Psychosocial Impact of Assistive Devices and Other Technologies on Deaf and Hard of Hearing People
Abstract
:1. Introduction
2. Materials and Methods
2.1. Participants
2.2. Procedure
2.3. Instruments
2.3.1. Psychosocial Impact of Assistive Devices Scale (PIADS)
2.3.2. Matching Person and Technology (MPT)
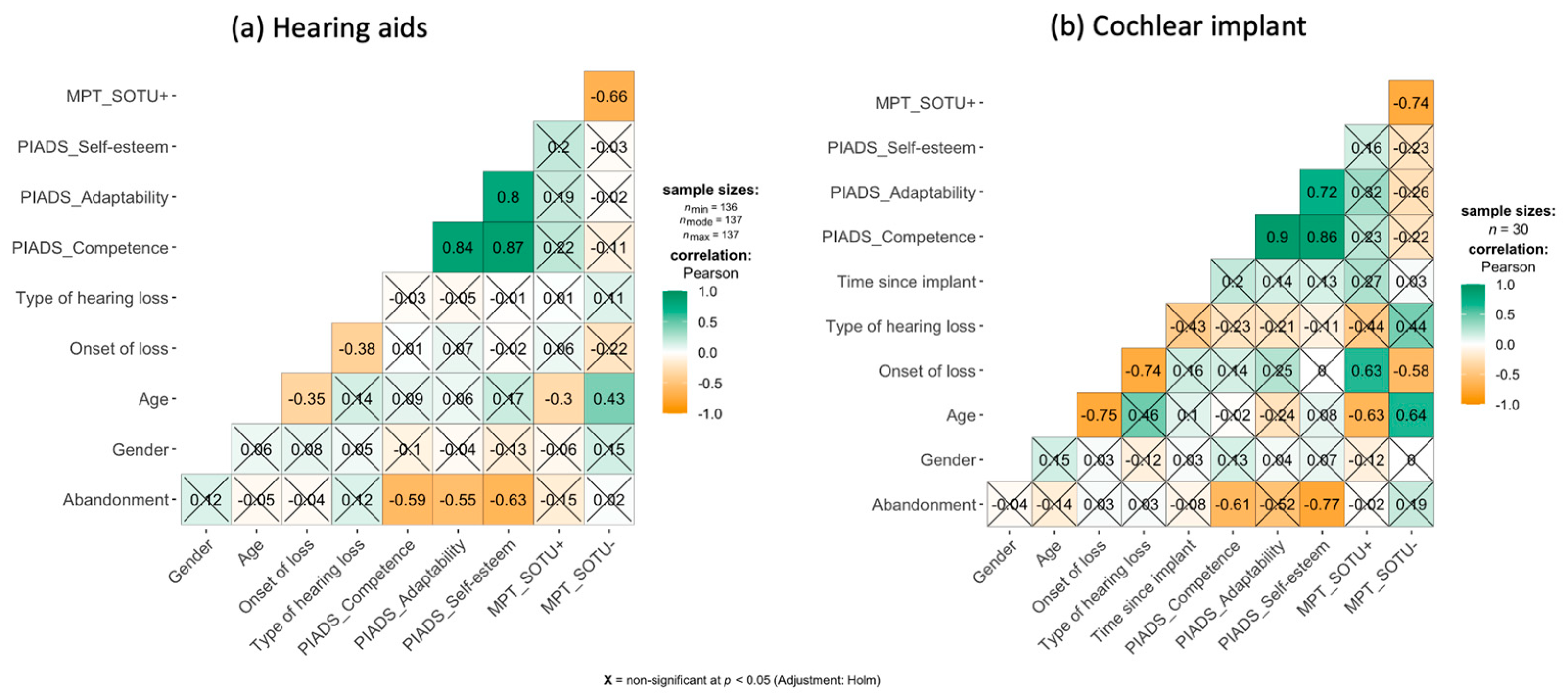
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- World Health Organization Deafness and Hearing Loss. Available online: https://www.who.int/news-room/fact-sheets/detail/deafness-and-hearing-loss (accessed on 2 May 2021).
- World Health Organization. World Report on Hearing; World Health Organization: Geneva, Switzerland, 2021. [Google Scholar]
- Laplante-Lévesque, A.; Hickson, L.; Worrall, L. Factors Influencing Rehabilitation Decisions of Adults with Acquired Hearing Impairment. Int. J. Audiol. 2010, 49, 497–507. [Google Scholar] [CrossRef]
- Upfold, L.J.; May, A.E.; Battaglia, J.A. Hearing Aid Manipulation Skills in an Elderly Population: A Comparison of ITE, BTE, and ITC Aids. Br. J. Audiol. 1990, 24, 311–318. [Google Scholar] [CrossRef]
- Zhang, F.; Underwood, G.; McGuire, K.; Liang, C.; Moore, D.R.; Fu, Q.-J. Frequency Change Detection and Speech Perception in Cochlear Implant Users. Hear. Res. 2019, 379, 12–20. [Google Scholar] [CrossRef]
- Federal Communications Commission Video Relay Services. Available online: https://www.fcc.gov/consumers/guides/video-relay-services (accessed on 2 May 2021).
- Maiorana-Basas, M.; Pagliaro, C.M. Technology Use Among Adults Who Are Deaf and Hard of Hearing: A National Survey. J. Deaf Stud. Deaf Educ. 2014, 19, 400–410. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mantokoudis, G.; Dähler, C.; Dubach, P.; Kompis, M.; Caversaccio, M.D.; Senn, P. Internet Video Telephony Allows Speech Reading by Deaf Individuals and Improves Speech Perception by Cochlear Implant Users. PLoS ONE 2013, 8, e54770. [Google Scholar] [CrossRef] [Green Version]
- Mantokoudis, G.; Koller, R.; Guignard, J.; Caversaccio, M.; Kompis, M.; Senn, P. Influence of Telecommunication Modality, Internet Transmission Quality, and Accessories on Speech Perception in Cochlear Implant Users. J. Med. Internet Res. 2017, 19, e135. [Google Scholar] [CrossRef]
- Aazh, H.; Moore, B.C.J. Audiological Rehabilitation for Facilitating Hearing Aid Use: A Review. J. Am. Acad. Audiol. 2017, 28, 248–260. [Google Scholar] [CrossRef] [PubMed]
- Cox, R.M.; Alexander, G.C. The Abbreviated Profile of Hearing Aid Benefit. Ear Hear. 1995, 16, 176–186. [Google Scholar] [CrossRef]
- Cox, R.M.; Alexander, G.C. Measuring Satisfaction with Amplification in Daily Life: The SADL Scale. Ear Hear. 1999, 20, 306–320. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Day, H.; Jutai, J. Measuring the Psychosocial Impact of Assistive Devices: The PIADS. Can. J. Rehabil. 1996, 9, 159–168. [Google Scholar]
- Saladin, S.P.; Hansmann, S.E. Psychosocial Variables Related to the Adoption of Video Relay Services Among Deaf or Hard-of-Hearing Employees at the Texas School for the Deaf. Assist. Technol. 2008, 20, 36–47. [Google Scholar] [CrossRef] [PubMed]
- Saunders, G.H.; Jutai, J.W. Hearing Specific and Generic Measures of the Psychosocial Impact of Hearing Aids. J. Am. Acad. Audiol. 2004, 15, 238–248. [Google Scholar] [CrossRef] [Green Version]
- Eklund, K.; Dahlin-Ivanoff, S. Low Vision, ADL and Hearing Assistive Device Use among Older Persons with Visual Impairments. Disabil. Rehabil. Assist. Technol. 2007, 2, 326–334. [Google Scholar] [CrossRef] [PubMed]
- Harris, F.; Sprigle, S. Outcomes Measurement of a Wheelchair Intervention. Disabil. Rehabil. Assist. Technol. 2008, 3, 171–180. [Google Scholar] [CrossRef]
- Sineva, E.L.; Fedina, I.N.; Preobrazhenskaia, E.A. Topical problems of occupational deafness. Med. Tr. Prom. Ekol. 2007, 34–39. [Google Scholar]
- Werngren-Elgström, M.; Iwarsson, S.; Elmståhl, S.; Dehlin, O. ADL Dependence and Perceived Health among Elderly Deaf Sign-Language Users: A Comparison with a Matched Group of Elderly Hearing People. Scand. J. Occup. Ther. 2005, 12, 81–88. [Google Scholar] [CrossRef]
- World Health Organization. Improving Access to Assistive Technology. Report by the Director-General; World Health Organization: Geneva, Switzerland, 2018; p. 6. [Google Scholar]
- Cox, R.M.; Alexander, G.C. Expectations about Hearing Aids and Their Relationship to Fitting Outcome. J. Am. Acad. Audiol. 2000, 11, 368–382, quiz 407. [Google Scholar]
- Wielandt, T.; Strong, J. Compliance with Prescribed Adaptive Equipment: A Literature Review. Br. J. Occup. Ther. 2000, 63, 65–75. [Google Scholar] [CrossRef]
- Guerra-Zúñiga, M.; Cardemil-Morales, F.; Albertz-Arévalo, N.; Rahal-Espejo, M. Explicaciones al no uso de audífonos en un grupo de adultos mayores de Santiago de Chile. Un estudio cualitativo. Acta Otorrinolaringológica Española 2014, 65, 8–14. [Google Scholar] [CrossRef]
- Chen, S.; Karamy, B.; Shipp, D.; Nedzelski, J.; Chen, J.; Lin, V. Assessment of the Psychosocial Impacts of Cochlear Implants on Adult Recipients and Their Partners. Cochlear Implant. Int. 2016, 17, 90–97. [Google Scholar] [CrossRef] [PubMed]
- Kochkin, S.; Rogin, M. Quantifying the Obvious: The Impact of Hearing Instruments on Quality of Life. Hear. Rev. 2000, 7, 6–30. [Google Scholar]
- Mulrow, C.D. Quality-of-Life Changes and Hearing Impairment: A Randomized Trial. Ann. Intern. Med. 1990, 113, 188. [Google Scholar] [CrossRef]
- Tomita, M.; Mann, W.C.; Welch, T.R. Use of Assistive Devices to Address Hearing Impairment by Older Persons with Disabilities. Int. J. Rehabil. Res. 2001, 24, 279–290. [Google Scholar] [CrossRef] [PubMed]
- Jutai, J.; Bortolussi, J. Psychosocial impact of assistive technology: Development of a measure for children. In Assistive Technology–Shaping the Future; Craddock, G.M., McCormack, L.P., Reilly, R.B., Knops, H.T.P., Eds.; IOS Press: Amsterdam, The Netherlands, 2003; pp. 936–940. [Google Scholar]
- Coryell, J.; Holcomb, T.K.; Scherer, M. Attitudes Toward Deafness: A Collegiate Perspective. Am. Ann. Deaf 1992, 137, 299–302. [Google Scholar] [CrossRef]
- Deal, M. Disabled People’s Attitudes toward Other Impairment Groups: A Hierarchy of Impairments. Disabil. Soc. 2003, 18, 897–910. [Google Scholar] [CrossRef]
- Erler, S.F.; Garstecki, D.C. Hearing Loss- and Hearing Aid-Related Stigma: Perceptions of Women with Age-Normal Hearing. Am. J. Audiol. 2002, 11, 83–91. [Google Scholar] [CrossRef]
- Götherström, U.-C.; Persson, J.; Jonsson, D. A Socioeconomic Model for Evaluation of Postal and Telecommunication Services for Disabled Persons. Technol. Disabil. 2004, 16, 91–99. [Google Scholar] [CrossRef]
- Mann, W.; Hurren, D.; Tomita, M. Assistive Device Needs of Home-Based Elderly Persons with Hearing Impairments. Technol. Disabil. 1994, 3, 47–61. [Google Scholar]
- Salomon, G.; Vesterager, V.; Jagd, M. Age-Related Hearing Difficulties: I. Hearing Impairment, Disability, and Handicap—A Controlled Study. Int. J. Audiol. 1988, 27, 164–178. [Google Scholar] [CrossRef]
- Scherer, M.J. Outcomes of Assistive Technology Use on Quality of Life. Disabil. Rehabil. 1996, 18, 439–448. [Google Scholar] [CrossRef] [PubMed]
- Gopinath, B.; Schneider, J.; Hartley, D.; Teber, E.; McMahon, C.M.; Leeder, S.R.; Mitchell, P. Incidence and Predictors of Hearing Aid Use and Ownership Among Older Adults With Hearing Loss. Ann. Epidemiol. 2011, 21, 497–506. [Google Scholar] [CrossRef] [PubMed]
- Southall, K.; Gagné, J.-P.; Leroux, T. Factors That Influence the Use of Assistance Technologies by Older Adults Who Have a Hearing Loss: Factores Que Influyen En El Uso de Tecnologías de Asistencia En Adultos Mayores Con Hipoacusia. Int. J. Audiol. 2006, 45, 252–259. [Google Scholar] [CrossRef]
- Day, H.; Jutai, J.; Woolric, W.; Strong, G. The Stability of Impact of Assistive Devices. Disabil. Rehabil. 2001, 23, 400–404. [Google Scholar] [CrossRef] [PubMed]
- Tamblay, N.N.; Villalobos, A.I.; Pastene, G.A.; Rahal, E.M. Impacto Social Del Uso de Audífonos En Adultos Mayores. Rev. Otorrinolaringol. Cir. Cabeza Cuello 2008, 68, 21–26. [Google Scholar] [CrossRef]
- Polgar, J. The myth of neutral technology. In Design and Use of Assistive Technology; Oishi, M.K., Mitchell, I.M., Van der Loos, F.H.M., Eds.; Springer: Berlin/Heidelberg, Germany, 2010; pp. 17–23. [Google Scholar]
- Humes, L.E.; Wilson, D.L.; Humes, A.C. Examination of Differences between Successful and Unsuccessful Elderly Hearing Aid Candidates Matched for Age, Hearing Loss and Gender: Evaluación de Las Diferencias Entre Los Candidatos Exitosos y No Exitosos de Edad Mayor, al Uso de Auxiliar Auditivo Por Edad, Grado de Hipoacusia y Sexo. Int. J. Audiol. 2003, 42, 432–441. [Google Scholar] [CrossRef] [PubMed]
- Kricos, P.B.; Erdman, S.; Bratt, G.W.; Williams, D.W. Psychosocial Correlates of Hearing Aid Adjustment. J. Am. Acad. Audiol. 2007, 18, 304–322. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Jutai, J.; Day, H. Psychosocial Impact of Assistive Devices Scale (PIADS). Technol. Disabil. 2002, 14, 107–111. [Google Scholar] [CrossRef]
- Day, H.; Jutai, J. The Psychosocial Impact of Assistive Devices Scale (PIADS) [Manual]; University of Western Ontario: London, ON, Canada, 1996. [Google Scholar]
- Jutai, J.; Ladak, N.; Schuller, R.; Naumann, S.; Wright, V. Outcomes Measurement of Assistive Technologies: An Institutional Case Study. Assist. Technol. 1996, 8, 110–120. [Google Scholar] [CrossRef]
- Quinteiro, M.V.Q. Impacto de Las Ayudas Técnicas de Acceso al Ordenador en el Aprendizaje de Materias Informáticas Mediante Cursos de Enseñanza Asistida por Ordenador (E.A.O) de Alumnos con Discapacidad en los MIEMBROS Superiores. [Impact of Assistive Technology for Computer Access on the Learning of Computer Subjects through Computer-Assisted Learning (C.A.T.) Courses for Students with Disabilities in the Upper Limbs.]. UNED. Madrid: Universidad Nacional de Educación a Distancia (España). 2010. Available online: https://dialnet.unirioja.es/descarga/tesis/22601.pdf (accessed on 10 December 2020).
- Saunders, G.H.; Lewis, M.S.; Forsline, A. Expectations, Prefitting Counseling, and Hearing Aid Outcome. J. Am. Acad. Audiol. 2009, 20, 320–334. [Google Scholar] [CrossRef] [PubMed]
- Scherer, M.J. Matching Person & Technology. A Series of Assessments for Evaluating Predispositions to and Outcomes of Technology Use in Rehabilitation, Education, the Workplace & Other Settings; The Institute for Matching Person & Technology, Inc.: Webster, NY, USA, 1998. [Google Scholar]
- Zhang, Z. Variable Selection with Stepwise and Best Subset Approaches. Ann. Transl. Med. 2016, 4, 136. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Billari, S.L. Outcome Assessment of Audient Foundation Hearing Aids at the James Madison University Clinic. Ph.D. Thesis, James Madison University, Harrisonburg, VA, USA, 2009. [Google Scholar]
- Boi, R.; Racca, L.; Cavallero, A.; Carpaneto, V.; Racca, M.; Dall’ Acqua, F.; Ricchetti, M.; Santelli, A.; Odetti, P. Hearing Loss and Depressive Symptoms in Elderly Patients: Hearing Aids in Elderly with Depression. Geriatr. Gerontol. Int. 2012, 12, 440–445. [Google Scholar] [CrossRef]
- Chisolm, T.H.; Noe, C.M.; McArdle, R.; Abrams, H. Evidence for the Use of Hearing Assistive Technology by Adults: The Role of the FM System. Trends Amplif. 2007, 11, 73–89. [Google Scholar] [CrossRef] [Green Version]
- Helvik, A.-S.; Jacobsen, G.; Hallberg, L.R.-M. Psychological Well-Being of Adults with Acquired Hearing Impairment. Disabil. Rehabil. 2006, 28, 535–545. [Google Scholar] [CrossRef] [PubMed]
- Lockey, K.; Jennings, M.B.; Shaw, L. Exploring Hearing Aid Use in Older Women through Narratives. Int. J. Audiol. 2010, 49, 542–549. [Google Scholar] [CrossRef]
- Solheim, J.; Kværner, K.J.; Falkenberg, E.-S. Daily Life Consequences of Hearing Loss in the Elderly. Disabil. Rehabil. 2011, 33, 2179–2185. [Google Scholar] [CrossRef] [Green Version]
- Huarte, A.; Lezaun, R.; Manrique, M. Quality of Life Outcomes for Cochlear Implantation in the Elderly. Audiol. Neurotol. 2014, 19, 36–39. [Google Scholar] [CrossRef]
- Olze, H.; Szczepek, A.J.; Haupt, H.; Zirke, N.; Graebel, S.; Mazurek, B. The Impact of Cochlear Implantation on Tinnitus, Stress and Quality of Life in Postlingually Deafened Patients. Audiol. Neurotol. 2012, 17, 2–11. [Google Scholar] [CrossRef] [PubMed]
- Park, E.; Shipp, D.B.; Chen, J.M.; Nedzelski, J.M.; Lin, V.Y.W. Postlingually Deaf Adults of All Ages Derive Equal Benefits from Unilateral Multichannel Cochlear Implant. J. Am. Acad. Audiol. 2011, 22, 637–643. [Google Scholar] [CrossRef] [PubMed]
- De Sousa, A.F.; Couto, M.I.V.; Martinho-Carvalho, A.C. Quality of Life and Cochlear Implant: Results in Adults with Postlingual Hearing Loss. Braz. J. Otorhinolaryngol. 2018, 84, 494–499. [Google Scholar] [CrossRef]
- Klop, W.M.C.; Boermans, P.P.B.M.; Ferrier, M.B.; van den Hout, W.B.; Stiggelbout, A.M.; Frijns, J.H.M. Clinical Relevance of Quality of Life Outcome in Cochlear Implantation in Postlingually Deafened Adults. Otol. Neurotol. 2008, 29, 615–621. [Google Scholar] [CrossRef] [Green Version]
- Zhao, F.; Bai, Z.; Stephens, D. The Relationship between Changes in Self-Rated Quality of Life after Cochlear Implantation and Changes in Individual Complaints. Clin. Otolaryngol. 2008, 33, 427–434. [Google Scholar] [CrossRef]
- Di Nardo, W.; Anzivino, R.; Giannantonio, S.; Schinaia, L.; Paludetti, G. The Effects of Cochlear Implantation on Quality of Life in the Elderly. Eur. Arch. Otorhinolaryngol. 2014, 271, 65–73. [Google Scholar] [CrossRef] [PubMed]
- Yang, Z.; Cosetti, M. Safety and Outcomes of Cochlear Implantation in the Elderly: A Review of Recent Literature. J. Otol. 2016, 11, 1–6. [Google Scholar] [CrossRef] [Green Version]
- Rekkedal, A.M. Assistive Hearing Technologies Among Students With Hearing Impairment: Factors That Promote Satisfaction. J. Deaf Stud. Deaf Educ. 2012, 17, 499–517. [Google Scholar] [CrossRef] [Green Version]
- Kobosko, J.; Jedrzejczak, W.W.; Gos, E.; Geremek-Samsonowicz, A.; Ludwikowski, M.; Skarzynski, H. Self-Esteem in the Deaf Who Have Become Cochlear Implant Users as Adults. PLoS ONE 2018, 13, e0203680. [Google Scholar] [CrossRef] [PubMed]
- Kobosko, J.; Jedrzejczak, W.W.; Barej, A.; Pankowska, A.; Geremek-Samsonowicz, A.; Skarzynski, H. Cochlear Implants in Adults with Partial Deafness: Subjective Benefits but Associated Psychological Distress. Eur. Arch. Otorhinolaryngol. 2021, 278, 1387–1394. [Google Scholar] [CrossRef]
- McCormack, A.; Fortnum, H. Why Do People Fitted with Hearing Aids Not Wear Them? Int. J. Audiol. 2013, 52, 360–368. [Google Scholar] [CrossRef] [Green Version]
- Summerfield, A.Q.; Marshall, D.H. Non-Use of Cochlear Implants by Post-Lingually Deafened Adults. Cochlear Implant. Int. 2000, 1, 18–38. [Google Scholar] [CrossRef]
- Knopke, S.; Gräbel, S.; Förster-Ruhrmann, U.; Mazurek, B.; Szczepek, A.J.; Olze, H. Impact of Cochlear Implantation on Quality of Life and Mental Comorbidity in Patients Aged 80 Years: CI and HRQoL in Elderly Patients. Laryngoscope 2016, 126, 2811–2816. [Google Scholar] [CrossRef]
- Kobosko, J.; Pankowska, A.; Skarżyński, H. Strategie Radzenia Sobie Ze Stresem u Osób Dorosłych Postlingwalnie Ogłuchłych Korzystających z Implantu Ślimakowego, w Porównaniu z Populacją Ogólną Słyszących. Otolaryngol. Polska 2012, 66, 132–137. [Google Scholar] [CrossRef]
- Claesen, E.; Pryce, H. An Exploration of the Perspectives of Help-Seekers Prescribed Hearing Aids. Prim. Health Care Res. Dev. 2012, 13, 279–284. [Google Scholar] [CrossRef] [PubMed]
- Salehomoum, M. Cochlear Implant Nonuse: Insight from Deaf Adults. J. Deaf Stud. Deaf Educ. 2020, 25, 270–282. [Google Scholar] [CrossRef] [PubMed]
- Lauer, A.; Longenecker, R.K.; Smith, R.O. ATOMS Project Technical Report—Factors in Assistive Technology Device Abandonment: Replacing “Abandonment” with “Discontinuance.”. 2006. Available online: www.r2d2.uwm.edu/atoms/archive/technicalreports/tr-discontinuance.html (accessed on 30 June 2017).
- Pape, T.L.-B.; Kim, J.; Weiner, B. The Shaping of Individual Meanings Assigned to Assistive Technology: A Review of Personal Factors. Disabil. Rehabil. 2002, 24, 5–20. [Google Scholar] [CrossRef] [PubMed]
- Verza, R.; Carvalho, M.L.; Battaglia, M.A.; Uccelli, M.M. An Interdisciplinary Approach to Evaluating the Need for Assistive Technology Reduces Equipment Abandonment. Mult. Scler. 2006, 12, 88. [Google Scholar] [CrossRef]
- Wong, L.L.N.; Hickson, L.; McPherson, B. Hearing Aid Satisfaction: What Does Research from the Past 20 Years Say? Trends Amplif. 2003, 7, 117–161. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Vestergaard Knudsen, L.; Öberg, M.; Nielsen, C.; Naylor, G.; Kramer, S.E. Factors Influencing Help Seeking, Hearing Aid Uptake, Hearing Aid Use and Satisfaction With Hearing Aids: A Review of the Literature. Trends Amplif. 2010, 14, 127–154. [Google Scholar] [CrossRef] [Green Version]
- Kobosko, J.; Jedrzejczak, W.W.; Pilka, E.; Pankowska, A.; Skarzynski, H. Satisfaction With Cochlear Implants in Postlingually Deaf Adults and Its Nonaudiological Predictors: Psychological Distress, Coping Strategies, and Self-Esteem. Ear Hear. 2015, 36, 605–618. [Google Scholar] [CrossRef]
- Hosford-Dunn, H.; Halpern, J. Clinical Application of the SADL Scale in Private Practice II: Predictive Validity of Fitting Variables. Satisfaction with Amplification in Daily Life. J. Am. Acad. Audiol. 2001, 12, 15–36. [Google Scholar]
- Uriarte, M.; Denzin, L.; Dunstan, A.; Sellars, J.; Hickson, L. Measuring Hearing Aid Outcomes Using the Satisfaction with Amplification in Daily Life (SADL) Questionnaire: Australian Data. J. Am. Acad. Audiol. 2005, 16, 383–402. [Google Scholar] [CrossRef] [Green Version]
- Díez, E.; Jiménez-Arberas, E.; Pousada, T. Psychometric Properties of the Spanish Version of Psychosocial Impact of Assistive Devices Scale in a Large Sample of People With Neuromuscular, Neurological, or Hearing Disabilities. Front. Psychol. 2021, 12, 659562. [Google Scholar] [CrossRef]
- Fuhrer, M.J. Assistive Technology Outcomes Research: Challenges Met and Yet Unmet. Am. J. Phys. Med. Rehabil. 2001, 80, 528–535. [Google Scholar] [CrossRef]
- Tangcharoensathien, V.; Witthayapipopsakul, W.; Viriyathorn, S.; Patcharanarumol, W. Improving Access to Assistive Technologies: Challenges and Solutions in Low- and Middle-Income Countries. WHO South-East. Asia J. Public Health 2018, 7, 84. [Google Scholar] [CrossRef]
| Variable | N (%) |
|---|---|
| Age | M = 56.12; SD = 25.11 |
| Gender | |
| Male | 115 (39.5%) |
| Female | 176 (60.5%) |
| Language | |
| Sign language | 39 (13.4%) |
| Spoken language | 146 (50.2%) |
| Both | 106 (36.4%) |
| Residential area | |
| Rural | 60 (20.6%) |
| Urban | 231 (79.4%) |
| Onset of loss | |
| Prelocutive | 94 (32.3%) |
| Postlocutive | 197 (67.7%) |
| Type of loss | |
| Hypoacusis | 214 (73.5%) |
| Cophosis/Total hearing loss | 77 (26.5%) |
| PIADS | |||||
|---|---|---|---|---|---|
| n | Total | Competence | Adaptability | Self-Esteem | |
| Hearing aids (Spectacle, Deep-insertion, In-the-canal, Behind-the-ear) * | 137 | 1.39 (0.93) | 1.37 (0.92) | 1.41 (0.97) | 1.42 (1.09) |
| hypoacusis | 120 | 1.38 (0.94) | 1.35 (.93) | 1.39 (0.96) | 1.41 (1.02) |
| cophosis | 17 | 1.47 (0.91) | 1.45 (.88) | 1.54 (1.09) | 1.46 (1.04) |
| Cochlear implant | 30 | 1.47 (1.13) | 1.45 (1.16) | 1.47 (0.91) | 1.37 (1.28) |
| hypoacusis | 14 | 1.24 (1.02) | 1.17 (1.00) | 1.39 (1.11) | 1.22 (1.22) |
| cophosis | 16 | 1.68 (1.21) | 1.70 (1.26) | 1.88 (1.17) | 1.50 (1.40) |
| Information and Communication Technologies (mobile phone, ooVoo, Skype) | 58 | 0.63 (0.95) | 0.59 (0.94) | 0.84 (1.18) | 0.54 (0.97) |
| hypoacusis | 38 | 0.57 (0.83) | 0.48 (0.79) | 0.83 (1.05) | 0.49 (0.91) |
| cophosis | 20 | 0.76 (1.15) | 0.80 (1.17) | 0.86 (1.43) | 0.62 (1.09) |
| Video Relay Services | 66 | 1.34 (0.87) | 1.40 (0.89) | 1.61 (1.02) | 1.04 (1.02) |
| hypoacusis | 42 | 1.23 (0.77) | 1.38 (0.77) | 1.40 (0.96) | 0.88 (0.93) |
| cophosis | 24 | 1.52 (1.01) | 1.43 (1.09) | 1.98 (1.05) | 1.31 (1.12) |
| PIADS | |||||
|---|---|---|---|---|---|
| Abandonment | Total | Competence | Adaptability | Self-Esteem | |
| Hearing aids | NO (n = 102) | 1.67 (0.80) | 1.62 (0.81) | 1.66 (0.88) | 1.75 (0.9) |
| YES (n = 25) | 0.16 (0.25) | 0.23 (0.32) | 0.27 (0.45) | −0.40 (0.51) | |
| Spectacle | NO (n = 2) | 2.77 (0.11) | 2.79 (0.18) | 2.5 (0.7) | 2.94 (0.88) |
| Deep-insertion | YES (n = 1) | 0.42 | 0.16 | 0.5 | 0.75 |
| In-the-canal | NO (n = 29) YES (n = 7) | 1.59 (0.78) 0.42 (0.28) | 1.55 (0.84) 0.17 (0.3) | 1.55 (0.92) 0.50 (0.5) | 1.7 (0.84) 0.75 (0.5) |
| Behind-the-ear | NO (n = 76) YES (n = 17) | 1.68 (0.81) 0.11 (0.24) | 1.62 (0.81) 0.21 (0.32) | 1.7 (0.87) 0.23 (0.44) | 1.74 (0.95) −0.13 (0.5) |
| Cochlear implant | NO (n = 24) YES (n = 6) | 1.85 (0.88) −0.03 (0.67) | 1.80 (0.96) −0.07(0.79) | 1.94 (1.02) 0.47 (0.90) | 1.85 (0.89) −0.56 (0.53) |
| Best Model with AIC Criteria | Best Model with BIC Criteria | ||||
|---|---|---|---|---|---|
| Odds Ratio * | p | Odds Ratio | p | ||
| (Intercept) | 0.0004 | <0.001 | (Intercept) | ||
| Gender (female) | 4.22 | 0.11 | |||
| Onset (prelocutive) | 0.0003 | 0.18 | |||
| MPT_ SOTU (−) | 0.52 | 0.11 | |||
| Competence | 0.04 | <0.01 | Competence | 0.12 | <0.05 |
| Self-esteem | 0.03 | <0.01 | Self-esteem | 0.04 | <0.01 |
| Best Model with AIC Criteria | Best Model with BIC Criteria | ||||
|---|---|---|---|---|---|
| Odds Ratio * | p | Odds Ratio | p | ||
| (Intercept) | 0.001 | <0.001 | (Intercept) | 0.009 | <0.001 |
| Type of loss (hypoacusis) | 4.12 | 0.15 | |||
| Competence | 0.27 | 0.10 | |||
| Self-esteem | 0.01 | <0.001 | Self-esteem | 0.01 | <0.001 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Jiménez-Arberas, E.; Díez, E. Psychosocial Impact of Assistive Devices and Other Technologies on Deaf and Hard of Hearing People. Int. J. Environ. Res. Public Health 2021, 18, 7259. https://0-doi-org.brum.beds.ac.uk/10.3390/ijerph18147259
Jiménez-Arberas E, Díez E. Psychosocial Impact of Assistive Devices and Other Technologies on Deaf and Hard of Hearing People. International Journal of Environmental Research and Public Health. 2021; 18(14):7259. https://0-doi-org.brum.beds.ac.uk/10.3390/ijerph18147259
Chicago/Turabian StyleJiménez-Arberas, Estíbaliz, and Emiliano Díez. 2021. "Psychosocial Impact of Assistive Devices and Other Technologies on Deaf and Hard of Hearing People" International Journal of Environmental Research and Public Health 18, no. 14: 7259. https://0-doi-org.brum.beds.ac.uk/10.3390/ijerph18147259







