L.K.; Christiansen, S.; Mandrup, K.R.; Berthelsen, L.O.; Vinggaard, A.M.; Hass, U. Persistent developmental toxicity in rat offspring after low dose exposure to a mixture of endocrine disrupting pesticides. Reprod. Toxicol. 2012, 34, 237–250. [Google Scholar] [CrossRef]
- Jacobsen, P.R.; Christiansen, S.; Boberg, J.; Nellemann, C.; Hass, U. Combined exposure to endocrine disrupting pesticides impairs parturition, causes pup mortality and affects sexual differentiation in rats. Int. J. Androl. 2010, 33, 434–442. [Google Scholar] [CrossRef] [PubMed]
- Liu, Y.; Wang, Y.L.; He, S.W.; Chen, M.H.; Zhang, Z.; Fu, X.P.; Fu, B.B.; Liao, B.Q.; Lin, Y.H.; Qi, Z.Q.; et al. Protective effects of resveratrol against mancozeb induced apoptosis damage in mouse oocytes. Oncotarget 2017, 8, 6233–6245. [Google Scholar] [CrossRef] [Green Version]
- Cuomo, D.; Porreca, I.; Ceccarelli, M.; Threadgill, D.W.; Barrington, W.T.; Petriella, A.; D’Angelo, F.; Cobellis, G.; De Stefano, F.; D’Agostino, M.N.; et al. Transcriptional landscape of mouse-aged ovaries reveals a unique set of non-coding RNAs associated with physiological and environmental ovarian dysfunctions. Cell Death Discov. 2018, 8, 6233–6245. [Google Scholar] [CrossRef]
- Mahdi, H.; Tahereh, H.; Esmaiel, S.; Massood, E. Vitamins E and C prevent apoptosis of testicular and ovarian tissues following mancozeb exposure in the first-generation mouse pups. Toxicol. Ind. Health 2019, 35, 136–144. [Google Scholar] [CrossRef]
- Esmaiel, S.; Tahereh, H.; Noreddin, N.M.S.; Massood, E. Mancozeb exposure during development and lactation periods results in decreased oocyte maturation, fertilization rates, and implantation in the first-generation mice pups: Protective effect of vitamins E and C. Toxicol. Ind. Health 2019, 35, 714–725. [Google Scholar] [CrossRef] [PubMed]
- Cosentino, K.; García-Sáez, A.J. Mitochondrial alterations in apoptosis. Chem. Phys. Lipids 2014, 181, 62–75. [Google Scholar] [CrossRef] [PubMed]
- Ishii, M.; Yamauchi, T.; Matsumoto, K.; Watanabe, G.; Taya, K.; Chatani, F. Maternal age and reproductive function in female Sprague-Dawley rats. J. Toxicol. Sci. 2012, 37, 631–638. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Maranghi, F.; De Angelis, S.; Tassinari, R.; Chiarotti, F.; Lorenzetti, S.; Moracci, G.; Marcoccia, D.; Gilardi, E.; Di Virgilio, A.; Eusepi, A.; et al. Reproductive toxicity and thyroid effects in Sprague Dawley rats exposed to low doses of ethylenethiourea. Food Chem. Toxicol. 2013, 59, 261–271. [Google Scholar] [CrossRef] [PubMed]
- Shukla, Y.; Arora, A. Transplacental carcinogenic potential of the carbamate fungicide mancozeb. J. Environ. Pathol. Toxicol. Oncol. 2001, 20, 127–131. [Google Scholar] [CrossRef]
- Oskarsson, A.; Hallén, I.P.; Sundberg, J. Exposure to toxic elements via breast milk. Analyst 1995, 120, 765–770. [Google Scholar] [CrossRef]
- Mora, A.M.; Córdoba, L.; Cano, J.C.; Hernandez-Bonilla, D.; Pardo, L.; Schnaas, L.; Smith, D.R.; Menezes-Filho, J.A.; Mergler, D.; Lindh, C.H.; et al. Prenatal mancozeb exposure, excess manganese, and neurodevelopment at 1 year of age in the infants’ environmental health (ISA) study. Envron. Health Perspect. 2018, 126, 057007. [Google Scholar] [CrossRef] [Green Version]
- EPA Federal Register, Rules and Regulations Mancozeb. Pesticide Tolerances. Available online: https://www.federalregister.gov/documents/2013/07/24/2013-17869/mancozeb-pesticide-tolerances (accessed on 24 July 2013).
| Level of Confidence for Health Effects | ||
|---|---|---|
| ++++ | High Confidence | Association between substance exposure and the outcome. The true effect is highly likely to be reflected in the apparent relationship. |
| +++ | Moderate Confidence | Association between substance exposure and the outcome. The true effect may be reflected in the apparent relationship. |
| ++ | Low Confidence | Association between substance exposure and the outcome. The true effect may be different from the apparent relationship. |
| + | Very Low Confidence | Association between substance exposure and the outcome. The true effect is highly likely to be different from the apparent relationship. |
| Author (Year) | Type of Cell/Tissue | Compound (Daily Dose) | Incubation | Outcomes | Confidence |
|---|---|---|---|---|---|
| Fejes et al. (2002) | 288 chicken embryos | 80% mancozeb containing formulation (dithane M-45) | 19 days | No toxic effect on embryos. Increased mortality in embryos in combination mixtures. | ++ |
| Greenlee et al. (2004) | Mice embryos | Low-doses of agrochemicals mancozeb (0.003 µg/mL) | 96 h | Reduced development of mouse blastocysts. Increased apoptosis during blastocyst formation | +++ |
| Abdoon et al. (2011) | Buffalo oocytes | Mancozeb (1.0, 2.5, and 5.0 µg/mL) | 24 h | In vitro maturation: mancozeb affects cytoplasmic and nuclear maturation. Dose-dependent oocyte degeneration. Fragmented cytoplasm and broken zona pellucida. In vitro fertilization: lower embryo development to morula and blastocyst stage. Fragmented and degenerated cytoplasm in all the exposed embryos. | +++ |
| Paro et al. (2012) | Mouse granulosa cells | Increasing concentrations of mancozeb (0.001–1 µg/mL) | 1, 24, and 36 h | Mouse: morphology changes; migration pattern; p53 reduced expression; no changes in apoptosis. Human: morphology changes; p53 reduced expression. | ++++ |
| Iorio et al. (2015) | Mouse granulosa cells | Mancozeb (0.01 µg/mL) | 36 h | p53 reduced expression. Depolarized mitochondrial membrane potential. Decreased ATP levels. Decreased glutathione levels (GSH). Increased reactive oxygen species (ROS). | ++++ |
| Palmerini et al. (2018) | Mouse granulosa cells | Increasing concentrations of mancozeb (0.001, 0.01, 0.1, and 1 µg/mL) | 36 h | Dose-dependent toxicity of mancozeb on mouse granulosa cells. | ++++ |
| Atmaca et al. (2018) | Bovine luteal cells | Mancozeb (0.01, 0.1, and 1 µM) | 4 days | Mancozeb exposure (1 µM) induces a significant decline (day 3 and 5) in steroidogenesis, compared to controls. | +++ |
| Author (Year) | Experimental Animal | n | Compound (Route) | Daily Dose | Duration | Outcomes | Ratings |
|---|---|---|---|---|---|---|---|
| Khera et al. (1973) | Adult nulliparous female Wistar rats, New Zealand White rabbits | 209 rats, 33 rabbits | Ethylene thiourea (ETU; oral) | 0, 5, 10, 20, 40, or 80 mg/kg/day | Rats Group 1: 21–42 (before gestation), 1–15 days (gestation) Group 2: 6–15 (gestation) Group 3: 7–20 days (gestation) Rabbits: 30 days (gestation) | No changes in the number of viable fetuses or in fetal death. 80 mg/kg of ETU have no significant effect before and during pregnancy. | ++++ |
| Castro et al. (1999) | Wister rats | 120 | Mancozeb (mixed in diet) | 0, 2000–3000 ppm | Group A: 1–6 (gestation days) Group B: 6–15 (gestation days) | No changes in estrous cycle during pregnancy. No changes in the number of live pup births. | +++ |
| Mahadevaswami et al. (2000) | Female Wistar virgin rats | 36 | Mancozeb (oral) | 500, 600, 700, and 800 mg/kg/day | 15 (before gestation days) | Decrease in ovary enlargement (700 and 800 mg/kg/day). No changes in estrous cycle (500 mg/kg/day). Decline in health follicle counts and a defective ovarian follicle rise (800 mg/kg/day). | ++++ |
| Baligar et Kaliwal (2001) | Wister virgin rats | 40 | Mancozeb (oral) | 500, 600, 700, and 800 mg/kg/day | 30 days | Decline in number of estrous cycle and healthy follicles, with changes in proestrus, estrus. and metestrus phases. | +++ |
| Baligar et Kaliwal (2004) | Female virgin albino rats | 70 | Mancozeb (75% wettable powder, olive oil; oral) | 700 mg/kg/day | 5, 10, 20, or 30 days (before gestation) | Alteration in diestrus and estrous cycle. Decline of healthy follicle numbers. Atretic follicles increase. | +++ |
| Rossi et al. (2006) | Swiss CD-1 female mice | 25 | Mancozeb (sesame oil; oral) | 50 and 500 mg/kg | Gestation day 2, pup day 20 | Eggs decline (ovulation) and fertilizability decreases. | +++ |
| Hass et al. (2012) | Nulliparous time-mated young adult female Wistar rats | 198 | Mancozeb (mixture composition; gavage) | 6.25 and 25 mg/kg/day | 7–21 (gestation day) 1–16 (pup day) | Longer gestation period (highest concentration). | ++++ |
| Jacobsen et al. (2012) | Nulliparous time-mated young adult female Wistar rats | 198 | Mancozeb (mixture composition; gavage) | 6.25 and 25 mg/kg/day | Gestation day 7, pup day 16 | No reproductive organ weight alterations (uterus and ovary). | ++++ |
| Jacobsen et al. (2010) | Nulliparous time-mated young adult female Wistar rats | 80 | Mancozeb (mixture composition; gavage) | 6.25, 12.5, 18.75, 25.0, and 31.25 mg/kg/day | Gestation day 7–day before expected birth (GD21) | Higher perinatal pup mortality and impaired parturition. | ++++ |
| Liu et al. (2017) | CD-1 mice (4–6 weeks old) | 240 | Mancozeb (oral) | 800 mg/kg/day | 4 weeks | Mancozeb reduces litter size and weight. Decreased ovary weight. Increased atretic follicles and decreased normal oocytes. Ultrastructural alterations in GV oocytes. Decrease in the number of pronuclei and two-cells of parthenogenetic activated oocytes. Changes in actin expression levels. Increase in apoptosis and in ROS production. Abnormal mitochondrial distribution and mitochondrial membrane alterations. Epigenetic modifications. | ++++ |
| Cuomo et al. (2018) | CD-1 mice | 20 | Ethylene thiourea (ETU; drinking water) | 0.1, 1, and 10 mg/kg/day | From conception (through mothers) to postnatal 21 days. | ETU influences ovarian aging biomarkers at all doses. | ++++ |
| Mahdi et al. (2019) | First-generation (F1) mouse female pups | 36 | Mancozeb (oral gavage) | 500 mg/kg | From day 2 of pregnancy to postnatal 20 days. | Apoptotic follicles. Remarkable germ cells depletion in gonads. | ++++ |
| Esmaiel et al. (2019) | First-generation (F1) female pups | 60 | Mancozeb (oral gavage) | 500 mg/kg (olive oil; mothers) | From day 2 of pregnancy to postnatal 21 days. | Reduction of number of collected oocyte. Comprised oocyte maturation, fertilization, implantation, and fecundity rate. Comprised embryo development. | ++++ |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bianchi, S.; Nottola, S.A.; Torge, D.; Palmerini, M.G.; Necozione, S.; Macchiarelli, G. Association between Female Reproductive Health and Mancozeb: Systematic Review of Experimental Models. Int. J. Environ. Res. Public Health 2020, 17, 2580. https://0-doi-org.brum.beds.ac.uk/10.3390/ijerph17072580
Bianchi S, Nottola SA, Torge D, Palmerini MG, Necozione S, Macchiarelli G. Association between Female Reproductive Health and Mancozeb: Systematic Review of Experimental Models. International Journal of Environmental Research and Public Health. 2020; 17(7):2580. https://0-doi-org.brum.beds.ac.uk/10.3390/ijerph17072580
Chicago/Turabian StyleBianchi, Serena, Stefania Annarita Nottola, Diana Torge, Maria Grazia Palmerini, Stefano Necozione, and Guido Macchiarelli. 2020. "Association between Female Reproductive Health and Mancozeb: Systematic Review of Experimental Models" International Journal of Environmental Research and Public Health 17, no. 7: 2580. https://0-doi-org.brum.beds.ac.uk/10.3390/ijerph17072580





