The Effect of Probiotics (MCP® BCMC® Strains) on Hepatic Steatosis, Small Intestinal Mucosal Immune Function, and Intestinal Barrier in Patients with Non-Alcoholic Fatty Liver Disease
Abstract
:1. Introduction
2. Methodology
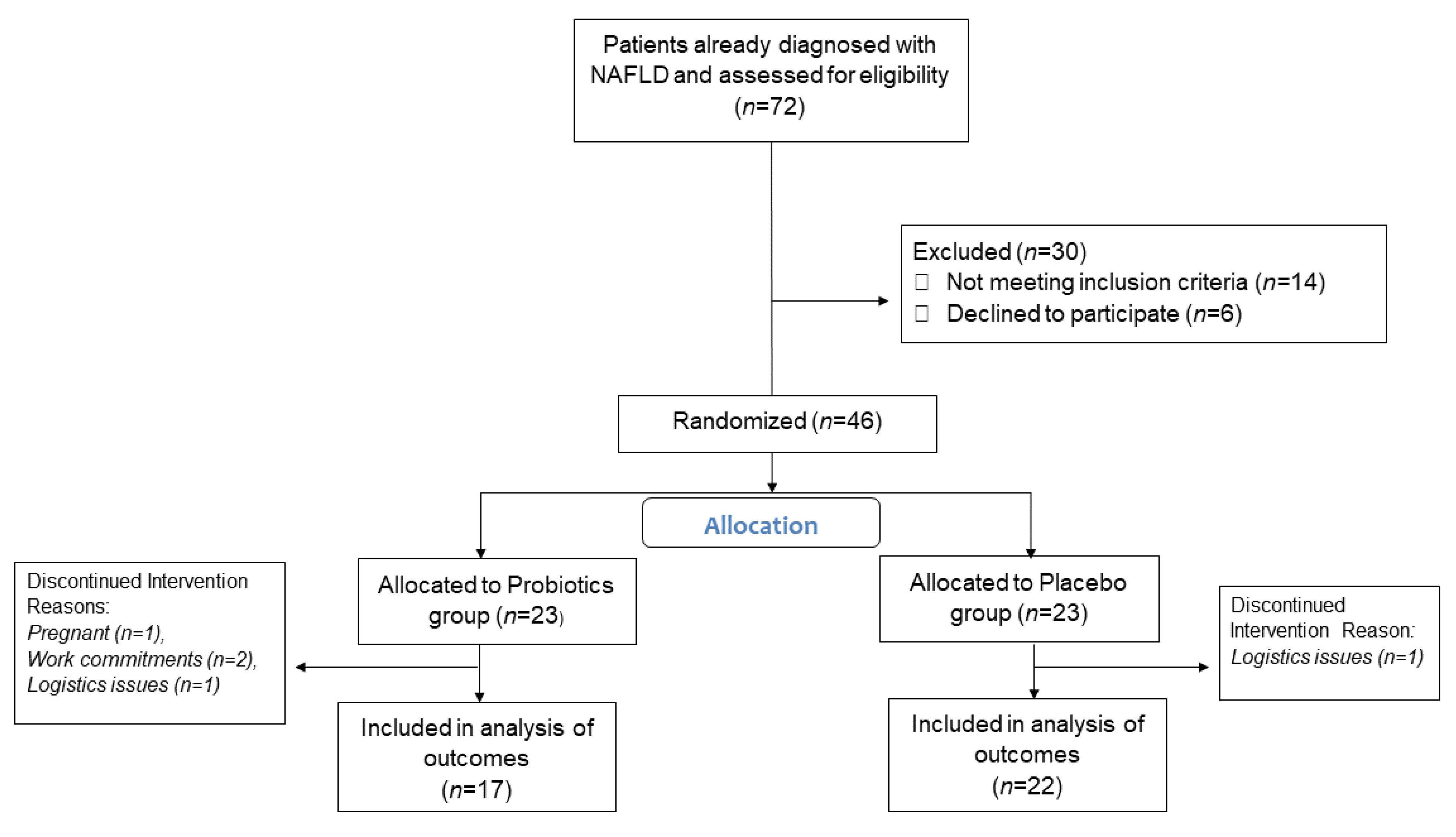
2.1. Study Design
2.2. Patient Recruitment
2.3. Clinical Assessment and Intervention
2.4. Laboratory Investigations
2.5. Immunohistochemistry Analysis
2.6. Transient Elastography
2.7. Probiotics and Compliance
2.8. Statistical Analysis
2.9. Primary and Secondary Outcomes
3. Results
3.1. Baseline Characteristics
3.2. Hepatic Steatosis, Fibrosis and Activity Scores
3.3. Biochemical Blood Tests
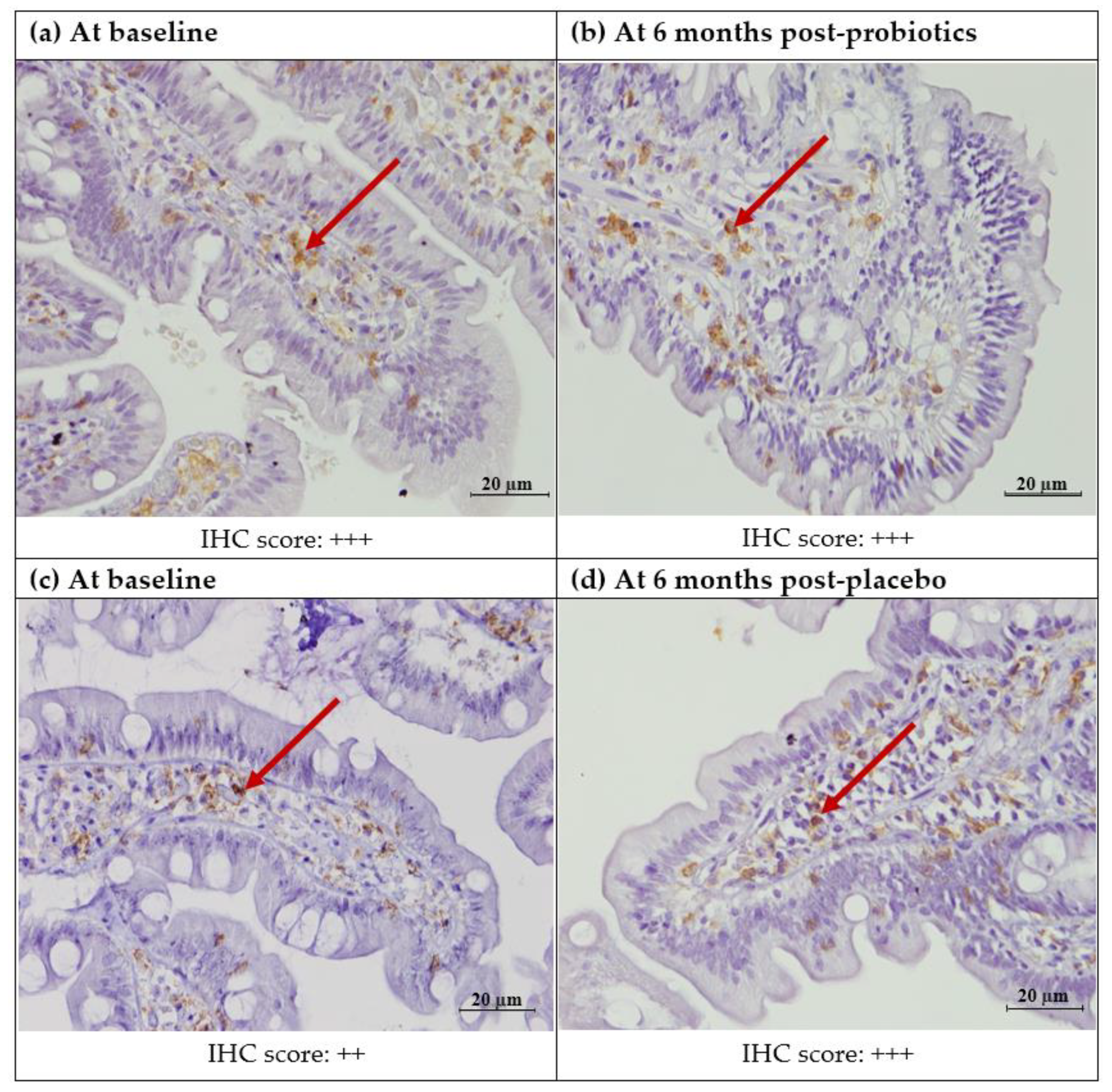
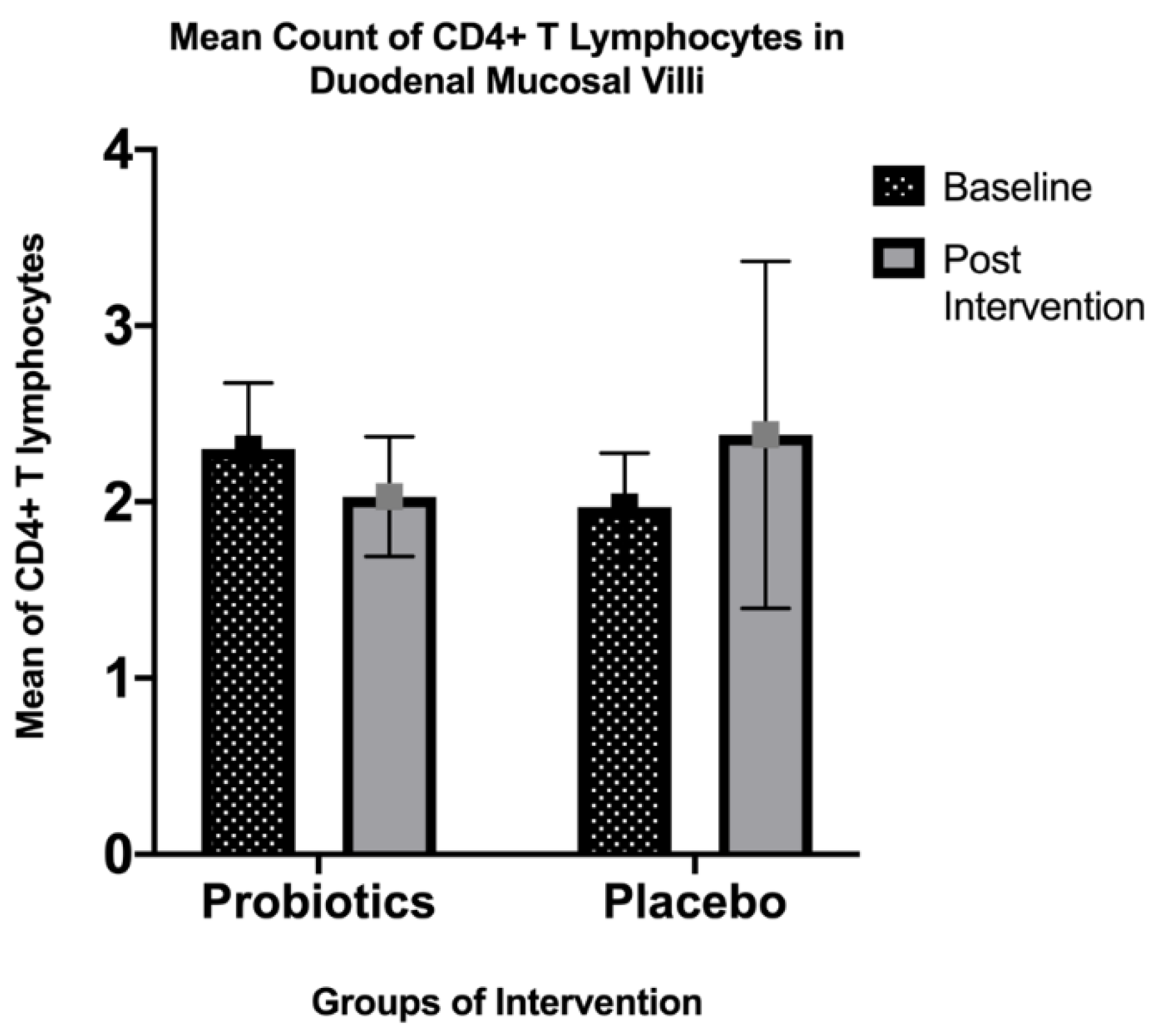
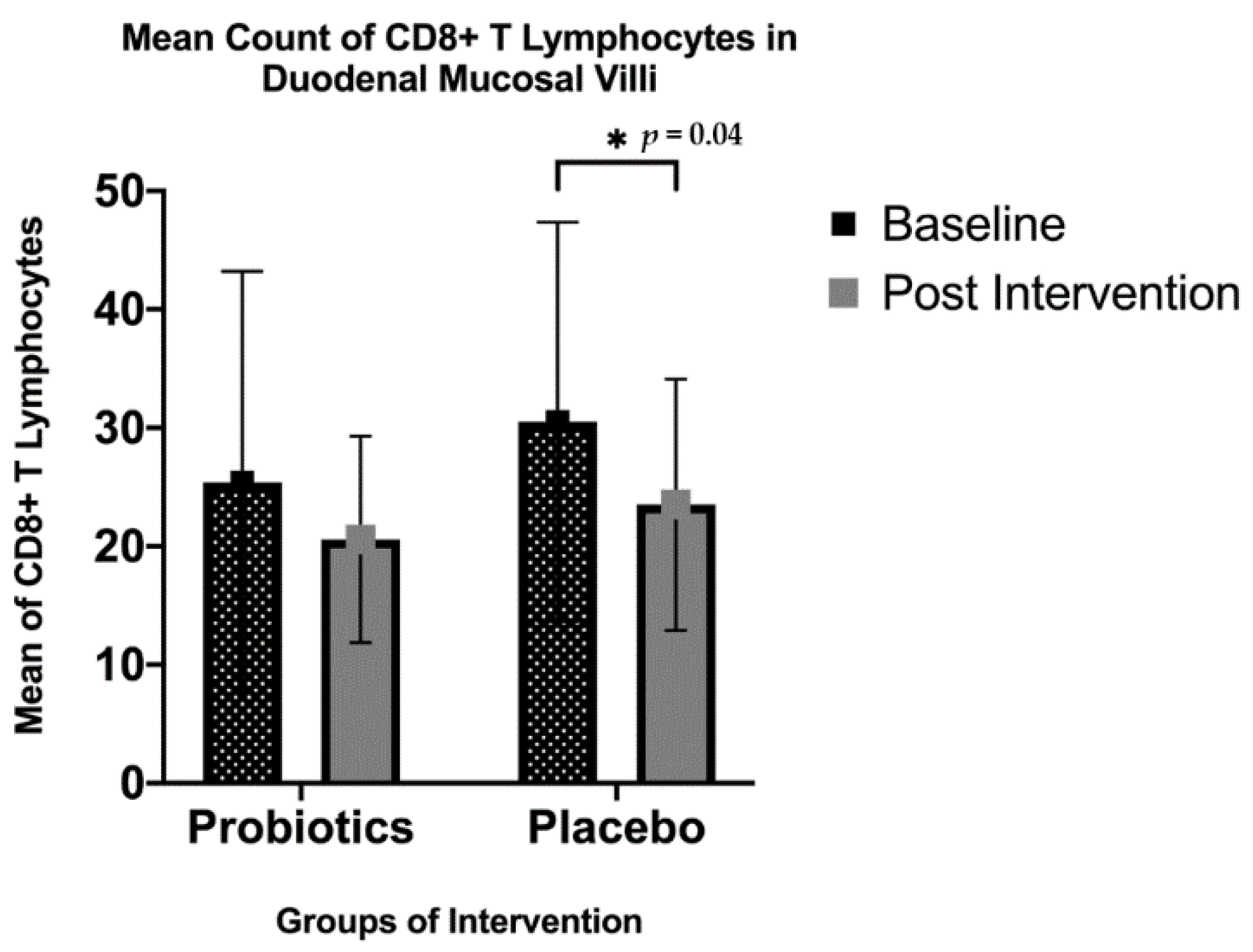
3.4. Immunohistochemistry Analysis
3.4.1. Expression of CD4+ T Lymphocytes
3.4.2. Expression of CD8+ T Lymphocytes
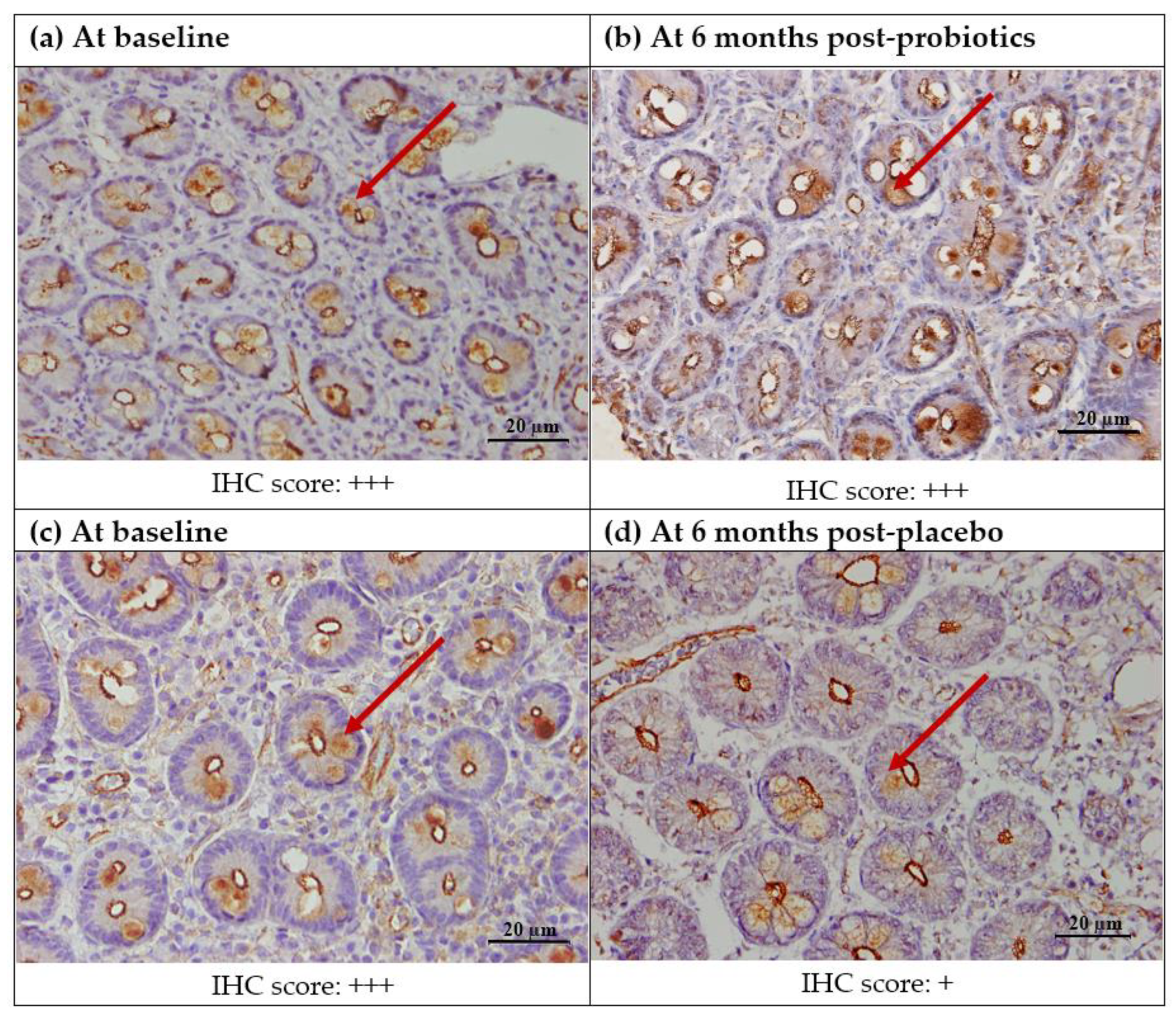
3.4.3. Expression of ZO-1
3.5. Nutritional Analysis
- (I)
- Fibrosis score: 0–0.27, no fibrosis, F0; 0.28–0.48, minimal, F1; 0.49–0.58, moderate, F2; 0.59–0.74, significant, F3; 0.75–1.00, severe, F4
- (II)
- Steatosis score: 0.69–1.0, no steatosis, S0; 0.38–0.56, minimal, S1; 0.57–0.68, moderate, S2; 0.69–1.00, severe, S3
- (III)
- Activity score: 0–0.29, no activity, A0; 0.3–0.52, minimal, A1; 0.53–0.62, moderate, A2; 0.63–0.72, significant, A3; 0.73–1.00, severe, A4
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Younossi, Z.M.; Koenig, A.B.; Abdelatif, D.; Fazel, Y.; Henry, L.; Wymer, M. Global epidemiology of nonalcoholic fatty liver disease—Meta-analytic assessment of prevalence, incidence, and outcomes. Hepatology 2016, 64, 73–84. [Google Scholar] [CrossRef] [Green Version]
- Li, J.; Zou, B.; Yeo, Y.H.; Feng, Y.; Xie, X.; Lee, D.H.; Fujii, H.; Wu, Y.; Kam, L.Y.; Ji, F.; et al. Prevalence, incidence, and outcome of non-alcoholic fatty liver disease in Asia, 1999–2019: A systematic review and meta-analysis. Lancet Gastroenterol. Hepatol. 2019, 4, 389–398. [Google Scholar] [CrossRef]
- Jennison, E.; Patel, J.; Scorletti, E.; Byrne, C.D. Diagnosis and management of non-alcoholic fatty liver disease. Postgrad. Med. J. 2019, 95, 314–322. [Google Scholar] [CrossRef] [PubMed]
- Buzzetti, E.; Pinzani, M.; Tsochatzis, E.A. The multiple-hit pathogenesis of non-alcoholic fatty liver disease (NAFLD). Metabolism 2016, 65, 1038–1048. [Google Scholar] [CrossRef] [PubMed]
- Bashiardes, S.; Shapiro, H.; Rozin, S.; Shibolet, O.; Elinav, E. Non-alcoholic fatty liver and the gut microbiota. Mol. Metab. 2016, 5, 782–794. [Google Scholar] [CrossRef] [PubMed]
- Jadhav, K.; Cohen, T.S. Can you trust your gut? Implicating a disrupted intestinal microbiome in the progression of NAFLD/NASH. Front. Endocrinol. 2020, 11, 592157. [Google Scholar] [CrossRef] [PubMed]
- MacIejewska, D.; Łukomska, A.; Dec, K.; Skonieczna-Zydecka, K.; Gutowska, I.; Skórka-Majewicz, M.; Styburski, D.; Misiakiewicz-Has, K.; Pilutin, A.; Palma, J. Diet-induced rat model of gradual development of non-alcoholic fatty liver dis-ease (NAFLD) with lipopolysaccharides (LPS) secretion. Diagnostics 2019, 9, 205. [Google Scholar] [CrossRef] [Green Version]
- Sander, M.E. Probiotics: Definition, sources, selection, and uses. Clin. Infect. Dis. 2008, 46, S58–S61. [Google Scholar] [CrossRef] [Green Version]
- Lim, C.C.; Ferguson, L.R.; Tannock, G.W. Dietary fibres as “prebiotics”: Implications for colorectal cancer. Mol. Nutr. Food Res. 2005, 49, 609–619. [Google Scholar] [CrossRef]
- Mofidi, F.; Poustchi, H.; Yari, Z.; Nourinayyer, B.; Merat, S.; Sharafkhah, M.; Malekzadeh, R.; Hekmatdoost, A. Synbiotic supplementation in lean patients with non-alcoholic fatty liver disease: A pilot, randomised, double-blind, placebo-controlled, clinical trial. Br. J. Nutr. 2017, 117, 662–668. [Google Scholar] [CrossRef] [Green Version]
- Loguercio, C.; De Simone, T.; Federico, A.; Terracciano, F.; Tuccillo, C.; Di Chicco, M.; Cartenì, M.; Del Vecchio Blanco, C. Gut-liver axis: A new point of attack to treat chronic liver damage? Am. J. Gastroenterol. 2002, 97, 2144–2146. [Google Scholar] [CrossRef] [PubMed]
- Li, Z.; Yang, S.; Lin, H.; Huang, J.; Watkins, P.A.; Moser, A.B.; DeSimone, C.; Song, X.Y.; Diehl, A.M. Probiotics and antibodies to TNF inhibit inflammatory activity and improve non-alcoholic fatty liver disease. Hepatology 2003, 37, 343–350. [Google Scholar] [CrossRef] [PubMed]
- Karaduta, O.; Glazko, G.; Dvanajscak, Z.; Arthur, J.; Mackintosh, S.; Orr, L.; Rahmatallah, Y.; Yeruva, L.; Tackett, A.; Zybailov, B. Resistant starch slows the progression of CKD in the 5/6 nephrectomy mouse model. Physiol. Rep. 2020, 8, e14610. [Google Scholar] [CrossRef] [PubMed]
- Jiang, T.; Wu, H.; Yang, X.; Li, Y.; Zhang, Z.; Chen, F.; Zhao, L.; Zhang, C. Lactobacillus mucosae strain promoted by a high-fiber diet in genetic obese child alleviates lipid metabolism and modifies gut microbiota in apoe-/- mice on a western diet. Microorganisms 2020, 8, 1225. [Google Scholar] [CrossRef]
- 15. Canani, R.B.; Sangwan, N.; Stefka, A.; Nocerino, R.; Paparo, L.; Aitoro, R.; Calignano, A.; Khan, A.A.; Gilbert, J.A.; Nagler, C.R. Lactobacillus rhamnosus GG-supplemented formula expands butyrate-producing bacterial strains in food allergic infants. ISME J. 2015, 10, 742–750. [Google Scholar] [CrossRef] [PubMed]
- Szajewska, H.; Kołodziej, M. Systematic review with meta-analysis: Lactobacillus rhamnosus GG in the prevention of antibiotic-associated diarrhea in children and adults. Aliment. Pharmacol. Ther. 2015, 42, 1149–1157. [Google Scholar] [CrossRef] [Green Version]
- Zaharuddin, L.; Mokhtar, N.M.; Nawawi, K.N.M.; Ali, R.A.R. A randomized double-blind placebo-controlled trial of probiotics in post-surgical colorectal cancer. BMC Gastroenterol. 2019, 19, 131. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ismail, I.S.; Bebakar, W.; Kamaruddin, N. Clinical Practice Guidelines on management of obesity 2004. Putrajaya: Ministry of Health Malaysia, Academy of Medicine of Malaysia, Malaysian Association for the Study of Obesity, Malaysian Endocrine and Metabolic Society. 2004. Available online: https://www.moh.gov.my/moh/resources/Penerbitan/CPG/Endocrine/5a.pdf (accessed on 5 September 2021).
- Nurul-fadhilah, A.; Teo, P.S.; Foo, L.H. Validity and reproducibility of a food frequency questionnaire (FFQ) for dietary as-sessment in Malay adolescents in Malaysia. Asia Pac. J. Clin. Nutr. 2012, 21, 97–103. [Google Scholar]
- Poynard, T.; Ratziu, V.; Naveau, S.; Thabut, D.; Charlotte, F.; Messous, D.; Capron, D.; Abella, A.; Massard, J.; Ngo, Y.; et al. The diagnostic value of biomarkers (SteatoTest) for the prediction of liver steatosis. Comp. Hepatol. 2005, 4, 10. [Google Scholar] [CrossRef] [Green Version]
- Munteanu, M.; Tiniakos, D.; Anstee, Q.; Charlotte, F.; Marchesini, G.; Bugianesi, E.; Trauner, M.; Romero, G.M.; Oliveira, C.; Day, C. Diagnostic performance of FibroTest, SteatoTest and ActiTest in patients with NAFLD using the SAF score as histological reference. Aliment. Pharmacol Ther. 2016, 44, 877–889. [Google Scholar] [CrossRef]
- Miele, L.; Valenza, V.; La Torre, G.; Montalto, M.; Cammarota, G.; Ricci, R.; Mascianà, R.; Forgione, A.; Gabrieli, M.L.; Perotti, G.; et al. Increased intestinal permeability and tight junction alterations in nonalcoholic fatty liver disease. Hepatology 2009, 49, 1877–1887. [Google Scholar] [CrossRef]
- Chan, W.-K.; Mustapha, N.R.N.; Mahadeva, S. Controlled attenuation parameter for the detection and quantification of hepatic steatosis in nonalcoholic fatty liver disease. J. Gastroenterol. Hepatol. 2014, 29, 1470–1476. [Google Scholar] [CrossRef]
- Krueger, K.P.; Felkey, B.G.; Berger, B.A. Improving adherence persistence: A review assessment of interventions description of steps toward a national adherence initiative. J. Am. Pharm. Assoc. 2003, 43, 668–679. [Google Scholar] [CrossRef]
- Michail, S.; Lin, M.; Frey, M.R.; Fanter, R.; Paliy, O.; Hilbush, B.; Reo, N.V. Altered gut microbial energy and metabolism in children with non-alcoholic fatty liver disease. FEMS Microbiol. Ecol. 2014, 91, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Zhu, L.; Baker, S.S.; Gill, C.; Liu, W.; Alkhouri, R.; Baker, R.D.; Gill, S.R. Characterization of gut microbiomes in nonalcoholic steatohepatitis (NASH) patients: A connection between endogenous alcohol and NASH. Hepatology 2012, 57, 601–609. [Google Scholar] [CrossRef] [PubMed]
- Mouzaki, M.; Comelli, E.M.; Arendt, B.M.; Bonengel, J.; Fung, S.K.; Fischer, S.; McGilvray, I.D.; Allard, J.P. Intestinal microbiota in patients with non-alcoholic fatty liver disease. Hepatology 2013, 58, 120–127. [Google Scholar] [CrossRef] [Green Version]
- Wong, V.W.-S.; Wong, G.L.-H.; Chan, H.L.-Y.; Yeung, D.K.W.; Chan, R.; Chim, A.M.-L.; Chan, C.K.M.; Tse, Y.K.; Woo, J.; Chu, W.C.W. Bacterial endotoxin and non-alcoholic fatty liver disease in the general population: A prospective cohort study. Aliment. Pharmacol. Ther. 2015, 42, 731–740. [Google Scholar] [CrossRef]
- Delzenne, N.M.; Knudsen, C.; Beaumont, M.; Rodriguez, J.; Neyrinck, A.; Bindels, L.B. Contribution of the gut microbiota to the regulation of host metabolism and energy balance: A focus on the gut–liver axis. Proc. Nutr. Soc. 2019, 78, 319–328. [Google Scholar] [CrossRef]
- Eslamparast, T.; Poustchi, H.; Zamani, F.; Sharafkhah, M.; Malekzadeh, R.; Hekmatdoost, A. Synbiotic supplementation in nonalcoholic fatty liver disease: A randomized, double-blind, placebo-controlled pilot study. Am. J. Clin. Nutr. 2014, 99, 535–542. [Google Scholar] [CrossRef] [PubMed]
- Ma, Y.Y.; Li, L.; Yu, C.H.; Shen, Z.; Chen, L.H.; Li, Y.M. Effects of probiotics on nonalcoholic fatty liver disease: A meta-analysis. World J. Gastroenterol. 2013, 19, 6911–6918. [Google Scholar] [CrossRef]
- Duseja, A.; Acharya, S.K.; Mehta, M.; Chhabra, S.; Rana, S.; Das, A.; Dattagupta, S.; Dhiman, R.K.; Chawla, Y.K. High potency multistrain probiotic improves liver histology in non-alcoholic fatty liver disease (NAFLD): A randomised, double-blind, proof of concept study. BMJ Open Gastroenterol. 2019, 6, e000315. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Scorletti, E.; Afolabi, P.R.; Miles, E.A.; Smith, D.E.; Almehmadi, A.; Alshathry, A.; Childs, C.E.; Del Fabbro, S.; Bilson, J.; Moyses, H.E. Synbiotics alter fecal microbiomes, but not liver fat or fibrosis, in a randomized trial of patients with non-alcoholic fatty liver disease. Gastroenterology 2020, 158, 1597–1610.e7. [Google Scholar] [CrossRef] [PubMed]
- Jiang, W.; Wu, N.; Wang, X.; Chi, Y.; Zhang, Y.; Qiu, X.; Hu, Y.; Li, J.; Liu, Y. Dysbiosis gut microbiota associated with in-flammation and impaired mucosal immune function in intestine of humans with non-alcoholic fatty liver disease. Sci. Rep. 2015, 5, 8096. [Google Scholar] [CrossRef] [PubMed]
- Zhao, C.; Lou, F.; Li, X.; Ma, J.; Zhu, Z.; Li, H.; Zhai, Y.; Chen, H.; Zhang, Q.; Liu, Z.; et al. Correlation of CD3+/CD4+, and serum CK-18 fragment levels with glucose and lipid metabolism in elderly type 2 diabetes patients with nonalcoholic fat-ty liver disease. Am. J. Transl. Res. 2021, 13, 2546–2554. [Google Scholar]
- Ma, C.; Kesarwala, A.; Eggert, T.; Medina-Echeverz, J.; Kleiner, D.E.; Jin, P.; Stroncek, P.J.D.F.; Terabe, M.; Kapoor, V.; Elgindi, M.; et al. NAFLD causes selective CD4+ T lymphocyte loss and promotes hepatocarcinogenesis. Nature 2016, 531, 253–257. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Antonucci, L.; Porcu, C.; Timperi, E.; Santini, S.J.; Iannucci, G.; Balsano, C. circulating neutrophils of nonalcoholic steatohepatitis patients show an activated phenotype and suppress T lymphocytes activity. J. Immunol. Res. 2020, 2020, 4570219. [Google Scholar] [CrossRef]
- Her, Z.; Tan, J.H.L.; Lim, Y.-S.; Tan, S.Y.; Chan, X.Y.; Tan, W.W.S.; Liu, M.; Yong, K.S.M.; Lai, F.; Ceccarello, E.; et al. CD4+ T cells mediate the development of liver fibrosis in high fat diet-induced NAFLD in humanized mice. Front. Immunol. 2020, 11, 580968. [Google Scholar] [CrossRef]
- Hu, Y.; Zhang, H.; Li, J.; Cong, X.; Chen, Y.; He, G.; Chi, Y.; Liu, Y. Gut-derived lymphocyte recruitment to liver and induce liver injury in non-alcoholic fatty liver disease mouse model. J. Gastroenterol. Hepatol. 2016, 31, 676–684. [Google Scholar] [CrossRef]
- Bauer, H.C.; Zweimueller-Mayer, J.; Steinbacher, P.; Lametschwandtner, A. The dual role of zonula occludens (ZO) proteins. J. Biomed. Biotechnol. 2010, 2010, 402593. [Google Scholar] [CrossRef] [Green Version]
- Feng, D.; Zou, J.; Su, D.; Mai, H.; Zhang, S.; Li, P.; Zheng, X. Curcumin prevents high-fat diet-induced hepatic steatosis in ApoE−/− mice by improving intestinal barrier function and reducing endotoxin and liver TLR4/NF-κB inflammation. Nutr. Metabol. 2019, 16, 79. [Google Scholar] [CrossRef]
- Kim, W.-K.; Jang, Y.J.; Seo, B.; Han, D.H.; Park, S.; Ko, G. Administration of Lactobacillus paracasei strains improves immunomodulation and changes the composition of gut microbiota leading to improvement of colitis in mice. J. Funct. Foods 2018, 52, 565–575. [Google Scholar] [CrossRef]
- Chong, C.W.; Ahmad, A.F.; Lim, Y.A.L.; Teh, C.S.J.; Yap, I.K.S.; Lee, S.C.; Chin, Y.T.; Loke, P.; Chua, K.H. Effect of ethnicity and socioeconomic variation to the gut microbiota composition among pre-adolescent in Malaysia. Sci. Rep. 2015, 5, srep13338. [Google Scholar] [CrossRef] [PubMed]
- Neoh, H.-M.; Osman, M.A.; Ab Mutalib, N.S.; Chin, S.F.; Ang, M.Y.; Mazlan, L.; Ngiu, C.S.; Jamal, R. IDDF2018-ABS-0199 Gut microbiome profiling of malaysians: A snapshot. BMJ 2018, 67, A13. [Google Scholar] [CrossRef]
- Lee, S.C.; Tang, M.S.; Lim, Y.A.L.; Choy, S.H.; Kurtz, Z.D.; Cox, L.M.; Gundra, U.M.; Cho, I.; Bonneau, R.; Blaser, M.J.; et al. Helminth colonization is associated with increased diversity of the gut microbiota. PLoS Negl. Trop. Dis. 2014, 8, e2880. [Google Scholar] [CrossRef] [PubMed]
- Bjerg, A.T.; Kristensen, M.; Ritz, C.; Holst, J.J.; Rasmussen, C.; Leser, T.D.; Wellejus, A.; Astrup, A. Lactobacillus paracasei subsp paracasei L. casei W8 suppresses energy intake acutely. Appetite 2014, 82, 111–118. [Google Scholar] [CrossRef]
- Nishida, C.; Martinez, N.F. FAO/WHO scientific update on carbohydrates in human nutrition: Introduction. Eur. J. Clin. Nutr. 2007, 61, S1–S4. [Google Scholar] [CrossRef]
- Ministry of Health Malaysia. Recommended Nutrient Intakes for Malaysia; Ministry of Health Malaysia: Putrajaya, Malaysia, 2005. [Google Scholar]
- Lee, Y.Y.; Muda, W.A.M.W. Dietary intakes and obesity of Malaysian adults. Nutr. Res. Pr. 2019, 13, 159–168. [Google Scholar] [CrossRef]
- Ismail, S.; Shamsuddin, K.; Latiff, K.; Saad, H. Food consumption among overweight and obese working Malay women in urban settings. Int. J. Community Med. Public Health 2016, 3, 658–662. [Google Scholar] [CrossRef] [Green Version]
- FAO. The State of Food and Agriculture Leveraging Food Systems for Inclusive Rural Transformation; FAO: Rome, Italy, 2017. [Google Scholar]

| Form | White Granules, Packed in a Sachet Form |
|---|---|
| Concentration | 30 billion colony-forming units (CFU) |
| Strains | MCP® BCMC® strains consisting of Lactobacillus acidophilus BCMC 12,130 (107 mg), Lactobacillus casei subsp. BCMC 12,313 (107 mg), Lactobacillus lactis BCMC 12,451 (107 mg), Bifidobacterium bifidum BCMC 02290 (107 mg), Bifidobacterium infantis BCMC 02129 (107 mg) and Bifidobacterium longum BCMC 02120 (107 mg) |
| Product weight | 3 g |
| Manufacturer | B-Crobes Laboratory Sdn. Bhd., GMP, manufactured in Malaysia |
| Total (n = 39) | Probiotics (n = 17) | Placebo (n = 22) | p-Value | |
|---|---|---|---|---|
| Age | 53.44 (14.13) | 54.70 (10.19) | 52.47 (16.73) | 0.63 |
| Gender | ||||
| Male | 28 | 11 | 17 | |
| Female | 11 | 6 | 5 | |
| Diabetes mellitus | ||||
| Yes | 19 | 9 | 10 | |
| No | 20 | 8 | 12 | |
| Hypertension | ||||
| Yes | 21 | 11 | 10 | |
| No | 18 | 6 | 12 | |
| Metabolic characteristics | ||||
| Height, m | 1.64 (0.08) | 1.62 (0.09) | 1.65 (0.07) | 0.21 |
| Weight, kg | 76.70 (13.45) | 75.00 (14.80) | 78.03 (12.51) | 0.49 |
| BMI, kg/m2 | 29.62 (8.46) | 31.33 (12.02) | 28.30 (3.90) | 0.63 |
| Nutritional intake | ||||
| Average kcal | 1731.82 (348.62) | 1759.94 (408.39) | 1710.09 (302.85) | 0.66 |
| Carbohydrate, g | 202.79(40.86) | 194.39 (46.82) | 209.29 (35.35) | 0.26 |
| % of total kcal | 46% | 44% | 48% | |
| Total fat, g | 67.23 (20.78) | 67.46 (21.81) | 61.31 (19.84) | 0.34 |
| % of total kcal | 33% | 34% | 32% | |
| Protein, g | 85.16 (23.93) | 91.64 (26.34) | 80.16 (21.16) | 0.14 |
| % of total kcal | 19% | 20% | 18% | |
| Serum biochemistry | ||||
| ALT, IU/L | 72.02 (34.77) | 70.29 (28.21) | 73.36 (39.71) | 0.78 |
| AST, IU/L | 46.92 (18.27) | 44.35 (12.67) | 48.90 (21.74) | 0.44 |
| GGT, IU/L | 70.10 (54.41) | 65.94 (34.07) | 73.31 (66.69) | 0.68 |
| Triglycerides, mmol/L | 2.06 (0.79) | 2.04 (0.79) | 2.09 (0.81) | 0.84 |
| Total Cholesterol, mmol/L | 5.79 (0.89) | 5.93(0.90) | 5.68 (0.88) | 0.38 |
| Fasting glucose, mmol/L | 5.34 (1.31) | 5.13 (0.96) | 5.50 (1.53) | 0.38 |
| Serum LiverFAST | ||||
| Steatosis score | 0.64 (0.15) | 0.67 (0.16) | 0.62 (0.14) | 0.41 |
| Fibrosis score | 0.30 (0.20) | 0.28 (0.17) | 0.33 (0.22) | 0.46 |
| Activity score | 0.42 (0.23) | 0.42 (0.21) | 0.43 (0.24) | 0.85 |
| Transient elastography | ||||
| Liver stiffness, kPa | 7.44 (2.76) | 7.25 (2.76) | 7.58 (2.82) | 0.37 |
| Controlled attenuated parameter, dB/m | 333.51 (34.35) | 339.11 (34.39) | 329.18 (35.15) | 0.71 |
| Probiotics (n = 17) | Placebo (n = 22) | |||||
|---|---|---|---|---|---|---|
| Baseline | End of Study | p-Value | Baseline | End of Study | p-Value | |
| Steatosis (CAP), dB/m | 339.17 (33.58) | 317.41 (40.37) | 0.05 | 329.18 (35.15) | 318.45 (45.37) | 0.29 |
| Liver stiffness, kPa | 7.25 (2.76) | 6.99 (2.74) | 0.55 | 7.58 (2.82) | 6.95 (2.19) | 0.23 |
| ALT, IU/L | 70.29 (28.21) | 84.29 (70.55) | 0.26 | 73.36 (39.71) | 74.50 (38.73) | 0.84 |
| AST, IU/L | 44.35(12.67) | 46.35 (23.19) | 0.64 | 48.90 (21.74) | 45.50 (25.80) | 0.36 |
| GGT, IU/L | 65.94 (34.07) | 72.17 (56.90) | 0.45 | 73.31 (66.69) | 74.63 (81.94) | 0.81 |
| * Steatosis score | 0.72 (0.53–0.80) | 0.76 (0.64–0.85) | 0.06 | 0.67 (0.52–0.74) | 0.73 (0.51–0.79) | 0.053 |
| * Fibrosis score | 0.26 (0.15–0.40) | 0.22 (0.18–0.36) | 0.88 | 0.27 (0.15–0.45) | 0.33 (0.15–0.36) | 0.022 |
| Activity score | 0.42 (0.21) | 0.41 (0.24) | 0.78 | 0.43 (0.24) | 0.44 (0.25) | 0.57 |
| * Body mass index, kg/m2 | 28.50 (25.0–31.60) | 30.0 (26.20–32.90) | 0.048 | 28.50 (25.05–31.15) | 29.60 (25.85–32.03) | 0.002 |
| Triglycerides, mg/dL | 2.04 (0.79) | 1.94 (0.75) | 0.55 | 2.09 (0.81) | 2.01 (1.01) | 0.66 |
| Total cholesterol, mg/dL | 5.93 (0.90) | 6.17 (1.38) | 0.31 | 5.68 (0.88) | 5.74 (1.46) | 0.79 |
| Fasting glucose, mg/dL | 5.13 (0.96) | 5.6 (1.09) | 0.06 | 5.50 (1.53) | 5.14(0.68) | 0.28 |
| Probiotics (n = 17) | Placebo (n = 22) | ||||
|---|---|---|---|---|---|
| Mean | SD | Mean | SD | p-Value | |
| Steatosis, dB/m | −21.7 | 42.60 | −10.72 | 46.64 | 0.45 |
| Liver stiffness, kPa | −0.25 | 1.77 | −0.62 | 2.37 | 0.59 |
| ALT, IU/L | 14.0 | 50.04 | 1.13 | 26.39 | 0.30 |
| AST, IU/L | 2.00 | 17.31 | −3.40 | 17.09 | 0.33 |
| GGT, IU/L | 6.2 | 33 | 1.35 | 28.38 | 0.60 |
| Steatosis score | 0.049 | 0.09 | 0.042 | 0.11 | 0.83 |
| Fibrosis score | 0.01 | 0.10 | 0.06 | 0.09 | 0.18 |
| Activity score | −0.12 | 0.15 | 0.015 | 0.13 | 0.56 |
| Body mass index, kg/m2 | 0.7 | 1.46 | 0.82 | 1.06 | 0.81 |
| Triglycerides, mg/dL | −0.10 | 0.68 | −0.07 | 0.77 | 0.90 |
| Total cholesterol, mg/dL | 0.23 | 0.93 | 0.05 | 1.07 | 0.59 |
| Fasting glucose, mg/dL | 0.46 | 0.94 | −0.44 | 1.31 | 0.03 |
| Probiotics (n = 17) | Placebo (n = 22) | |||||
|---|---|---|---|---|---|---|
| Baseline | End of Study | p-Value | Baseline | End of Study | p-Value | |
| Calories, kcal | 1759.94 (408) | 1645.03 (565) | 0.39 | 1636.04 (457) | 1637.11 (485) | 0.98 |
| Carbohydrates, g | 194.39 (46.82) | 215.31 (63.87) | 0.26 | 209.29 (35.35) | 213.24 (46.46) | 0.70 |
| Protein, g | 91.64(26.34) | 83.23 (23.77) | 0.14 | 80.16 (21.16) | 86.97 (21.75) | 0.13 |
| Total fat, g | 67.46 (21.81) | 56.82 (18.60) | <0.05 | 61.31 (19.84) | 58.77 (16.96) | 0.58 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mohamad Nor, M.H.; Ayob, N.; Mokhtar, N.M.; Raja Ali, R.A.; Tan, G.C.; Wong, Z.; Shafiee, N.H.; Wong, Y.P.; Mustangin, M.; Nawawi, K.N.M. The Effect of Probiotics (MCP® BCMC® Strains) on Hepatic Steatosis, Small Intestinal Mucosal Immune Function, and Intestinal Barrier in Patients with Non-Alcoholic Fatty Liver Disease. Nutrients 2021, 13, 3192. https://0-doi-org.brum.beds.ac.uk/10.3390/nu13093192
Mohamad Nor MH, Ayob N, Mokhtar NM, Raja Ali RA, Tan GC, Wong Z, Shafiee NH, Wong YP, Mustangin M, Nawawi KNM. The Effect of Probiotics (MCP® BCMC® Strains) on Hepatic Steatosis, Small Intestinal Mucosal Immune Function, and Intestinal Barrier in Patients with Non-Alcoholic Fatty Liver Disease. Nutrients. 2021; 13(9):3192. https://0-doi-org.brum.beds.ac.uk/10.3390/nu13093192
Chicago/Turabian StyleMohamad Nor, Mohamad Hizami, Nurainina Ayob, Norfilza M. Mokhtar, Raja Affendi Raja Ali, Geok Chin Tan, Zhiqin Wong, Nor Hamizah Shafiee, Yin Ping Wong, Muaatamarulain Mustangin, and Khairul Najmi Muhammad Nawawi. 2021. "The Effect of Probiotics (MCP® BCMC® Strains) on Hepatic Steatosis, Small Intestinal Mucosal Immune Function, and Intestinal Barrier in Patients with Non-Alcoholic Fatty Liver Disease" Nutrients 13, no. 9: 3192. https://0-doi-org.brum.beds.ac.uk/10.3390/nu13093192






