Dissemination of Aerosol and Splatter in Clinical Environment during Cavity Preparation: An In Vitro Study
Abstract
:1. Introduction
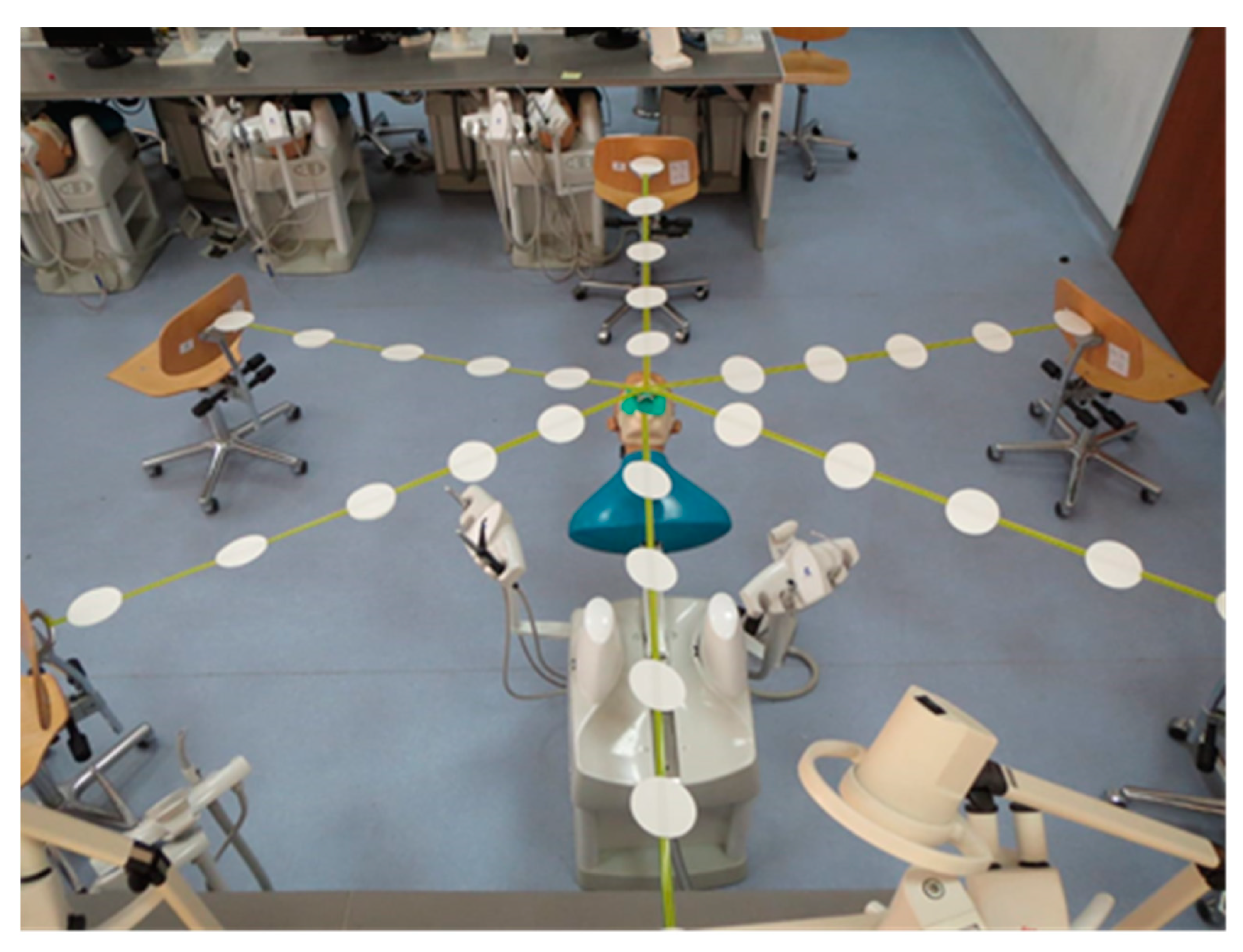
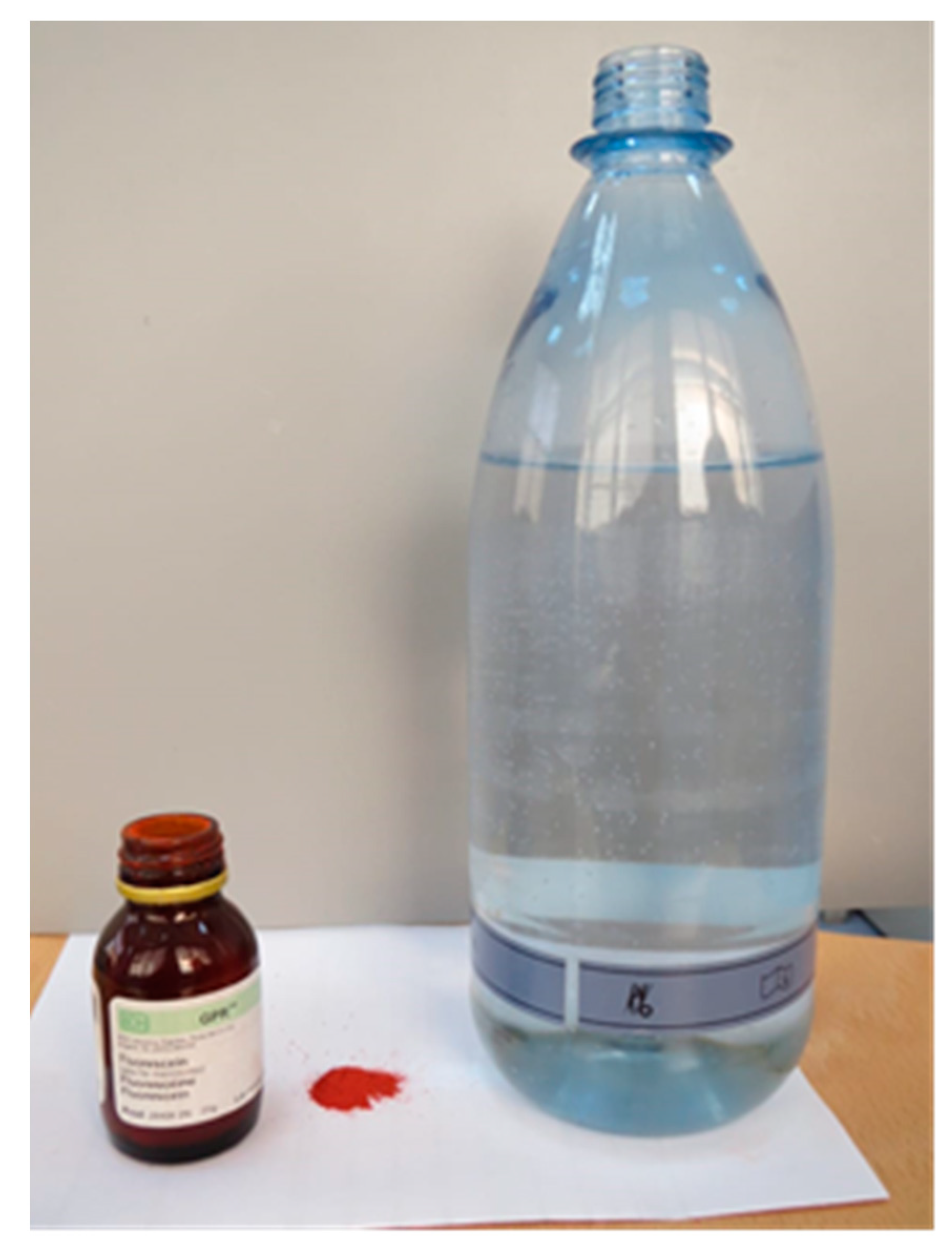
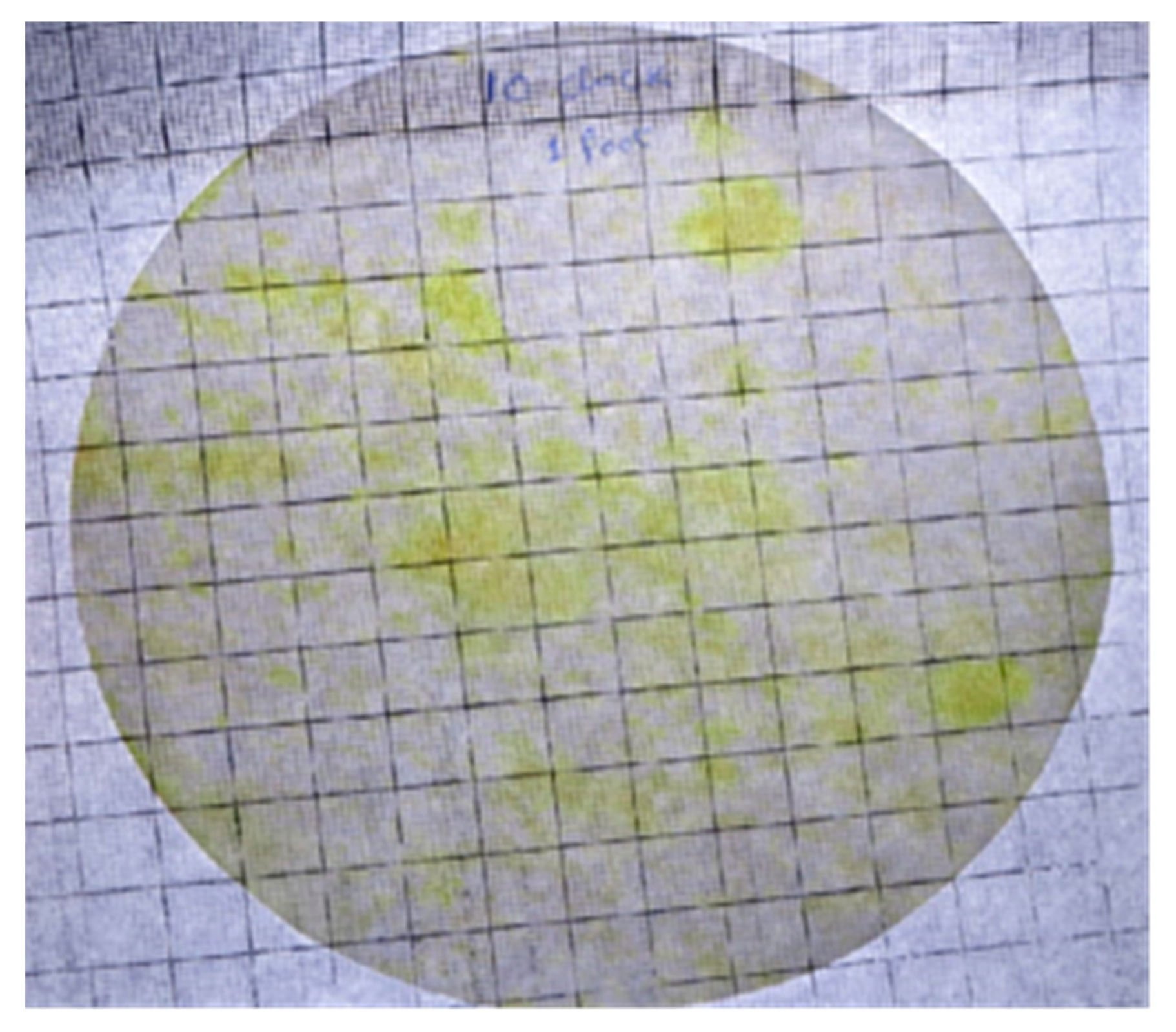
2. Materials and Methods
Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Shimoji, S.; Ishihama, K.; Yamada, H.; Okayama, M.; Yasuda, K.; Shibutani, T.; Ogasawara, T.; Miyazawa, H.; Furusawa, K. Occupational safety among dental health-care workers. Adv. Med. Educ. Pract. 2010, 1, 41–47. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Harrel, S.K.; Molinari, J. Aerosols and splatter in dentistry: A brief review of the literature and infection control implications. J. Am. Dent. Assoc. 2004, 135, 429–437. [Google Scholar] [CrossRef]
- Matys, J.; Grzech-Leśniak, K. Dental aerosol as a hazard risk for dental workers. Materials 2020, 13, 5109. [Google Scholar] [CrossRef]
- Veena, H.R.; Mahantesha, S.; Joseph, P.A.; Patil, S.R.; Patil, S.H. Dissemination of aerosol and splatter during ultrasonic scaling: A pilot study. J. Infect. Public Health 2015, 8, 260–265. [Google Scholar] [CrossRef] [PubMed]
- Ahmed, M.A.; Jouhar, R.; Adnan, S.; Ahmed, N.; Ghazal, T.; Adanir, N. Evaluation of Patient’s Knowledge, Attitude, and Practice of Cross-Infection Control in Dentistry during COVID-19 Pandemic. Eur. J. Dent. 2020, 14, S1–S6. [Google Scholar] [CrossRef] [PubMed]
- Rautemaa, R.; Nordberg, A.; Wuolijoki-Saaristo, K.; Meurman, J.H. Bacterial aerosols in dental practice—A potential hospital infection problem? J. Hosp. Infect. 2006, 64, 76–81. [Google Scholar] [CrossRef] [PubMed]
- Yang, M.; Chaghtai, A.; Melendez, M.; Hasson, H.; Whitaker, E.; Badi, M.; Sperrazza, L.; Godel, J.; Yesilsoy, C.; Tellez, M.; et al. Mitigating saliva aerosol contamination in a dental school clinic. BMC Oral Health 2021, 21. [Google Scholar] [CrossRef]
- Azim, A.A.; Shabbir, J.; Khurshid, Z.; Zafar, M.S.; Ghabbani, H.M.; Dummer, P.M.H. Clinical endodontic management during the COVID-19 pandemic: A literature review and clinical recommendations. Int. Endod. J. 2020, 53, 1461–1471. [Google Scholar] [CrossRef]
- Bhandary, N.; Desai, A.; Shetty, B.Y. High-Speed Handpiece. J. Am. Dent. Assoc. 1993, 124, 16. [Google Scholar] [CrossRef]
- Hailu, K.; Lawoyin, D.; Glascoe, A.; Jackson, A. Unexpected Hazards with Dental High Speed Drill. Dent. J. 2017, 5, 10. [Google Scholar] [CrossRef] [Green Version]
- Ravenel, T.D.; Kessler, R.; Comisi, J.C.; Kelly, A.; Renne, W.G.; Teich, S.T. Evaluation of the spatter-reduction effectiveness and aerosol containment of eight dry-field isolation techniques. Quintessence Int. 2020, 51, 2–12. [Google Scholar] [CrossRef]
- Jacks, M.E. A laboratory comparison of evacuation devices on aerosol reduction. J. Dent. Hyg. 2002, 76, 202–206. [Google Scholar] [PubMed]
- Setti, L.; Passarini, F.; De Gennaro, G.; Barbieri, P.; Perrone, M.G.; Borelli, M.; Palmisani, J.; Di Gilio, A.; Piscitelli, P.; Miani, A. Airborne transmission route of covid-19: Why 2 meters/6 feet of inter-personal distance could not be enough. Int. J. Environ. Res. Public Health 2020, 17, 2932. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ahmed, M.A.; Jouhar, R.; Ahmed, N.; Adnan, S.; Aftab, M.; Zafar, M.S.; Khurshid, Z. Fear and practice modifications among dentists to combat novel coronavirus disease (COVID-19) outbreak. Int. J. Environ. Res. Public Health 2020, 17, 2821. [Google Scholar] [CrossRef] [PubMed]
- Consolo, U.; Bellini, P.; Bencivenni, D.; Iani, C.; Checchi, V. Epidemiological aspects and psychological reactions to COVID-19 of dental practitioners in the Northern Italy districts of modena and reggio emilia. Int. J. Environ. Res. Public Health 2020, 17, 3459. [Google Scholar] [CrossRef] [PubMed]
- Tysiąc-Miśta, M.; Dziedzic, A. The attitudes and professional approaches of dental practitioners during the COVID-19 outbreak in poland: A cross-sectional survey. Int. J. Environ. Res. Public Health 2020, 17, 4703. [Google Scholar] [CrossRef] [PubMed]
- Mijiritsky, E.; Hamama-Raz, Y.; Liu, F.; Datarkar, A.N.; Mangani, L.; Caplan, J.; Shacham, A.; Kolerman, R.; Mijiritsky, O.; Ben-Ezra, M.; et al. Subjective overload and psychological distress among dentists during COVID-19. Int. J. Environ. Res. Public Health 2020, 17, 5074. [Google Scholar] [CrossRef]
- Sarapultseva, M.; Zolotareva, A.; Kritsky, I.; Nasretdinova, N.; Sarapultsev, A. Psychological distress and post-traumatic symptomatology among dental healthcare workers in Russia: Results of a pilot study. Int. J. Environ. Res. Public Health 2021, 18, 708. [Google Scholar] [CrossRef]
- Kumar, A.R.N.; Karumaran, S.C.; Kattula, D.; Thavarajah, R.; Anusa, A.M. Perceived stress and psychological (Dis)stress among indian endodontists during COVID19 pandemic lock down. MedRxiv 2020, 311, 1–19. [Google Scholar] [CrossRef]
- Dahiya, P.; Kamal, R.; Sharma, V.; Kaur, S. “Hepatitis”—Prevention and management in dental practice. J. Educ. Health Promot. 2015, 4, 33. [Google Scholar] [CrossRef]
- Sebastiani, F.R.; Dym, H.; Kirpalani, T. Infection Control in the Dental Office. Dent. Clin. North Am. 2017, 61, 435–457. [Google Scholar] [CrossRef]
- Kohn, W.G.; Harte, J.A.; Malvitz, D.M.; Collins, A.S.; Cleveland, J.L.; Eklund, K.J. Guidelines for infection control in dental health care settings—2003. J. Am. Dent. Assoc. 2004, 135, 33–47. [Google Scholar] [CrossRef] [PubMed]
- Bentley, C.D.; Burkhart, N.W.; Crawford, J.J. Evaluating spatter and aerosol contamination during dental procedures. J. Am. Dent. Assoc. 1994, 125, 579–584. [Google Scholar] [CrossRef] [PubMed]
- ADA Releases Interim Guidance on Minimizing COVID-19 Transmission Risk when Treating Dental Emergencies. Available online: https://www.ada.org/en/publications/ada-news/2020-archive/april/ada-releases-interim-guidance-on-minimizing-covid-19-transmission-risk-when-treating-emergencies (accessed on 3 April 2021).
- Llandro, H.; Allison, J.R.; Currie, C.C.; Edwards, D.C.; Bowes, C.; Durham, J.; Jakubovics, N.; Rostami, N.; Holliday, R. Evaluating splatter and settled aerosol during orthodontic debonding: Implications for the COVID-19 pandemic. Br. Dent. J. 2021. [Google Scholar] [CrossRef]
- Bennett, A.M.; Fulford, M.R.; Walker, J.T.; Bradshaw, D.J.; Martin, M.V.; Marsh, P.D. Microbial aerosols in general dental practice. Br. Dent. J. 2000, 189, 664–667. [Google Scholar] [CrossRef] [PubMed]
- Gandolfi, M.G.; Zamparini, F.; Spinelli, A.; Sambri, V.; Prati, C. Risks of aerosol contamination in dental procedures during the second wave of COVID-19—experience and proposals of innovative IPC in dental practice. Int. J. Environ. Res. Public Health 2020, 17, 8954. [Google Scholar] [CrossRef]
- Sarapultseva, M.; Hu, D.; Sarapultsev, A. SARS-CoV-2 Seropositivity among Dental Staff and the Role of Aspirating Systems. JDR Clin. Transl. Res. 2021, 6, 132–138. [Google Scholar] [CrossRef]
- Aurangjeb, A.M.; Zaman, T.; Badruddoza, M. Practice of Dental Surgeons about Dental Splatter and Aerosol. City Dent. Coll. J. 2013, 10, 10–16. [Google Scholar] [CrossRef] [Green Version]

| Distance | Contaminated Surface Area (cm2) | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Two-Hole Handpiece | Four-Hole Handpiece | |||||||||||
| 12 o’clock | 2 o’clock | 4 o’clock | 6 o’clock | 8 o’clock | 10 o’clock | 12 o’clock | 2 o’clock | 4 o’clock | 6 o’clock | 8 o’clock | 10 o’clock | |
| 12 inches | 63 | 71 | 41 | 55 | 60 | 74 | 59 | 60 | 36 | 48 | 55 | 70 |
| 24 inches | 49 | 58 | 19 | 38 | 28 | 53 | 40 | 54 | 10 | 29 | 30 | 45 |
| 36 inches | 15 | 30 | - | 19 | 13 | 22 | - | 23 | - | 11 | 12 | 27 |
| 48 inches | - | 11 | - | 4 | - | 10 | - | 5 | - | - | - | 7 |
| 60 inches | - | 4 | - | - | - | 3 | - | - | - | - | - | - |
| Mean | 25.4 | 34.8 | 12 | 23.2 | 20.2 | 32.4 | 19.8 | 28.4 | 9.2 | 17.6 | 19.4 | 29.8 |
| St. Dev | 29.02 | 29.09 | 18.17 | 23.2 | 25.06 | 30.12 | 27.93 | 27.55 | 15.59 | 20.71 | 23.38 | 28.56 |
| Body Part | Contaminated Surface Area (cm2) Operator | Contaminated Surface Area (cm2) Assistant |
|---|---|---|
| Head | 67 | 52 |
| Chest | 55 | 39 |
| Right arm | 91 | 19 |
| Left arm | 34 | 85 |
| Inside mask | 7 | 2 |
| Total | 254 | 197 |
| Distance | p-Value | Mean Difference | Std. Error Difference |
|---|---|---|---|
| 12 Inches | 0.398 | 6.00000 | 6.79379 |
| 24 Inches | 0.500 | 6.16667 | 8.81318 |
| 36 Inches | 0.498 | 4.33333 | 6.16532 |
| 48 Inches | 0.401 | 2.16667 | 2.46869 |
| 60 Inches | 0.150 | 1.16667 | 0.74907 |
| Handpieces | Distance | Time | Mean | St. Deviation | p-Value |
|---|---|---|---|---|---|
| Two holes | 12 inches | Post filling | 60.6667 | 11.91078 | 0.000 |
| After 30 min | 10.17 | 5.707 | |||
| 24 inches | Post filling | 40.8333 | 15.22388 | 0.001 | |
| After 30 min | 0.50 | 1.225 | |||
| 36 inches | Post filling | 16.5000 | 10.05485 | 0.010 | |
| After 30 min | 0.00 | 0.000 | |||
| 48 inches | Post filling | 4.1667 | 5.15429 | 0.105 | |
| After 30 min | 0.00 | 0.000 | |||
| 60 inches | Post filling | 1.1667 | 1.83485 | 0.180 | |
| After 30 min | 0.00 | 0.000 | |||
| Four holes | 12 inches | Post filling | 54.6667 | 11.62182 | 0.000 |
| After 30 min | 3.17 | 3.817 | |||
| 24 inches | Post filling | 34.6667 | 15.30577 | 0.003 | |
| After 30 min | 0.00 | 0.000 | |||
| 36 inches | Post filling | 12.1667 | 11.26795 | 0.046 | |
| After 30 min | 0.00 | 0.000 | |||
| 48 inches | Post filling | 2.0000 | 3.16228 | 0.182 | |
| After 30 min | 0.00 | 0.000 | |||
| 60 inches | Post filling | 0.0000 | 0.00000 | - | |
| After 30 min | 0.00 | 0.000 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ahmed, M.A.; Jouhar, R. Dissemination of Aerosol and Splatter in Clinical Environment during Cavity Preparation: An In Vitro Study. Int. J. Environ. Res. Public Health 2021, 18, 3773. https://0-doi-org.brum.beds.ac.uk/10.3390/ijerph18073773
Ahmed MA, Jouhar R. Dissemination of Aerosol and Splatter in Clinical Environment during Cavity Preparation: An In Vitro Study. International Journal of Environmental Research and Public Health. 2021; 18(7):3773. https://0-doi-org.brum.beds.ac.uk/10.3390/ijerph18073773
Chicago/Turabian StyleAhmed, Muhammad Adeel, and Rizwan Jouhar. 2021. "Dissemination of Aerosol and Splatter in Clinical Environment during Cavity Preparation: An In Vitro Study" International Journal of Environmental Research and Public Health 18, no. 7: 3773. https://0-doi-org.brum.beds.ac.uk/10.3390/ijerph18073773







