Antidepressant-Like Properties of Intrastriatal Botulinum Neurotoxin-A Injection in a Unilateral 6-OHDA Rat Model of Parkinson’s Disease
Abstract
:1. Introduction
2. Results
2.1. Spontaneous Motor Tests
2.1.1. Open Field Test
2.1.2. Elevated Plus Maze Test
2.1.3. Forced Swim Test
2.1.4. Tail Suspension Test
2.2. Correlating Open Field Test, Elevated Plus Maze Test, Forced Swim Test, and Apomorphine- and Amphetamine-Induced Rotations
3. Discussion
3.1. Readout of Test Results Indicating Anxiety-Like or Depression-Like Behavior
3.1.1. Anxiety
3.1.2. Anxiety-Like Behavior Is Not Induced in Hemi-PD Rats and Not Altered by Additional Intrastriatal BoNT-A
3.1.3. Depression
3.1.4. Depression-Like Behavior in Hemi-PD Rats Is Decreased by Intrastriatal BoNT-A
3.1.5. Tail Suspension Test
3.1.6. Correlating Parameters Indicative for Anxiety- and Depression-like Behaviors
3.1.7. Correlating Open Field Test, Elevated Plus Maze Test, Forced Swim Test and Apomorphine- and Amphetamine-Induced Rotations
4. Conclusions
5. Materials and Methods
5.1. Animals
5.2. Injections of Drugs
5.2.1. 6-OHDA Lesion Surgery
5.2.2. Injection of BoNT-A into the Striatum
5.3. Behavioral Testing
5.3.1. Drug-Induced Rotation Tests (Apomorphine, Amphetamine)
Apomorphine-Induced Rotation Test
Amphetamine-Induced Rotation Test
5.3.2. Spontaneous Motor Tests
Open Field Test
Elevated Plus Maze Test
Forced Swim Test
Tail Suspension Test
5.4. Data Analysis
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| α1 | noradrenergic α1 receptor |
| α2 | noradrenergic α2 receptor |
| ACC | anterior cingulate cortex |
| ACh | acetylcholine |
| BNST | bed nucleus of the stria terminalis |
| BoNT-A | botulinum neurotoxin-A |
| BSP | blepharospasm |
| CPu | caudate-putamen |
| DA | dopamine |
| D1 | dopamine D1 receptor |
| D2 | dopamine D2 receptor |
| D3 | dopamine D3 receptor |
| dmPFC | dorsomedial prefrontal cortex |
| EPM | elevated plus maze test |
| FST | forced swim test |
| 5-HT | serotonin |
| 5HT2A | serotonergic 5HT2A receptor |
| hemi-PD | hemiparkinsonian |
| HPC | hippocampus |
| iFC | intrinsic functional connectivity |
| mAch | muscarinic acetylcholine receptor |
| MAOI | monoamine-oxidase inhibitors |
| MAO-B | monoaminooxidase B |
| MDD | major depressive disorder |
| MFB | medial forebrain bundle |
| M1 | muscarinic M1 receptor |
| M2 | muscarinic M2 receptor |
| M3 | muscarinic M3 receptor |
| NA | noradrenaline |
| nAch | nicotinic acetylcholine receptor |
| OFT | open field test |
| 6-OHDA | 6-hydroxydopamine |
| PD | Parkinson’s disease |
| PET | positron emission tomography |
| PFC | prefrontal cortex |
| rs | Spearman’s correlation coefficient |
| SNpc | substantia nigra pars compacta |
| SNRI | norepinephrine reuptake inhibitors |
| SSRI | selective serotonin reuptake inhibitors |
| TCA | tricyclic antidepressants |
| TST | tail suspension test |
References
- Dorsey, E.R.; Constantinescu, R.; Thompson, J.P.; Biglan, K.M.; Holloway, R.G.; Kieburtz, K.; Marshall, F.J.; Ravina, B.M.; Schifitto, G.; Siderowf, A.; et al. Projected Number of People with Parkinson Disease in the Most Populous Nations, 2005 through 2030. Neurology 2007, 68, 384–386. [Google Scholar] [CrossRef] [PubMed]
- Kalia, L.V.; Lang, A.E. Parkinson’s Disease. Lancet 2015, 386, 896–912. [Google Scholar] [CrossRef]
- De Lau, L.M.; Breteler, M.M. Epidemiology of Parkinson’s Disease. Lancet Neurol. 2006, 5, 525–535. [Google Scholar] [CrossRef]
- Moustafa, A.A.; Chakravarthy, S.; Phillips, J.R.; Gupta, A.; Keri, S.; Polner, B.; Frank, M.J.; Jahanshahi, M. Motor Symptoms in Parkinson’s Disease: A Unified Framework. Neurosci. Biobehav. Rev. 2016, 68, 727–740. [Google Scholar] [CrossRef] [PubMed]
- Rafael, A.S.R.; Barbosa, J.M.P.; Rosas, M.J.S.L.; Garrett, M.C.L.A. Parkinson’s Disease and Development of Levodopa Induced Motor Complications: Influence of Baseline Features and First Medical Approach. Porto Biomed. J. 2016, 1, 136–141. [Google Scholar] [CrossRef] [Green Version]
- Boix, J.; Padel, T.; Paul, G. A Partial Lesion Model of Parkinson’s Disease in Mice—Characterization of a 6-OHDA-Induced Medial Forebrain Bundle Lesion. Behav. Brain Res. 2015, 284, 196–206. [Google Scholar] [CrossRef]
- Poirier, A.-A.; Aubé, B.; Côté, M.; Morin, N.; Di Paolo, T.; Soulet, D. Gastrointestinal Dysfunctions in Parkinson’s Disease: Symptoms and Treatments. Parkinsons. Dis. 2016, 2016, 6762528. [Google Scholar] [CrossRef]
- Jankovic, J.; Tolosa, E. Parkinson’s Disease and Movement Disorders, 6th ed.; Jankovic, J., Tolosa, E., Eds.; Lippincott Williams and Wilkins: Philadelphia, PA, USA, 2015; ISBN 9781608311767. [Google Scholar]
- Lees, A.J.; Hardy, J.; Revesz, T. Parkinson’s Disease. Lancet 2009, 373, 2055–2066. [Google Scholar] [CrossRef]
- Jankovic, J. Parkinson’s Disease: Clinical Features and Diagnosis. J. Neurol. Neurosurg. Psychiatry 2008, 79, 368–376. [Google Scholar] [CrossRef] [Green Version]
- Hayes, M.W.; Fung, V.S.; Kimber, T.E.; O’Sullivan, J.D. Current Concepts in the Management of Parkinson Disease. Med. J. Aust. 2010, 192, 144–149. [Google Scholar] [CrossRef]
- Rasmussen, M.; Li, Y.; Lindgreen, S.; Pedersen, J.S.; Albrechtsen, A.; Moltke, I.; Metspalu, M.; Metspalu, E.; Kivisild, T.; Gupta, R.; et al. Ancient Human Genome Sequence of an Extinct Palaeo-Eskimo. Nature 2010, 463, 757–762. [Google Scholar] [CrossRef] [PubMed]
- Chaudhuri, K.R.; Healy, D.G.; Schapira, A.H.H.V. Non-Motor Symptoms of Parkinson’s Disease: Diagnosis and Management. Lancet Neurol. 2006, 5, 235–245. [Google Scholar] [CrossRef]
- Langston, J.W. The Parkinson’s Complex: Parkinsonism Is Just the Tip of the Iceberg. Ann. Neurol. 2006, 59, 591–596. [Google Scholar] [CrossRef]
- Armstrong, M.J.; Okun, M.S. Diagnosis and Treatment of Parkinson Disease: A Review. JAMA J. Am. Med. Assoc. 2020, 323, 548–560. [Google Scholar] [CrossRef]
- Goldman, J.G.; Postuma, R. Premotor and Nonmotor Features of Parkinson’s Disease. Curr. Opin. Neurol. 2014, 27, 434–441. [Google Scholar] [CrossRef] [Green Version]
- Park, A.; Stacy, M. Non-Motor Symptoms in Parkinson’s Disease. J. Neurol. 2009, 256, 293–298. [Google Scholar] [CrossRef]
- Sauerbier, A.; Chaudhuri, K.R. Non-Motor Symptoms: The Core of Multi-Morbid Parkinson’s Disease. Br. J. Hosp. Med. 2014, 75, 18–24. [Google Scholar] [CrossRef]
- Schapira, A.H.V.V.; Emre, M.; Jenner, P.; Poewe, W. Levodopa in the Treatment of Parkinson’s Disease. Eur. J. Neurol. 2009, 16, 982–989. [Google Scholar] [CrossRef]
- Schapira, A.H.V.; Chaudhuri, K.R.; Jenner, P. Non-Motor Features of Parkinson Disease. Nat. Rev. Neurosci. 2017, 18, 435–450. [Google Scholar] [CrossRef]
- Schrag, A.; Jahanshahi, M.; Quinn, N. How Does Parkinson’s Disease Affect Quality of Life? A Comparison with Quality of Life in the General Population. Mov. Disord. 2000, 15, 1112–1118. [Google Scholar] [CrossRef]
- Martínez-Rivera, F.J.; Rodriguez-Romaguera, J.; Lloret-Torres, M.E.; Do Monte, F.H.; Quirk, G.J.; Barreto-Estrada, J.L. Bidirectional Modulation of Extinction of Drug Seeking by Deep Brain Stimulation of the Ventral Striatum. Biol. Psychiatry 2016, 80, 682–690. [Google Scholar] [CrossRef] [Green Version]
- Klingelhoefer, L.; Reichmann, H. Pathogenesis of Parkinson disease—The Gut-Brain Axis and Environmental Factors. Nat. Rev. Neurol. 2015, 11, 625–636. [Google Scholar] [CrossRef]
- Henderson, R.; Kurlan, R.; Kersun, J.M.; Como, P. Preliminary Examination of the Comorbidity of Anxiety and Depression in Parkinson’s Disease. J. Neuropsychiatry Clin. Neurosci. 1992, 4, 257–264. [Google Scholar] [CrossRef] [PubMed]
- Arnold, C.B. Major Depressive Disorder. Med. Sect. Proc. 1995, 358, 19–26. [Google Scholar] [CrossRef] [Green Version]
- Baquero, M.; Martín, N. Depressive Symptoms in Neurodegenerative Diseases. World J. Clin. Cases 2015, 3, 682. [Google Scholar] [CrossRef] [PubMed]
- Ferrari, A.J.; Charlson, F.J.; Norman, R.E.; Patten, S.B.; Freedman, G.; Murray, C.J.L.; Vos, T.; Whiteford, H.A. Burden of Depressive Disorders by Country, Sex, Age, and Year: Findings from the Global Burden of Disease Study 2010. PLoS Med. 2013, 10. [Google Scholar] [CrossRef] [Green Version]
- Aarsland, D.; Påhlhagen, S.; Ballard, C.G.; Ehrt, U.; Svenningsson, P. Depression in Parkinson Disease—Epidemiology, Mechanisms and Management. Nat. Rev. Neurol. 2012, 8, 35–47. [Google Scholar] [CrossRef]
- Steel, Z.; Marnane, C.; Iranpour, C.; Chey, T.; Jackson, J.W.; Patel, V.; Silove, D. The Global Prevalence of Common Mental Disorders: A Systematic Review and Meta-Analysis 1980–2013. Int. J. Epidemiol. 2014, 43, 476–493. [Google Scholar] [CrossRef] [Green Version]
- Rex, A.; Schickert, R.; Fink, H. Antidepressant-Like Effect of Nicotinamide Adenine Dinucleotide in the Forced Swim Test in Rats. Pharmacol. Biochem. Behav. 2004, 77, 303–307. [Google Scholar] [CrossRef] [PubMed]
- Ishihara, L.; Brayne, C. A Systematic Review of Depression and Mental Illness Preceding Parkinson’s Disease. Acta Neurol. Scand. 2006, 113, 211–220. [Google Scholar] [CrossRef]
- Fang, X.; Sugiyama, K.; Akamine, S.; Sun, W.; Namba, H. The Different Performance among Motor Tasks during the Increasing Current Intensity of Deep Brain Stimulation of the Subthalamic Nucleus in Rats with Different Degrees of the Unilateral Striatal Lesion. Neurosci. Lett. 2010, 480, 64–68. [Google Scholar] [CrossRef]
- Jacob, E.L.; Gatto, N.M.; Thompson, A.; Bordelon, Y.; Ritz, B. Occurrence of Depression and Anxiety Prior to Parkinson’s Disease. Park. Relat. Disord. 2010, 16, 576–581. [Google Scholar] [CrossRef] [Green Version]
- Alonso, A.; García Rodríguez, L.A.; Logroscino, G.; Hernán, M.A. Use of Antidepressants and the Risk of Parkinson’s Disease: A Prospective Study. J. Neurol. Neurosurg. Psychiatry 2009, 80, 671–674. [Google Scholar] [CrossRef] [Green Version]
- Leentjens, A.F.G.; Van den Akker, M.; Metsemakers, J.F.M.; Lousberg, R.; Verhey, F.R.J. Higher Incidence of Depression Preceding the Onset of Parkinson’s Disease: A Register Study. Mov. Disord. 2003, 18, 414–418. [Google Scholar] [CrossRef]
- Li, X.; Sundquist, J.; Hwang, H.; Sundquist, K. Impact of Psychiatric Disorders on Parkinson’s Disease: A Nationwide Follow-up Study from Sweden. J. Neurol. 2008, 255, 31–36. [Google Scholar] [CrossRef]
- Schuurman, A.G.; Van den Akker, M.; Ensinck, K.T.J.L.; Metsemakers, J.F.M.; Knottnerus, J.A.; Leentjens, A.F.G.; Buntinx, F. Increased Risk of Parkinson’s Disease after Depression: A Retrospective Cohort Study. Neurology 2002, 58, 1501–1504. [Google Scholar] [CrossRef]
- Shen, C.C.; Tsai, S.J.; Perng, C.L.; Kuo, B.I.T.; Yang, A.C. Risk of Parkinson Disease after Depression: A Nationwide Population-Based Study. Neurology 2013, 81, 1538–1544. [Google Scholar] [CrossRef] [PubMed]
- Poewe, W. Non-Motor Symptoms in Parkinson’s Disease. Eur. J. Neurol. 2008, 15 (Suppl. S1), 14–20. [Google Scholar] [CrossRef]
- Riis, R.C.; Cummings, J.F.; Loew, E.R.; De Lahunta, A. Tibetan Terrier Model of Canine Ceroid Lipofuscinosis. Am. J. Med. Genet. 1992, 42, 615–621. [Google Scholar] [CrossRef]
- Slaughter, J.R.; Slaughter, K.A.; Nichols, D.; Holmes, S.E.; Martens, M.P. Prevalence, Clinical Manifestations, Etiology, and Treatment of Depression in Parkinson’s Disease. J. Neuropsychiatry Clin. Neurosci. 2001, 13, 187–196. [Google Scholar] [CrossRef]
- Allain, H.; Schuck, S.; Mauduit, N. Depression in Parkinson’s Disease. Br. Med. J. 2000, 320, 1287–1288. [Google Scholar] [CrossRef]
- Blonder, L.X.; Slevin, J.T. Emotional Dysfunction in Parkinson’s Disease. Behav. Neurol. 2011, 24, 201–217. [Google Scholar] [CrossRef]
- Veazey, C.; Aki, S.O.E.; Cook, K.F.; Lai, E.C.; Kunik, M.E. Prevalence and Treatment of Depression in Parkinson’s Disease. J. Neuropsychiatry Clin. Neurosci. 2005, 17, 310–323. [Google Scholar] [CrossRef]
- Hantz, P.; Caradoc-Davies, G.; Caradoc-Davies, T.; Weatherall, M.; Dixon, G. Depression in Parkinson’s Disease. Am. J. Psychiatry 1994, 151, 1010–1014. [Google Scholar] [CrossRef] [Green Version]
- Mayeux, R.; Stern, Y.; Rosen, J.; Leventhal, J. Depression, Intellectual Impairment, and Parkinson Disease. Neurology 1981, 31, 645–650. [Google Scholar] [CrossRef]
- Taylor, A.E.; Saint-Cyr, J.A.; Lang, A.E.; Kenny, F.T. Parkinson’s Disease and Depression: A Critical Re-Evaluation. Brain 1986, 109, 279–292. [Google Scholar] [CrossRef]
- Tandberg, E.; Larsen, J.P.; Aarsland, D.; Cummings, J.L. The Occurrence of Depression in Parkinson’s Disease: A Community-Based Study. Arch. Neurol. 1996, 53, 175–179. [Google Scholar] [CrossRef]
- Starkstein, S.E.; Merello, M.; Jorge, R.; Brockman, S.; Bruce, D.; Petracca, G.; Robinson, R.G. A Validation Study of Depressive Syndromes in Parkinson’s Disease. Mov. Disord. 2008, 23, 538–546. [Google Scholar] [CrossRef]
- Gotham, A.M.; Brown, R.G.; Marsden, C.D. Depression in Parkinson’s Disease: A Quantitative and Qualitative Analysis. J. Neurol. Neurosurg. Psychiatry 1986, 49, 381–389. [Google Scholar] [CrossRef] [Green Version]
- Dobkin, R.D.F.; Menza, M.; Bienfait, K.L.; Gara, M.; Marin, H.; Mark, M.H.; Dicke, A.; Tröster, A. The Impact of Antidepressant Treatment on Cognitive Functioning in Depressed Patients with Parkinson’s Disease. J. Neuropsychiatry Clin. Neurosci. 2010, 22, 188–195. [Google Scholar] [CrossRef] [PubMed]
- Cummings, J.L. Depression and Parkinson’s Disease: A Review. Am. J. Psychiatry 1992, 149, 443–454. [Google Scholar] [CrossRef]
- Poewe, W.H.; Rascol, O.; Quinn, N.; Tolosa, E.; Oertel, W.H.; Martignoni, E.; Rupp, M.; Boroojerdi, B. Efficacy of Pramipexole and Transdermal Rotigotine in Advanced Parkinson’s Disease: A Double-Blind, Double-Dummy, Randomised Controlled Trial. Lancet Neurol. 2007, 6, 513–520. [Google Scholar] [CrossRef]
- Majbour, N.; El-Agnaf, O. Cognitive Impairment in Parkinson’s Disease. Lancet Neurol. 2017, 16, 23. [Google Scholar] [CrossRef]
- Starkstein, S.E.; Preziosi, T.J.; Forrester, A.W.; Robinson, R.G. Specificity of Affective and Autonomic Symptoms of Depression in Parkinson’s Disease. J. Neurol. Neurosurg. Psychiatry 1990, 53, 869–873. [Google Scholar] [CrossRef]
- Starkstein, S.E.; Mayberg, H.S.; Preziosi, T.J.; Andrezejewski, P.; Leiguarda, R.; Robinson, R.G. Reliability, Validity, and Clinical Correlates of Apathy in Parkinson’s Disease. J. Neuropsychiatry Clin. Neurosci. 1992, 4, 134–139. [Google Scholar] [CrossRef]
- McDonald, W.M.; Richard, I.H.; DeLong, M.R. Prevalence, Etiology, and Treatment of Depression in Parkinson’s Disease. Biol. Psychiatry 2003, 54, 363–375. [Google Scholar] [CrossRef]
- Mayeux, R. Depression in the Patient with Parkinson’s Disease. J. Clin. Psychiatry 1990, 51, 20–23. [Google Scholar]
- Mayeux, R.; Williams, J.B.; Stern, Y.; Côté, L. Depression and Parkinson’s Disease. Adv. Neurol. 1984, 40, 241–250. [Google Scholar] [PubMed]
- Santiago, R.M.; Barbieiro, J.; Lima, M.M.S.; Dombrowski, P.A.; Andreatini, R.; Vital, M.A.B.F. Depressive-Like Behaviors Alterations Induced by Intranigral MPTP, 6-OHDA, LPS and Rotenone Models of Parkinson’s Disease Are Predominantly Associated with Serotonin and Dopamine. Prog. Neuro-Psychopharmacol. Biol. Psychiatry 2010, 34, 1104–1114. [Google Scholar] [CrossRef] [PubMed]
- Chaudhuri, K.R.; Schapira, A.H.V. Non-Motor Symptoms of Parkinson’s Disease: Dopaminergic Pathophysiology and Treatment. Lancet. Neurol. 2009, 8, 464–474. [Google Scholar] [CrossRef]
- Lewis, S.J.G.; Dove, A.; Robbins, T.W.; Barker, R.A.; Owen, A.M. Cognitive Impairments in Early Parkinson’s Disease Are Accompanied by Reductions in Activity in Frontostriatal Neural Circuitry. J. Neurosci. 2003, 23, 6351–6356. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hely, M.A.; Reid, W.G.J.; Adena, M.A.; Halliday, G.M.; Morris, J.G.L. The Sydney Multicenter Study of Parkinson’s Disease: The Inevitability of Dementia at 20 years. Mov. Disord. 2008, 23, 837–844. [Google Scholar] [CrossRef]
- Adler, C.H.; Caviness, J.N.; Sabbagh, M.N.; Shill, H.A.; Connor, D.J.; Sue, L.; Evidente, V.G.H.; Driver-Dunckley, E.; Beach, T.G. Heterogeneous Neuropathological Findings in Parkinson’s Disease with Mild Cognitive Impairment. Acta Neuropathol. 2010, 120, 827–828. [Google Scholar] [CrossRef] [Green Version]
- Fahn, S. Does Levodopa Slow or Hasten the Rate of Progression of Parkinson’s Disease? J. Neurol. 2005, 252. [Google Scholar] [CrossRef]
- Stoker, T.B.; Barker, R.A. Recent Developments in the Treatment of Parkinson’s Disease. F1000Research 2020, 9. [Google Scholar] [CrossRef]
- Xie, C.; Prasad, A.A. Probiotics Treatment Improves Hippocampal Dependent Cognition in a Rodent Model of Parkinson’s Disease. Microorganisms 2020, 8, 1661. [Google Scholar] [CrossRef]
- Hälbig, T.D.; Assuras, S.; Creighton, J.; Borod, J.C.; Tse, W.; Frisina, P.G.; Voustianiouk, A.; Gracies, J.M.; Olanow, C.W. Differential Role of Dopamine In Emotional Attention and Memory: Evidence from Parkinson’s Disease. Mov. Disord. 2011, 26, 1677–1683. [Google Scholar] [CrossRef]
- Blonder, L.X.; Slevin, J.T.; Kryscio, R.J.; Martin, C.A.; Andersen, A.H.; Smith, C.D.; Schmitt, F.A. Dopaminergic Modulation of Memory and Affective Processing in Parkinson Depression. Psychiatry Res. 2013, 210, 146–149. [Google Scholar] [CrossRef] [Green Version]
- Herrero, M.T.; Pagonabarraga, J.; Linazasoro, G. Neuroprotective Role of Dopamine Agonists: Evidence from Animal Models and Clinical Studies. Neurologist 2011, 17. [Google Scholar] [CrossRef]
- Müller, T.; Baas, H.; Kassubek, J.; Riederer, P.; Urban, P.P.; Schrader, C.; Reichmann, H.; Woitalla, D.; Gerlach, M. Laboratory Assessments in the Course of Parkinson’s Disease: A Clinician’s Perspective. J. Neural Transm. 2016, 123, 65–71. [Google Scholar] [CrossRef]
- Muzerengi, S.; Contrafatto, D.; Chaudhuri, K.R. Non-Motor Symptoms: Identification and Management. Park. Relat. Disord. 2007, 13. [Google Scholar] [CrossRef]
- McDowell, K.; Chesselet, M.F. Animal Models of the Non-Motor Features of Parkinson’s Disease. Neurobiol. Dis. 2012, 46, 597–606. [Google Scholar] [CrossRef] [Green Version]
- Zhang, X.; Egeland, M.; Svenningsson, P. Antidepressant-Like Properties of Sarizotan in Experimental Parkinsonism. Psychopharmacology 2011, 218, 621–634. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rihmer, Z. Antidepresszívumok, Depresszió és Öngyilkosság. Neuropsychopharmacol. Hung. 2013, 15, 157–164. [Google Scholar] [PubMed]
- Chen, P.; Kales, H.C.; Weintraub, D.; Blow, F.C.; Jiang, L.; Mellow, A.M. Antidepressant Treatment of Veterans with Parkinson’s Disease and Depression: Analysis of a National Sample. J. Geriatr. Psychiatry Neurol. 2007, 20, 161–165. [Google Scholar] [CrossRef] [PubMed]
- Cools, R.; Stefanova, E.; Barker, R.A.; Robbins, T.W.; Owen, A.M. Dopaminergic Modulation of High-Level Cognition in Parkinson’s Disease: The Role of the Prefrontal Cortex Revealed by PET. Brain 2002, 125, 584–594. [Google Scholar] [CrossRef] [Green Version]
- Mattay, V.S.; Tessitore, A.; Callicott, J.H.; Bertolino, A.; Goldberg, T.E.; Chase, T.N.; Hyde, T.M.; Weinberger, D.R. Dopaminergic Modulation of Cortical Function in Patients with Parkinson’s Disease. Ann. Neurol. 2002, 51, 156–164. [Google Scholar] [CrossRef]
- Tessitore, A.; Hariri, A.R.; Fera, F.; Smith, W.G.; Chase, T.N.; Hyde, T.M.; Weinberger, D.R.; Mattay, V.S. Dopamine Modulates the Response of the Human Amygdala: A Study in Parkinson’s Disease. J. Neurosci. 2002, 22, 9099–9103. [Google Scholar] [CrossRef] [Green Version]
- Cools, R.; Barker, R.A.; Sahakian, B.J.; Robbins, T.W. L-Dopa Medication Remediates Cognitive Inflexibility, but Increases Impulsivity in Patients with Parkinson’s Disease. Neuropsychologia 2003, 41, 1431–1441. [Google Scholar] [CrossRef]
- Cools, R.; Barker, R.A.; Sahakian, B.J.; Robbins, T.W. Enhanced or Impaired Cognitive Function in Parkinson’s Disease as a Function of Dopaminergic Medication and Task Demands. Cereb. Cortex 2001, 11, 1136–1143. [Google Scholar] [CrossRef]
- Benton, J.L.; Wengel, S.P.; Burke, W.J. Depression in Parkinson’s Disease: An Update. In Parkinson’s Disease and Nonmotor Dysfunction, 2nd ed.; Humana Press Inc.: Totowa, NJ, USA, 2013; pp. 3–15. ISBN 9781607614296. [Google Scholar]
- Robertson, M.M.; Katona, C.L.E. Depression in Neurological Disorders. In Depression and Physical Illness; Robertson, M.M., Katona, C.L., Eds.; John Wiley: Chichester, UK; New York, NY, USA, 1997; pp. 305–340. ISBN 0471961485. [Google Scholar]
- Latoo, J.; Mistry, M.; Dunne, F.J. Depression in Parkinson’s Disease: Diagnosis and Management. Br. J. Hosp. Med. 2012, 73, 331–334. [Google Scholar] [CrossRef]
- Schwarz, J.; Odin, P.; Buhmann, C.; Csoti, I.; Jost, W.; Wüllner, U.; Storch, A. Depression in Parkinson’s Disease. J. Neurol. 2011, 258, S336–S338. [Google Scholar] [CrossRef]
- Eskow Jaunarajs, K.L.; Angoa-Perez, M.; Kuhn, D.M.; Bishop, C. Potential Mechanisms Underlying Anxiety and Depression in Parkinson’s Disease: Consequences of L-DOPA Treatment. Neurosci. Biobehav. Rev. 2011, 35, 556–564. [Google Scholar] [CrossRef] [Green Version]
- Imamura, K.; Okayasu, N.; Nagatsu, T. The Relationship between Depression and Regional Cerebral Blood Flow in Parkinson’s Disease and the Effect of Selegiline Treatment. Acta Neurol. Scand. 2011, 124, 28–39. [Google Scholar] [CrossRef]
- Korchounov, A.; Winter, Y.; Rössy, W. Combined Beneficial Effect of Rasagiline on Motor Function and Depression in De Novo PD. Clin. Neuropharmacol. 2012, 35, 121–124. [Google Scholar] [CrossRef] [PubMed]
- Bxarone, P.; Poewe, W.; Albrecht, S.; Debieuvre, C.; Massey, D.; Rascol, O.; Tolosa, E.; Weintraub, D. Pramipexole for the Treatment of Depressive Symptoms in Patients with Parkinson’s Disease: A Randomised, Double-Blind, Placebo-Controlled Trial. Lancet Neurol. 2010, 9, 573–580. [Google Scholar] [CrossRef]
- Starkstein, S.E.; Brockman, S.; Hayhow, B.D. Psychiatric Syndromes in Parkinson’s Disease. Curr. Opin. Psychiatry 2012, 25, 468–472. [Google Scholar] [CrossRef]
- Schreiber, M.A.; Thompson, W.A. The Pharmacologic Management of Depression in Parkinson’s Disease. Degener. Neurol. Neuromuscul. Dis. 2013, 3, 1. [Google Scholar] [CrossRef] [Green Version]
- Costa, F.H.R.; Rosso, A.L.Z.; Maultasch, H.; Nicaretta, D.H.; Vincent, M.B. Depression in Parkinson’s Disease: Diagnosis and Treatment. Arq. Neuropsiquiatr. 2012, 70, 617–620. [Google Scholar] [CrossRef]
- Hanna, K.K.; Cronin-Golomb, A. Impact of Anxiety on Quality of Life in Parkinson’s Disease. Parkinsons. Dis. 2012, 2012. [Google Scholar] [CrossRef] [Green Version]
- Riedel, O.; Dodel, R.; Deuschl, G.; Klotsche, J.; Förstl, H.; Heuser, I.; Oertel, W.; Reichmann, H.; Riederer, P.; Trenkwalder, C.; et al. Depression and Care-Dependency in Parkinson’s Disease: Results from a Nationwide Study of 1449 Outpatients. Park. Relat. Disord. 2012, 18, 598–601. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Pontone, G.M.; Williams, J.R.; Anderson, K.E.; Chase, G.; Goldstein, S.R.; Grill, S.; Hirsch, E.S.; Lehmann, S.; Little, J.T.; Margolis, R.L.; et al. Anxiety and Self-Perceived Health Status in Parkinson’s Disease. Park. Relat. Disord. 2011, 17, 249–254. [Google Scholar] [CrossRef] [Green Version]
- Weintraub, D.; Moberg, P.J.; Duda, J.E.; Katz, I.R.; Stern, M.B. Effect of Psychiatric and Other Nonmotor Symptoms on Disability in Parkinson’s Disease. J. Am. Geriatr. Soc. 2004, 52, 784–788. [Google Scholar] [CrossRef]
- Mathias, J.L. Neurobehavioral Functioning of Persons with Parkinson’s Disease. Appl. Neuropsychol. 2003, 10, 57–68. [Google Scholar] [CrossRef]
- Richard, I.H.; Schiffer, R.B.; Kurlan, R. Anxiety and Parkinson’s Disease. J. Neuropsychiatry Clin. Neurosci. 1996, 8, 383–392. [Google Scholar] [CrossRef] [Green Version]
- Martínez-Martín, P.; Damián, J. Parkinson Disease: Depression and Anxiety in Parkinson Disease. Nat. Rev. Neurol. 2010, 6, 243–245. [Google Scholar] [CrossRef] [PubMed]
- Walsh, K.; Bennett, G. Parkinson’s Disease and Anxiety. Postgrad. Med. J. 2001, 77, 89–93. [Google Scholar] [CrossRef] [Green Version]
- Chen, J.J.; Marsh, L. Anxiety in Parkinson’s Disease: Identification and Management. Ther. Adv. Neurol. Disord. 2014, 7, 52–59. [Google Scholar] [CrossRef] [Green Version]
- Schiffer, R.B.; Kurlan, R.; Rubin, A.; Boer, S. Evidence for Atypical Depression in Parkinson’s Disease. Am. J. Psychiatry 1988, 145, 1020–1022. [Google Scholar] [CrossRef]
- Menza, M.A.; Robertson-Hoffman, D.E.; Bonapace, A.S. Parkinson’s Disease and Anxiety: Comorbidity with Depression. Biol. Psychiatry 1993, 34, 465–470. [Google Scholar] [CrossRef]
- Menza, M.A.; Mark, M.H. Parkinson’s Disease and Depression: The Relationship to Disability and Personality. J. Neuropsychiatry Clin. Neurosci. 1994, 6, 165–169. [Google Scholar] [CrossRef]
- Ding, J.; Guzman, J.N.; Tkatch, T.; Chen, S.; Goldberg, J.A.; Ebert, P.J.; Levitt, P.; Wilson, C.J.; Hamm, H.E.; Surmeier, D.J. RGS4-Dependent Attenuation of M4 Autoreceptor Function in Striatal Cholinergic Interneurons Following Dopamine Depletion. Nat. Neurosci. 2006, 9, 832–842. [Google Scholar] [CrossRef]
- Oldenburg, I.A.; Ding, J.B. Cholinergic Modulation of Synaptic Integration and Dendritic Excitability in the Striatum. Curr. Opin. Neurobiol. 2011, 21, 425–432. [Google Scholar] [CrossRef] [Green Version]
- Pisani, A.; Bernardi, G.; Ding, J.; Surmeier, D.J. Re-Emergence of Striatal Cholinergic Interneurons in Movement Disorders. Trends Neurosci. 2007, 30, 545–553. [Google Scholar] [CrossRef]
- Ztaou, S.; Maurice, N.; Camon, J.; Guiraudie-Capraz, G.; Kerkerian-Le Goff, L.; Beurrier, C.; Liberge, M.; Amalric, M. Involvement of Striatal Cholinergic Interneurons and M1 and M4 Muscarinic Receptors in Motor Symptoms of Parkinson’s Disease. J. Neurosci. 2016, 36, 9161–9172. [Google Scholar] [CrossRef] [PubMed]
- Antipova, V.; Hawlitschka, A.; Mix, E.; Schmitt, O.; Dräger, D.; Benecke, R.; Wree, A. Behavioral and Structural Effects of Unilateral Intrastriatal Injections of Botulinum Neurotoxin A in the Rat Model of Parkinson’s Disease. J. Neurosci. Res. 2013, 91, 838–847. [Google Scholar] [CrossRef]
- Antipova, V.; Holzmann, C.; Schmitt, O.; Wree, A.; Hawlitschka, A. Botulinum Neurotoxin A Injected Ipsilaterally or Contralaterally into the Striatum in the Rat 6-OHDA Model of Unilateral Parkinson’s Disease Differently Affects Behavior. Front. Behav. Neurosci. 2017, 11, 119. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Antipova, V.; Wree, A.; Holzmann, C.; Mann, T.; Palomero-Gallagher, N.; Zilles, K.; Schmitt, O.; Hawlitschka, A. Unilateral Botulinum Neurotoxin-A Injection into the Striatum of C57BL/6 Mice Leads to a Different Motor Behavior Compared with Rats. Toxins 2018, 10, 295. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Antipova, V.; Holzmann, C.; Hawlitschka, A.; Wree, A. Botulinum Neurotoxin-A Injected Intrastriatally into Hemiparkinsonian Rats Improves the Initiation Time for Left and Right Forelimbs in Both Forehand and Backhand Directions. Int. J. Mol. Sci. 2019, 20, 992. [Google Scholar] [CrossRef] [Green Version]
- Hawlitschka, A.; Antipova, V.; Schmitt, O.; Witt, M.; Benecke, R.; Mix, E.; Wree, A. Intracerebrally Applied Botulinum Neurotoxin in Experimental Neuroscience. Curr. Pharm. Biotechnol. 2013, 14, 124–130. [Google Scholar] [CrossRef]
- Hawlitschka, A.; Holzmann, C.; Wree, A.; Antipova, V. Repeated Intrastriatal Botulinum Neurotoxin-A Injection in Hemiparkinsonian Rats Increased the Beneficial Effect on Rotational Behavior. Toxins 2018, 10, 368. [Google Scholar] [CrossRef] [Green Version]
- Hawlitschka, A.; Berg, C.; Schmitt, O.; Holzmann, C.; Wree, A.; Antipova, V. Repeated Intrastriatal Application of Botulinum Neurotoxin-A Did Not Influence Choline Acetyltransferase-Immunoreactive Interneurons in Hemiparkinsonian Rat Brain—A Histological, Stereological and Correlational Analysis. Brain Res. 2020, 1742, 146877. [Google Scholar] [CrossRef] [PubMed]
- Hawlitschka, A.; Wree, A. Experimental Intrastriatal Applications of Botulinum Neurotoxin-A: A Review. Int. J. Mol. Sci. 2018, 19, 1392. [Google Scholar] [CrossRef] [Green Version]
- Holzmann, C.; Dräger, D.; Mix, E.; Hawlitschka, A.; Antipova, V.; Benecke, R.; Wree, A. Effects of Intrastriatal Botulinum Neurotoxin A on the Behavior of Wistar Rats. Behav. Brain Res. 2012, 234, 107–116. [Google Scholar] [CrossRef] [PubMed]
- Wree, A.; Mix, E.; Hawlitschka, A.; Antipova, V.; Witt, M.; Schmitt, O.; Benecke, R. Intrastriatal Botulinum Toxin Abolishes Pathologic Rotational Behaviour and Induces Axonal Varicosities in the 6-OHDA Rat Model of Parkinson’s Disease. Neurobiol. Dis. 2011, 41, 291–298. [Google Scholar] [CrossRef]
- Mehlan, J.; Brosig, H.; Schmitt, O.; Mix, E.; Wree, A.; Hawlitschka, A. Intrastriatal Injection of Botulinum Neurotoxin-A Is Not Cytotoxic in Rat Brain—A Histological and Stereological Analysis. Brain Res. 2016, 1630, 18–24. [Google Scholar] [CrossRef]
- Wree, A.; Hawlitschka, A.; Holzmann, C.; Witt, M.; Kurth, J.; Lindner, T.; Mann, T.; Antipova, V. Interlinking Potential Therapy with Botulinum Neurotoxin A and Parkinson’s Disease. In The Neuroscience of Parkinson’s Disease; Martin, C.R., Preedy, V.R., Eds.; Elsevier/Academic Press: London, UK, 2020; pp. 665–681. ISBN 9780128159583. [Google Scholar]
- Dagyte, G.; Den Boer, J.A.; Trentani, A. The Cholinergic System and Depression. Behav. Brain Res. 2011, 221, 574–582. [Google Scholar] [CrossRef]
- Reuter, M.; Markett, S.; Melchers, M.; Montag, C. Interaction of the Cholinergic System and the Hypothalamic-Pituitary-Adrenal Axis as a Risk Factor for Depression: Evidence from a Genetic Association Study. Neuroreport 2012, 23, 717–720. [Google Scholar] [CrossRef] [PubMed]
- Dilsaver, S.C. Cholinergic Mechanisms in Depression. Brain Res. Rev. 1986, 11, 285–316. [Google Scholar] [CrossRef] [Green Version]
- Dulawa, S.C.; Janowsky, D.S. Cholinergic Regulation of Mood: From Basic and Clinical Studies to Emerging Therapeutics. Mol. Psychiatry 2019, 24, 694–709. [Google Scholar] [CrossRef]
- Janowsky, D.S.; Davis, J.M.; El-Yousef, M.K.; Sekerke, H.J. A Cholinergic-Adrenergic Hypothesis of Mania and Depression. Lancet 1972, 300, 632–635. [Google Scholar] [CrossRef]
- Barbosa, I.G.; Vaz, G.N.; Rocha, N.P.; Machado-Vieira, R.; Ventura, M.R.D.; Huguet, R.B.; Bauer, M.E.; Berk, M.; Teixeira, A.L. Plasma Levels of Tumor Necrosis Factor Superfamily Molecules Are Increased in Bipolar Disorder. Clin. Psychopharmacol. Neurosci. 2017, 15, 269–275. [Google Scholar] [CrossRef] [Green Version]
- Suarez-Lopez, J.R.; Hood, N.; Suárez-Torres, J.; Gahagan, S.; Gunnar, M.R.; López-Paredes, D. Associations of Acetylcholinesterase Activity with Depression and Anxiety Symptoms among Adolescents Growing Up Near Pesticide Spray Sites. Int. J. Hyg. Environ. Health 2019, 222, 981–990. [Google Scholar] [CrossRef]
- Eppolito, A.K.; Bachus, S.E.; McDonald, C.G.; Meador-Woodruff, J.H.; Smith, R.F. Late Emerging Effects of Prenatal and Early Postnatal Nicotine Exposure on the Cholinergic System and Anxiety-Like Behavior. Neurotoxicol. Teratol. 2010, 32, 336–345. [Google Scholar] [CrossRef]
- McCloskey, M.C.; Young, T.J.; Anderson, S.M. The Influence of Acetylcholinesterase on Anxiety- and Depression-Like Behaviors in Fluoxetine-Treated Male Mice. Bios 2017, 88, 29–38. [Google Scholar] [CrossRef]
- Mineur, Y.S.; Cahuzac, E.L.; Mose, T.N.; Bentham, M.P.; Plantenga, M.E.; Thompson, D.C.; Picciotto, M.R. Interaction between Noradrenergic and Cholinergic Signaling in Amygdala Regulates Anxiety- and Depression-Related Behaviors in Mice. Neuropsychopharmacology 2018, 43, 2118–2125. [Google Scholar] [CrossRef] [Green Version]
- Wise, T.; Patrick, F.; Meyer, N.; Mazibuko, N.; Oates, A.E.; van der Bijl, A.H.M.; Danjou, P.; O’Connor, S.M.; Doolin, E.; Wooldridge, C.; et al. Cholinergic Modulation of Disorder-Relevant Neural Circuits in Generalized Anxiety Disorder. Biol. Psychiatry 2020, 87, 908–915. [Google Scholar] [CrossRef]
- Ztaou, S.; Lhost, J.; Watabe, I.; Torromino, G.; Amalric, M. Striatal Cholinergic Interneurons Regulate Cognitive and Affective Dysfunction in Partially Dopamine-Depleted Mice. Eur. J. Neurosci. 2018, 48, 2988–3004. [Google Scholar] [CrossRef] [Green Version]
- Picciotto, M.R.; Lewis, A.S.; Van Schalkwyk, G.I.; Mineur, Y.S. Mood and Anxiety Regulation by Nicotinic Acetylcholine Receptors: A Potential Pathway to Modulate Aggression and Related Behavioral States. Neuropharmacology 2015, 96, 235–243. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Perkins, A.; Patrick, F.; Wise, T.; Meyer, N.; Mazibuko, N.; Oates, A.E.; van der Bijl, A.H.M.; Danjou, P.; O’Connor, S.M.; Doolin, E.; et al. Cholinergic Modulation of Disorder-Relevant Human Defensive Behaviour in Generalised Anxiety Disorder. Transl. Psychiatry 2021, 11. [Google Scholar] [CrossRef]
- Kerestes, R.; Harrison, B.J.; Dandash, O.; Stephanou, K.; Whittle, S.; Pujol, J.; Davey, C.G. Specific Functional Connectivity Alterations of the Dorsal Striatum in Young People with Depression. NeuroImage Clin. 2015, 7, 266–272. [Google Scholar] [CrossRef] [Green Version]
- Price, J.L.; Drevets, W.C. Neurocircuitry of Mood Disorders. Neuropsychopharmacology 2010, 35, 192–216. [Google Scholar] [CrossRef]
- Price, J.L.; Drevets, W.C. Neural Circuits Underlying the Pathophysiology of Mood Disorders. Trends Cogn. Sci. 2012, 16, 61–71. [Google Scholar] [CrossRef]
- Cullen, K.R.; Gee, D.G.; Klimes-Dougan, B.; Gabbay, V.; Hulvershorn, L.; Mueller, B.A.; Camchong, J.; Bell, C.J.; Houri, A.; Kumra, S.; et al. A Preliminary Study of Functional Connectivity in Comorbid Adolescent Depression. Neurosci. Lett. 2009, 460, 227–231. [Google Scholar] [CrossRef] [Green Version]
- Jiao, Q.; Ding, J.; Lu, G.; Su, L.; Zhang, Z.; Wang, Z.; Zhong, Y.; Li, K.; Ding, M.; Liu, Y. Increased Activity Imbalance in Fronto-Subcortical Circuits in Adolescents with Major Depression. PLoS ONE 2011, 6. [Google Scholar] [CrossRef]
- Shad, M.U.; Bidesi, A.P.; Chen, L.A.; Ernst, M.; Rao, U. Neurobiology of Decision Making in Depressed Adolescents: A Functional Magnetic Resonance Imaging Study. J. Am. Acad. Child. Adolesc. Psychiatry 2011, 50, 612–621.e2. [Google Scholar] [CrossRef] [Green Version]
- Zhu, X.; Wang, X.; Xiao, J.; Liao, J.; Zhong, M.; Wang, W.; Yao, S. Evidence of a Dissociation Pattern in Resting-State Default Mode Network Connectivity in First-Episode, Treatment-Naive Major Depression Patients. Biol. Psychiatry 2012, 71, 611–617. [Google Scholar] [CrossRef] [PubMed]
- Alexander, G.E.; DeLong, M.R.; Strick, P.L. Parallel Organization of Functionally Segregated Circuits Linking Basal Ganglia and Cortex. Annu. Rev. Neurosci. 1986, 9, 357–381. [Google Scholar] [CrossRef] [PubMed]
- Haber, S.N. The Primate Basal Ganglia: Parallel and Integrative Networks. J. Chem. Neuroanat. 2003, 26, 317–330. [Google Scholar] [CrossRef]
- Postuma, R.B.; Dagher, A. Basal Ganglia Functional Connectivity Based on a Meta-Analysis of 126 Positron Emission Tomography and Functional Magnetic Resonance Imaging Publications. Cereb. Cortex 2006, 16, 1508–1521. [Google Scholar] [CrossRef]
- Chantiluke, K.; Halari, R.; Simic, M.; Pariante, C.M.; Papadopoulos, A.; Giampietro, V.; Rubia, K. Fronto-Striato-Cerebellar Dysregulation in Adolescents with Depression during Motivated Attention. Biol. Psychiatry 2012, 71, 59–67. [Google Scholar] [CrossRef]
- Forbes, E.E.; Olino, T.M.; Ryan, N.D.; Birmaher, B.; Axelson, D.; Moyles, D.L.; Dahl, R.E. Reward-Related Brain Function as a Predictor of Treatment Response in Adolescents with Major Depressive Disorder. Cogn. Affect. Behav. Neurosci. 2010, 10, 107–118. [Google Scholar] [CrossRef]
- Forbes, E.E.; Christopher May, J.; Siegle, G.J.; Ladouceur, C.D.; Ryan, N.D.; Carter, C.S.; Birmaher, B.; Axelson, D.A.; Dahl, R.E. Reward-Related Decision-Making in Pediatric Major Depressive Disorder: An Fmri Study. J. Child. Psychol. Psychiatry Allied Discip. 2006, 47, 1031–1040. [Google Scholar] [CrossRef] [Green Version]
- Furman, D.J.; Hamilton, J.P.; Gotlib, I.H. Frontostriatal Functional Connectivity in Major Depressive Disorder. Biol. Mood Anxiety Disord. 2011, 1. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gabbay, V.; Ely, B.A.; Li, Q.; Bangaru, S.D.; Panzer, A.M.; Alonso, C.M.; Castellanos, F.X.; Milham, M.P. Striatum-Based Circuitry of Adolescent Depression and Anhedonia. J. Am. Acad. Child. Adolesc. Psychiatry 2013, 52, 628–641.e13. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Calhoon, G.G.; Tye, K.M. Resolving the Neural Circuits of Anxiety. Nat. Neurosci. 2015, 18, 1394–1404. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Davis, M.; Walker, D.L.; Miles, L.; Grillon, C. Phasic vs Sustained Fear in Rats and Humans: Role of the Extended Amygdala in Fear vs Anxiety. Neuropsychopharmacology 2010, 35, 105–135. [Google Scholar] [CrossRef] [Green Version]
- Lago, T.; Davis, A.; Grillon, C.; Ernst, M. Striatum on the Anxiety Map: Small Detours into Adolescence. Brain Res. 2017, 1654, 177–184. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Drevets, W.C.; Furey, M.L. Replication of Scopolamine’s Antidepressant Efficacy in Major Depressive Disorder: A Randomized, Placebo-Controlled Clinical Trial. Biol. Psychiatry 2010, 67, 432–438. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kasper, S.; Moises, H.W.; Beckmann, H. The Anticholinergic Biperiden in Depressive Disorders. Pharmacopsychiatria 1981, 14, 195–198. [Google Scholar] [CrossRef]
- Beckmann, H.; Moises, H.W. The Cholinolytic Biperiden in Depression—An Acute Placebo Controlled Study. Arch. Psychiatry Nervenkr. 1982, 231, 213–220. [Google Scholar] [CrossRef] [PubMed]
- Gillin, J.C.; Lauriello, J.; Kelsoe, J.R.; Rapaport, M.; Golshan, S.; Kenny, W.M.; Sutton, L. No Antidepressant Effect of Biperiden Compared with Placebo in Depression: A Double-Blind 6-Week Clinical Trial. Psychiatry Res. 1995, 58, 99–105. [Google Scholar] [CrossRef]
- Newhouse, P.A.; Sunderland, T.; Tariot, P.N.; Weingartner, H.; Thompson, K.; Mellow, A.M.; Cohen, R.M.; Murphy, D.L. The Effects of Acute Scopolamine in Geriatric Depression. Arch. Gen. Psychiatry 1988, 45, 906–912. [Google Scholar] [CrossRef]
- Gillin, J.C.; Sutton, L.; Ruiz, C.; Darko, D.; Golshan, S.; Risch, S.C.; Janowsky, D. The Effects of Scopolamine on Sleep and Mood in Depressed Patients with a History of Alcoholism and a Normal Comparison Group. Biol. Psychiatry 1991, 30, 157–169. [Google Scholar] [CrossRef]
- Furey, M.L.; Drevets, W.C. Antidepressant Efficacy of the Antimuscarinic Drug Scopolamine: A Randomized, Placebo-Controlled Clinical Trial. Arch. Gen. Psychiatry 2006, 63, 1121–1129. [Google Scholar] [CrossRef]
- Hesselink, J.M.K.; Cummings, J.L. Serotonin and Parkinson’s Disease. Am. J. Psychiatry 1993, 150, 843–844. [Google Scholar] [CrossRef] [PubMed]
- Steur, E.N.H.J. Increase of Parkinson Disability after Fluoxetine Medication. Neurology 1993, 43, 211–213. [Google Scholar] [CrossRef]
- Birkmayer, W. Deprenyl (Selegiline) in the Treatment of Parkinson’s Disease. Acta Neurol. Scand. 1983, 68, 103–106. [Google Scholar] [CrossRef]
- McDowell, F.; Cedarbaum, J. The Extrapyramidal System and Disorders of Movement. In Clinical Neurology; Joynt, R., Ed.; J. B. Lippincott Co.: Philadelphia, PA, USA, 1991; pp. 1–116. [Google Scholar]
- Ungvari, G.; Karczag, I.; Gerevich, J.; Petho, B. Clinical Notes on the Possible Anticholinergic Reversal of Depressive Syndromes. Pharmacopsychiatria 1981, 14, 71–73. [Google Scholar] [CrossRef]
- Coid, J.; Strang, J. Mania Secondary to Procyclidine (‘Kemadrin’) Abuse. Br. J. Psychiatry 1982, 141, 81–84. [Google Scholar] [CrossRef]
- Rubinstein, J.S. Abuse of Antiparkinsonism Drugs: Feigning of Extrapyramidal Symptoms to Obtain Trihexyphenidyl. JAMA J. Am. Med. Assoc. 1978, 239, 2365–2366. [Google Scholar] [CrossRef]
- Macvicar, K. Abuse of Antiparkinsonian Drugs by Psychiatric Patients. Am. J. Psychiatry 1977, 134, 809–811. [Google Scholar] [CrossRef]
- Goggin, D.A.; Solomon, G.F. Trihexyphenidyl Abuse for Euphorigenic Effect. Am. J. Psychiatry 1979, 136, 459–460. [Google Scholar] [CrossRef]
- Carvalho, M.M.; Campos, F.L.; Coimbra, B.; Pêgo, J.M.; Rodrigues, C.; Lima, R.; Rodrigues, A.J.; Sousa, N.; Salgado, A.J. Behavioral Characterization of the 6-Hydroxidopamine Model of Parkinson’s Disease and Pharmacological Rescuing of Non-Motor Deficits. Mol. Neurodegener. 2013, 8, 14. [Google Scholar] [CrossRef] [Green Version]
- Campos, F.L.; Carvalho, M.M.; Cristovão, A.C.; Je, G.; Baltazar, G.; Salgado, A.J.; Kim, Y.-S.S.; Sousa, N. Rodent Models of Parkinson’s Disease: Beyond the Motor Symptomatology. Front. Behav. Neurosci. 2013, 7, 175. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Liu, K.C.; Li, J.Y.; Tan, H.H.; Du, C.X.; Xie, W.; Zhang, Y.M.; Ma, W.L.; Zhang, L. Serotonin6 Receptors in the Dorsal Hippocampus Regulate Depressive-Like Behaviors in Unilateral 6-Hydroxydopamine-Lesioned Parkinson’s Rats. Neuropharmacology 2015, 95, 290–298. [Google Scholar] [CrossRef] [PubMed]
- Hui, Y.P.; Zhang, Q.J.; Zhang, L.; Chen, L.; Guo, Y.; Qiao, H.F.; Wang, Y.; Liu, J. Activation of Prelimbic 5-HT1A Receptors Produces Antidepressant-Like Effects in a Unilateral Rat Model of Parkinson’s Disease. Neuroscience 2014, 268, 265–275. [Google Scholar] [CrossRef] [PubMed]
- Bonito-Oliva, A.; Masini, D.; Fisone, G. A Mouse Model of Non-Motor Symptoms in Parkinson’s Disease: Focus on Pharmacological Interventions Targeting Affective Dysfunctions. Front. Behav. Neurosci. 2014, 8, 290. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bonito-Oliva, A.; Pignatelli, M.; Spigolon, G.; Yoshitake, T.; Seiler, S.; Longo, F.; Piccinin, S.; Kehr, J.; Mercuri, N.B.; Nisticò, R.; et al. Cognitive Impairment and Dentate Gyrus Synaptic Dysfunction in Experimental Parkinsonism. Biol. Psychiatry 2014, 75, 701–710. [Google Scholar] [CrossRef]
- Favier, M.; Duran, T.; Carcenac, C.; Drui, G.; Savasta, M.; Carnicella, S. Pramipexole Reverses Parkinson’s Disease-Related Motivational Deficits in Rats. Mov. Disord. 2014, 29, 912–920. [Google Scholar] [CrossRef]
- Carnicella, S.; Drui, G.; Boulet, S.; Carcenac, C.; Favier, M.; Duran, T.; Savasta, M. Implication of Dopamine D3 Receptor Activation in the Reversion of Parkinson’s Disease-Related Motivational Deficits. Transl. Psychiatry 2014, 4. [Google Scholar] [CrossRef]
- Drui, G.; Carnicella, S.; Carcenac, C.; Favier, M.; Bertrand, A.; Boulet, S.; Savasta, M. Loss of Dopaminergic Nigrostriatal Neurons Accounts for the Motivational and Affective Deficits in Parkinson’s Disease. Mol. Psychiatry 2014, 19, 358–367. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Santiago, R.M.; Barbiero, J.; Gradowski, R.W.; Bochen, S.; Lima, M.M.S.; Da Cunha, C.; Andreatini, R.; Vital, M.A.B.F. Induction of Depressive-Like Behavior by Intranigral 6-OHDA Is Directly Correlated with Deficits in Striatal Dopamine and Hippocampal Serotonin. Behav. Brain Res. 2014, 259, 70–77. [Google Scholar] [CrossRef]
- Branchi, I.; D’Andrea, I.; Armida, M.; Cassano, T.; Pèzzola, A.; Potenza, R.L.; Morgese, M.G.; Popoli, P.; Alleva, E. Nonmotor Symptoms in Parkinson’s Disease: Investigating Early-Phase Onset of Behavioral Dysfunction in the 6-Hydroxydopamine-Lesioned Rat Model. J. Neurosci. Res. 2008, 86, 2050–2061. [Google Scholar] [CrossRef] [PubMed]
- Tadaiesky, M.T.; Dombrowski, P.A.; Figueiredo, C.P.; Cargnin-Ferreira, E.; Da Cunha, C.; Takahashi, R.N. Emotional, Cognitive and Neurochemical Alterations in a Premotor Stage Model of Parkinson’s Disease. Neuroscience 2008, 156, 830–840. [Google Scholar] [CrossRef]
- Eskow Jaunarajs, K.L.; George, J.A.; Bishop, C. L-DOPA-Induced Dysregulation of Extrastriatal Dopamine and Serotonin and Affective Symptoms in a Bilateral Rat Model of Parkinson’s Disease. Neuroscience 2012, 218, 243–256. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Eskow Jaunarajs, K.L.; Dupre, K.B.; Ostock, C.Y.; Button, T.; Deak, T.; Bishop, C. Behavioral and Neurochemical Effects of Chronic L-DOPA Treatment on Nonmotor Sequelae in the Hemiparkinsonian Rat. Behav. Pharmacol. 2010, 21, 627–637. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sun, W.; Sugiyama, K.; Fang, X.; Yamaguchi, H.; Akamine, S.; Magata, Y.; Namba, H. Different Striatal D2-Like Receptor Function in an Early Stage after Unilateral Striatal Lesion and Medial Forebrain Bundle Lesion in Rats. Brain Res. 2010, 1317, 227–235. [Google Scholar] [CrossRef] [Green Version]
- Delaville, C.; Chetrit, J.; Abdallah, K.; Morin, S.; Cardoit, L.; De Deurwaerdère, P.; Benazzouz, A. Emerging Dysfunctions Consequent to Combined Monoaminergic Depletions in Parkinsonism. Neurobiol. Dis. 2012, 45, 763–773. [Google Scholar] [CrossRef]
- Winter, L.; Spiegel, J. Botulinum Toxin Type-A in the Treatment of Glabellar Lines. Clin. Cosmet. Investig. Dermatol. 2010, 3, 1–4. [Google Scholar] [CrossRef] [Green Version]
- Jungnickel, J.; Kalve, I.; Reimers, L.; Nobre, A.; Wesemann, M.; Ratzka, A.; Halfer, N.; Lindemann, C.; Schwabe, K.; Töllner, K.; et al. Topology of Intrastriatal Dopaminergic Grafts Determines Functional and Emotional Outcome in Neurotoxin-Lesioned Rats. Behav. Brain Res. 2011, 216, 129–135. [Google Scholar] [CrossRef] [PubMed]
- Kuan, W.L.; Zhao, J.W.; Barker, R.A. The Role of Anxiety in the Development of Levodopa-Induced Dyskinesias in an Animal Model of Parkinson’s Disease, and the Effect of Chronic Treatment with the Selective Serotonin Reuptake Inhibitor Citalopram. Psychopharmacology 2008, 197, 279–293. [Google Scholar] [CrossRef] [PubMed]
- Jankovic, J. Botulinum Toxin: State of the Art. Mov. Disord. 2017, 32, 1131–1138. [Google Scholar] [CrossRef]
- Jankovic, J.; Orman, J. Botulinum a Toxin for Cranial-Cervicaldystonia: A Double-Blind, Placebo-Controlled Study. Neurology 1987, 37, 616–623. [Google Scholar] [CrossRef] [PubMed]
- Anandan, C.; Jankovic, J. Botulinum Toxin in Movement Disorders: An Update. Toxins 2021, 13, 42. [Google Scholar] [CrossRef]
- Jocson, A.; Lew, M. Use of Botulinum Toxin in Parkinson’s Disease. Park. Relat. Disord. 2019, 59, 57–64. [Google Scholar] [CrossRef]
- Espay, A.J.; Vaughan, J.E.; Shukla, R.; Gartner, M.; Sahay, A.; Revilla, F.J.; Duker, A.P. Botulinum Toxin Type A for Levodopa-Induced Cervical Dyskinesias in Parkinson’s Disease: Unfavorable Risk-Benefit Ratio. Mov. Disord. 2011, 26, 913–914. [Google Scholar] [CrossRef] [PubMed]
- Cardoso, F. Botulinum Toxin in Parkinsonism: The When, How, and Which for Botulinum Toxin Injections. Toxicon 2018, 147, 107–110. [Google Scholar] [CrossRef]
- Jankovic, J. Disease-Oriented Approach to Botulinum Toxin Use. Toxicon 2009, 54, 614–623. [Google Scholar] [CrossRef]
- Rieu, I.; Degos, B.; Castelnovo, G.; Vial, C.; Durand, E.; Pereira, B.; Simonetta-Moreau, M.; Sangla, S.; Fluchère, F.; Guehl, D.; et al. Incobotulinum Toxin A in Parkinson’s Disease with Foot Dystonia: A Double Blind Randomized Trial. Park. Relat. Disord. 2018, 46, 9–15. [Google Scholar] [CrossRef]
- Cordivari, C.; Misra, P.V.; Catania, S.; Less, A.J. Treatment of Dystonic Clenched Fist with Botulinum Toxin. Mov. Disord. 2001, 16, 907–913. [Google Scholar] [CrossRef] [PubMed]
- Sheffield, J.K.; Jankovic, J. Botulinum Toxin in the Treatment of Tremors, Dystonias, Sialorrhea and Other Symptoms Associated with Parkinson’s Disease. Expert Rev. Neurother. 2007, 7, 637–647. [Google Scholar] [CrossRef] [PubMed]
- Schneider, S.A.; Edwards, M.J.; Cordivari, C.; Macleod, W.N.; Bhatia, K.P. Botulinum Toxin A May Be Efficacious as Treatment for Jaw Tremor in Parkinson’s Disease. Mov. Disord. 2006, 21, 1722–1724. [Google Scholar] [CrossRef] [PubMed]
- Rahimi, F.; Samotus, O.; Lee, J.; Jog, M. Effective Management of Upper Limb Parkinsonian Tremor by Incobotulinumtoxina Injections Using Sensor-Based Biomechanical Patterns. Tremor Other Hyperkinet. Mov. 2015, 5, 348. [Google Scholar] [CrossRef]
- Mittal, S.O.; Machado, D.; Richardson, D.; Dubey, D.; Jabbari, B. Botulinum Toxin in Parkinson Disease Tremor: A Randomized, Double-Blind, Placebo-Controlled Study with a Customized Injection Approach. Mayo Clin. Proc. 2017, 92, 1359–1367. [Google Scholar] [CrossRef]
- Fernandez, H.H.; Lannon, M.C.; Trieschmann, M.E.; Friedman, J.H. Botulinum Toxin Type B for Gait Freezing in Parkinson’s Disease. Med. Sci. Monit. 2004, 10, CR282–CR284. [Google Scholar] [PubMed]
- Vaštík, M.; Hok, P.; Hluštík, P.; Otruba, P.; Tüdös, Z.; Kanovsky, P. Botulinum Toxin Treatment of Freezing of Gait in Parkinson’s Disease Patients as Reflected in Functional Magnetic Resonance Imaging of Leg Movement. Neuroendocrinol. Lett. 2016, 37, 147–153. [Google Scholar]
- Gurevich, T.; Peretz, C.; Moore, O.; Weizmann, N.; Giladi, N. The Effect of Injecting Botulinum Toxin Type A into the Calf Muscles on Freezing of Gait in Parkinson’s Disease: A Double Blind Placebo-Controlled Pilot Study. Mov. Disord. 2007, 22, 880–883. [Google Scholar] [CrossRef]
- Giladi, N.; Gurevich, T.; Shabtai, H.; Paleacu, D.; Simon, E.S. The Effect of Botulinum Toxin Injections to the Calf Muscles on Freezing of Gait in Parkinsonism: A Pilot Study. J. Neurol. 2001, 248, 572–576. [Google Scholar] [CrossRef] [PubMed]
- Santamato, A.; Ianieri, G.; Ranieri, M.; Megna, M.; Panza, F.; Fiore, P.; Megna, G. Botulinum Toxin Type a in the Treatment of Sialorrhea in Parkinson’s Disease. J. Am. Geriatr. Soc. 2008, 56, 765–767. [Google Scholar] [CrossRef]
- Narayanaswami, P.; Geisbush, T.; Tarulli, A.; Raynor, E.; Gautam, S.; Tarsy, D.; Gronseth, G. Drooling in Parkinson’s Disease: A Randomized Controlled Trial of Incobotulinum Toxin A and Meta-Analysis of Botulinum Toxins. Park. Relat. Disord. 2016, 30, 73–77. [Google Scholar] [CrossRef] [PubMed]
- Lagalla, G.; Millevolte, M.; Capecci, M.; Provinciali, L.; Ceravolo, M.G. Botulinum Toxin Type A for Drooling in Parkinson’s Disease: A Double-Blind, Randomized, Placebo-Controlled Study. Mov. Disord. 2006, 21, 704–707. [Google Scholar] [CrossRef] [PubMed]
- Mancini, F.; Zangaglia, R.R.; Cristina, S.; Sommaruga, M.G.; Martignoni, E.; Nappi, G.; Pacchetti, C. Double-Blind, Placebo-Controlled Study to Evaluate the Efficacy and Safety of Botulinum Toxin Type A in the Treatment of Drooling Parkinsonism. Mov. Disord. 2003, 18, 685–688. [Google Scholar] [CrossRef] [PubMed]
- Chinnapongse, R.; Gullo, K.; Nemeth, P.; Zhang, Y.; Griggs, L. Safety and Efficacy of Botulinum Toxin Type B for Treatment of Sialorrhea in Parkinson’s Disease: A Prospective Double-Blind Trial. Mov. Disord. 2012, 27, 219–226. [Google Scholar] [CrossRef] [PubMed]
- Giannantoni, A.; Rossi, A.; Mearini, E.; Del Zingaro, M.; Porena, M.; Berardelli, A. Botulinum Toxin A for Overactive Bladder and Detrusor Muscle Overactivity in Patients with Parkinson’s Disease and Multiple System Atrophy. J. Urol. 2009, 182, 1453–1457. [Google Scholar] [CrossRef]
- Giannantoni, A.; Conte, A.; Proietti, S.; Giovannozzi, S.; Rossi, A.; Fabbrini, G.; Porena, M.; Berardelli, A. Botulinum Toxin Type A in Patients with Parkinson’s Disease and Refractory Overactive Bladder. J. Urol. 2011, 186, 960–964. [Google Scholar] [CrossRef]
- Anderson, R.U.; Orenberg, E.K.; Glowe, P. Onabotulinum Toxin A Office Treatment for Neurogenic Bladder Incontinence in Parkinson’s Disease. Urology 2014, 83, 22–27. [Google Scholar] [CrossRef]
- Vurture, G.; Peyronnet, B.; Feigin, A.; Biagioni, M.C.; Gilbert, R.; Rosenblum, N.; Frucht, S.; Di Rocco, A.; Nitti, V.W.; Brucker, B.M. Outcomes of Intradetrusor Onabotulinum Toxin A Injection in Patients with Parkinson’s Disease. Neurourol. Urodyn. 2018, 37, 2669–2677. [Google Scholar] [CrossRef]
- Cadeddu, F.; Bentivoglio, A.R.; Brandara, F.; Marniga, G.; Brisinda, G.; Maria, G. Outlet Type Constipation in Parkinson’s Disease: Results of Botulinum Toxin Treatment. Aliment. Pharmacol. Ther. 2005, 22, 997–1003. [Google Scholar] [CrossRef]
- Albanese, A.; Brisinda, G.; Bentivoglio, A.R.; Maria, G. Treatment of outlet obstruction constipation in Parkinson’s disease with botulinum neurotoxin a. Am. J. Gastroenterol. 2003, 98, 1439–1440. [Google Scholar] [CrossRef]
- Azher, S.N.; Jankovic, J. Camptocormia: Pathogenesis, Classification, and Response to Therapy. Neurology 2005, 65, 355–359. [Google Scholar] [CrossRef] [PubMed]
- Fietzek, U.M.; Schroeteler, F.E.; Ceballos-Baumann, A.O. Goal Attainment After Treatment of Parkinsonian Camptocormia with Botulinum Toxin. Mov. Disord. 2009, 24, 2027–2028. [Google Scholar] [CrossRef] [PubMed]
- Von Coelln, R.; Raible, A.; Gasser, T.; Asmus, F. Ultrasound-Guided Injection of the Iliopsoas Muscle with Botulinum Toxin in Camptocormia. Mov. Disord. 2008, 23, 889–892. [Google Scholar] [CrossRef] [PubMed]
- Tassorelli, C.; De Icco, R.; Alfonsi, E.; Bartolo, M.; Serrao, M.; Avenali, M.; De Paoli, I.; Conte, C.; Pozzi, N.G.; Bramanti, P.; et al. Botulinum Toxin Type A Potentiates The Effect of Neuromotor Rehabilitation of Pisa Syndrome in Parkinson Disease: A Placebo Controlled Study. Park. Relat. Disord. 2014, 20, 1140–1144. [Google Scholar] [CrossRef] [PubMed]
- Artusi, C.A.; Bortolani, S.; Merola, A.; Zibetti, M.; Busso, M.; De Mercanti, S.; Arnoffi, P.; Martinetto, S.; Gaidolfi, E.; Veltri, A.; et al. Botulinum Toxin for Pisa Syndrome: An MRI-, Ultrasound-And Electromyography-Guided Pilot Study. Park. Relat. Disord. 2019, 62, 231–235. [Google Scholar] [CrossRef] [PubMed]
- Alfonsi, E.; Merlo, I.M.; Ponzio, M.; Montomoli, C.; Tassorelli, C.; Biancardi, C.; Lozza, A.; Martignoni, E. An Electrophysiological Approach to the Diagnosis of Neurogenic Dysphagia: Implications for Botulinum Toxin Treatment. J. Neurol. Neurosurg. Psychiatry 2010, 81, 54–60. [Google Scholar] [CrossRef] [Green Version]
- Restivo, D.A.; Palmeri, A.; Marchese-Ragona, R. Botulinum Toxin for Cricopharyngeal Dysfunction in Parkinson’s Disease. N. Engl. J. Med. 2002, 346, 1174–1175. [Google Scholar] [CrossRef]
- Martinez-Ramirez, D.; Giugni, J.C.; Hastings, E.; Shukla, A.W.; Malaty, I.A.; Okun, M.S.; Rodriguez, R.L. Comparable Botulinum Toxin Outcomes between Primary and Secondary Blepharospasm: A Retrospective Analysis. Tremor Other Hyperkinet. Mov. 2014, 4, 286. [Google Scholar] [CrossRef]
- Lepore, V.; Defazio, G.; Acquistapace, D.; Melpignano, C.; Pomes, L.; Lamberti, P.; Livrea, P.; Ferrari, E. Botulinum A Toxin for the So-Called Apraxia of Lid Opening. Mov. Disord. 1995, 10, 525–526. [Google Scholar] [CrossRef]
- Hall, C.; Ballachey, E.L. A Study of The Rat’s Behavior in A Field. A Contribution to Method in Comparative Psychology. Univ. Calif. Publ. Psychol. 1932, 6, 1–12. [Google Scholar]
- Prut, L.; Belzung, C. The Open Field as a Paradigm to Measure the Effects of Drugs on Anxiety-Like Behaviors: A Review. Eur. J. Pharmacol. 2003, 463, 3–33. [Google Scholar] [CrossRef]
- Zimcikova, E.; Simko, J.; Karesova, I.; Kremlacek, J.; Malakova, J. Behavioral Effects of Antiepileptic Drugs in Rats: Are the Effects on Mood and Behavior Detectable in Open-Field Test? Seizure 2017, 52, 35–40. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Dawson, G.R.; Tricklebank, M.D. Use of the Elevated Plus Maze in the Search for Novel Anxiolytic Agents. Trends Pharmacol. Sci. 1995, 16, 33–36. [Google Scholar] [CrossRef]
- Haller, J.; Alicki, M. Current Animal Models of Anxiety, Anxiety Disorders, and Anxiolytic Drugs. Curr. Opin. Psychiatry 2012, 25, 59–64. [Google Scholar] [CrossRef]
- Carobrez, A.P.; Bertoglio, L.J. Ethological and Temporal Analyses of Anxiety-Like Behavior: The Elevated Plus-Maze Model 20 Years on. Neurosci. Biobehav. Rev. 2005, 29, 1193–1205. [Google Scholar] [CrossRef]
- Borsini, F.; Meli, A. Is the Forced Swimming Test A Suitable Model for Revealing Antidepressant Activity? Psychopharmacology 1988, 94, 147–160. [Google Scholar] [CrossRef] [PubMed]
- Brotto, L.A.; Gorzalka, B.B.; Barr, A.M. Paradoxical Effects of Chronic Corticosterone on Forced Swim Behaviours in Aged Male and Female Rats. Eur. J. Pharmacol. 2001, 424, 203–209. [Google Scholar] [CrossRef]
- Slattery, D.A.; Cryan, J.F. Using the Rat Forced Swim Test to Assess Antidepressant-Like Activity in Rodents. Nat. Protoc. 2012, 7, 1009–1014. [Google Scholar] [CrossRef]
- Warden, M.R.; Selimbeyoglu, A.; Mirzabekov, J.J.; Lo, M.; Thompson, K.R.; Kim, S.Y.; Adhikari, A.; Tye, K.M.; Frank, L.M.; Deisseroth, K. A Prefrontal Cortex-Brainstem Neuronal Projection that Controls Response to Behavioural Challenge. Nature 2012, 492, 428–432. [Google Scholar] [CrossRef]
- Campus, P.; Colelli, V.; Orsini, C.; Sarra, D.; Cabib, S. Evidence for the Involvement of Extinction-Associated Inhibitory Learning in the Forced Swimming Test. Behav. Brain Res. 2015, 278, 348–355. [Google Scholar] [CrossRef]
- Steru, L.; Chermat, R.; Thierry, B.; Simon, P. The Tail Suspension Test: A New Method for Screening Antidepressants in Mice. Psychopharmacology 1985, 85, 367–370. [Google Scholar] [CrossRef]
- Thierry, B.; Stéru, L.; Simon, P.; Porsolt, R.D. The tail suspension test: Ethical considerations. Psychopharmacology 1986, 90, 284–285. [Google Scholar] [CrossRef] [PubMed]
- Zou, T.; Zhang, J.; Liu, Y.; Zhang, Y.; Sugimoto, K.; Mei, C. Antidepressant-Like Effect of Geniposide in Mice Exposed to a Chronic Mild Stress Involves the Microrna-298-5p-Mediated Nox1. Front. Mol. Neurosci. 2021, 13, 131. [Google Scholar] [CrossRef]
- Martinez-Martin, P. The Importance of Non-Motor Disturbances to Quality of Life in Parkinson’s Disease. J. Neurol. Sci. 2011, 310, 12–16. [Google Scholar] [CrossRef] [PubMed]
- Ziemssen, T.; Reichmann, H. Non-Motor Dysfunction in Parkinson’s Disease. Park. Relat. Disord. 2007, 13, 323–332. [Google Scholar] [CrossRef]
- Marques, A.; Figorilli, M.; Lambert, C.; Pereira, B.; Vidal, T.; Montplaisir, J.; Durif, F.; Livia Fantini, M. The Urge to Move: From Restless Legs Syndrome to Impulse Control Disorders in Parkinson’s Disease. J. Sleep Res. 2021, 30. [Google Scholar] [CrossRef] [PubMed]
- Salawu, F.K.; Danburam, A.; Olokoba, A.B. Non-Motor Symptoms of Parkinson’s Disease: Diagnosis and Management. Niger. J. Med. 2010, 19, 126–131. [Google Scholar] [CrossRef]
- Stacy, M.; Bowron, A.; Guttman, M.; Hauser, R.; Hughes, K.; Larsen, J.P.; Le Witt, P.; Oertel, W.; Quinn, N.; Sethi, K.; et al. Identification of Motor and Nonmotor Wearing-Off in Parkinson’s Disease: Comparison of a Patient Questionnaire Versus a Clinician Assessment. Mov. Disord. 2005, 20, 726–733. [Google Scholar] [CrossRef]
- Wolters, E.C. Non-Motor Extranigral Signs and Symptoms in Parkinson’s Disease. Park. Relat. Disord. 2009, 15. [Google Scholar] [CrossRef]
- Burn, D.J. Beyond the Iron Mask: Towards Better Recognition and Treatment of Depression Associated with Parkinson’s Disease. Mov. Disord. 2002, 17, 445–454. [Google Scholar] [CrossRef]
- Weisskopf, M.G.; Chen, H.; Schwarzschild, M.A.; Kawachi, I.; Ascherio, A. Prospective Study of Phobic Anxiety and Risk of Parkinson’s Disease. Mov. Disord. 2003, 18, 646–651. [Google Scholar] [CrossRef]
- Shiba, M.; Bower, J.H.; Maraganore, D.M.; McDonnell, S.K.; Peterson, B.J.; Ahlskog, J.E.; Schaid, D.J.; Rocca, W.A. Anxiety Disorders And Depressive Disorders Preceding Parkinson’s Disease: A Case-Control Study. Mov. Disord. 2000, 15, 669–677. [Google Scholar] [CrossRef]
- Shulman, L.M.; Taback, R.L.; Rabinstein, A.A.; Weiner, W.J. Non-Recognition of Depression and Other Non-Motor Symptoms In Parkinson’s Disease. Park. Relat. Disord. 2002, 8, 193–197. [Google Scholar] [CrossRef]
- Sullivan, K.L.; Ward, C.L.; Hauser, R.A.; Zesiewicz, T.A. Prevalence and Treatment of Non-Motor Symptoms in Parkinson’s Disease. Park. Relat. Disord. 2007, 13, 545. [Google Scholar] [CrossRef] [PubMed]
- Thompson, A.W.; Liu, H.; Hays, R.D.; Katon, W.J.; Rausch, R.; Diaz, N.; Jacob, E.L.; Vassar, S.D.; Vickrey, B.G. Diagnostic Accuracy and Agreement Across Three Depression Assessment Measures for Parkinson’s Disease. Park. Relat. Disord. 2011, 17, 40–45. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Dissanayaka, N.N.N.W.; White, E.; O’Sullivan, J.D.; Marsh, R.; Pachana, N.A.; Byrne, G.J. The Clinical Spectrum of Anxiety in Parkinson’s Disease. Mov. Disord. 2014, 29, 967–975. [Google Scholar] [CrossRef] [PubMed]
- Nilsson, F.M.; Kessing, L.V.; Bolwig, T.G. Increased Risk of Developing Parkinson’s Disease for Patients with Major Affective Disorder: A Register Study. Acta Psychiatr. Scand. 2001, 104, 380–386. [Google Scholar] [CrossRef] [PubMed]
- Zhuo, C.; Xue, R.; Luo, L.; Ji, F.; Tian, H.; Qu, H.; Lin, X.; Jiang, R.; Tao, R. Efficacy of Antidepressive Medication for Depression in Parkinson Disease: A Network Meta-Analysis. Medicine 2017, 96. [Google Scholar] [CrossRef]
- Barone, P.; Santangelo, G.; Morgante, L.; Onofrj, M.; Meco, G.; Abbruzzese, G.; Bonuccelli, U.; Cossu, G.; Pezzoli, G.; Stanzione, P.; et al. A Randomized Clinical Trial to Evaluate the Effects of Rasagiline on Depressive Symptoms in Non-Demented Parkinson’s Disease Patients. Eur. J. Neurol. 2015, 22, 1184–1191. [Google Scholar] [CrossRef]
- Weintraub, D.; Mavandadi, S.; Mamikonyan, E.; Siderowf, A.D.; Duda, J.E.; Hurtig, H.I.; Colcher, A.; Horn, S.S.; Nazem, S.; Ten Have, T.R.; et al. Atomoxetine for Depression and Other Neuropsychiatric Symptoms in Parkinson Disease. Neurology 2010, 75, 448–455. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Menza, M.; Dobkin, R.D.; Marin, H.; Mark, M.H.; Gara, M.; Buyske, S.; Bienfait, K.; Dicke, A. A Controlled Trial of Antidepressants in Patients with Parkinson Disease and Depression. Neurology 2009, 72, 886–892. [Google Scholar] [CrossRef] [PubMed]
- Pålhagen, S.; Qi, H.; Mårtensson, B.; Wålinder, J.; Granérus, A.K.; Svenningsson, P. Monoamines, BDNF, IL-6 and Corticosterone in CSF in Patients with Parkinson’s Disease and Major Depression. J. Neurol. 2010, 257, 524–532. [Google Scholar] [CrossRef]
- Axel Wollmer, M.; Kalak, N.; Jung, S.; de Boer, C.; Magid, M.; Reichenberg, J.S.; Brand, S.; Holsboer-Trachsler, E.; Kruger, T.H.C. Agitation Predicts Response of Depression to Botulinum Toxin Treatment in a Randomized Controlled Trial. Front. Psychiatry 2014, 5. [Google Scholar] [CrossRef] [Green Version]
- Wollmer, M.A.; De Boer, C.; Kalak, N.; Beck, J.; Götz, T.; Schmidt, T.; Hodzic, M.; Bayer, U.; Kollmann, T.; Kollewe, K.; et al. Facing Depression with Botulinum Toxin: A Randomized Controlled Trial. J. Psychiatr. Res. 2012, 46, 574–581. [Google Scholar] [CrossRef] [Green Version]
- Finzi, E.; Rosenthal, N.E. Treatment of Depression with Onabotulinum toxina: A Randomized, Double-Blind, Placebo Controlled Trial. J. Psychiatr. Res. 2014, 52, 1–6. [Google Scholar] [CrossRef]
- Finzi, E.; Rosenthal, N.E. Emotional Proprioception: Treatment of Depression with Afferent Facial Feedback. J. Psychiatr. Res. 2016, 80, 93–96. [Google Scholar] [CrossRef]
- Magid, M.; Reichenberg, J.S.; Poth, P.E.; Robertson, H.T.; LaViolette, A.K.; Kruger, T.H.C.; Wollmer, M.A. Treatment of Major Depressive Disorder Using Botulinum Toxin A: A 24-Week Randomized, Double-Blind, Placebo-Controlled Study. J. Clin. Psychiatry 2014, 75, 837–844. [Google Scholar] [CrossRef]
- Lewis, M.B. The Interactions Between Botulinum-Toxin-Based Facial Treatments and Embodied Emotions. Sci. Rep. 2018, 8. [Google Scholar] [CrossRef] [PubMed]
- Kim, M.J.; Neta, M.; Davis, F.C.; Ruberry, E.J.; Dinescu, D.; Heatherton, T.F.; Stotland, M.A.; Whalen, P.J. Botulinum Toxin-Induced Facial Muscle Paralysis Affects Amygdala Responses to the Perception of Emotional Expressions: Preliminary Findings from an A-B-A Design. Biol. Mood Anxiety Disord. 2014, 4, 11. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Brennan, C. Botulinum Toxin Type—A (BoNT-A) Injections of the Corrugator Muscles for Aesthetics and Depression? Plast. Surg. Nurs. 2016, 36, 167–169. [Google Scholar] [CrossRef] [PubMed]
- Khademi, M.; Roohaninasab, M.; Goodarzi, A.; Seirafianpour, F.; Dodangeh, M.; Khademi, A. The Healing Effects of Facial BOTOX Injection on Symptoms of Depression Alongside Its Effects on Beauty Preservation. J. Cosmet. Dermatol. 2021, 20, 1411–1415. [Google Scholar] [CrossRef]
- Kruger, T.H.C.; Wollmer, M.A. Depression—An Emerging Indication for Botulinum Toxin Treatment. Toxicon 2015, 107, 154–157. [Google Scholar] [CrossRef] [PubMed]
- De Boulle, K.; Fagien, S.; Sommer, B.; Glogau, R. Treating Glabellar Lines with Botulinum Toxin Type A-Hemagglutinin Complex: A Review of the Science, the Clinical Data, and Patient Satisfaction. Clin. Interv. Aging 2010, 5, 101–118. [Google Scholar] [CrossRef] [Green Version]
- Rzany, B.; Dill-Müller, D.; Grablowitz, D.; Heckmann, M.; Caird, D. Repeated Botulinum Toxin A Injections for the Treatment of Lines in the Upper Face: A Retrospective Study of 4,103 Treatments in 945 Patients. Dermatol. Surg. 2007, 33. [Google Scholar] [CrossRef]
- Lewis, M.B.; Bowler, P.J. Botulinum Toxin Cosmetic Therapy Correlates with a More Positive Mood. J. Cosmet. Dermatol. 2009, 8, 24–26. [Google Scholar] [CrossRef]
- Finzi, E.; Wasserman, E. Treatment of Depression with Botulinum Toxin A: A Case Series. Dermatol. Surg. 2006, 32, 645–650. [Google Scholar] [CrossRef]
- Sommer, B.; Zschocke, I.; Bergfeld, D.; Sattler, G.; Augustin, M. Satisfaction of Patients after Treatment with Botulinum Toxin for Dynamic Facial Lines. Dermatol. Surg. 2003, 29, 456–460. [Google Scholar] [CrossRef] [PubMed]
- Boudreau, G.P.; Grosberg, B.M.; McAllister, P.J.; Lipton, R.B.; Buse, D.C. Prophylactic Onabotulinum toxina in Patients with Chronic Migraine and Comorbid Depression: An Open-Label, Multicenter, Pilot Study of Efficacy, Safety and Effect on Headache-Related Disability, Depression, and Anxiety. Int. J. Gen. Med. 2015, 8, 79–86. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Johnston, R.E.; Schallert, T.; Becker, J.B. Akinesia and Postural Abnormality after Unilateral Dopamine Depletion. Behav. Brain Res. 1999, 104, 189–196. [Google Scholar] [CrossRef]
- Schwarting, R.K.W.; Huston, J.P. The Unilateral 6-Hydroxydopamine Lesion Model in Behavioral Brain Research. Analysis of Functional Deficits, Recovery and Treatments. Prog. Neurobiol. 1996, 50, 275–331. [Google Scholar] [CrossRef]
- Ferro, M.M.; Bellissimo, M.I.; Anselmo-Franci, J.A.; Angellucci, M.E.M.; Canteras, N.S.; Da Cunha, C. Comparison of Bilaterally 6-OHDA—and MPTP—Lesioned Rats as Models of the Early Phase of Parkinson’s Disease: Histological, Neurochemical, Motor and Memory Alterations. J. Neurosci. Methods 2005, 148, 78–87. [Google Scholar] [CrossRef] [PubMed]
- Dauer, W.; Przedborski, S. Parkinson’s Disease: Mechanisms and Models. Neuron 2003, 39, 889–909. [Google Scholar] [CrossRef] [Green Version]
- Dujardin, K.; Sgambato, V. Neuropsychiatric Disorders in Parkinson’s Disease: What Do We Know about the Role of Dopaminergic and Non-dopaminergic Systems? Front. Neurosci. 2020, 14, 25. [Google Scholar] [CrossRef] [PubMed]
- Clement, Y.; Chapouthier, G. Biological Bases of Anxiety. Neurosci. Biobehav. Rev. 1998, 22, 623–633. [Google Scholar] [CrossRef]
- Walsh, R.N.; Cummins, R.A. The Open-Field Test: A Critical Review. Psychol. Bull. 1976, 83, 482–504. [Google Scholar] [CrossRef]
- Greggor, A.L.; Thornton, A.; Clayton, N.S. Neophobia Is Not only Avoidance: Improving Neophobia Tests by Combining Cognition and Ecology. Curr. Opin. Behav. Sci. 2015, 6, 82–89. [Google Scholar] [CrossRef] [Green Version]
- Perals, D.; Griffin, A.S.; Bartomeus, I.; Sol, D. Revisiting the Open-Field Test: What Does It Really Tell Us about Animal Personality? Anim. Behav. 2017, 123, 69–79. [Google Scholar] [CrossRef]
- Carter, A.J.; Feeney, W.E.; Marshall, H.H.; Cowlishaw, G.; Heinsohn, R. Animal personality: What are behavioural ecologists measuring? Biol. Rev. 2013, 88, 465–475. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Pellow, S.; Chopin, P.; File, S.E.; Briley, M. Validation of Open: Closed Arm Entries in an Elevated Plus-Maze as a Measure of Anxiety in the Rat. J. Neurosci. Methods 1985, 14, 149–167. [Google Scholar] [CrossRef]
- Hogg, S. A Review of the Validity and Variability of the Elevated Plus-Maze as an Animal Model of Anxiety. Pharmacol. Biochem. Behav. 1996, 54, 21–30. [Google Scholar] [CrossRef]
- Treit, D.; Menard, J.; Royan, C. Anxiogenic Stimuli in the Elevated Plus-Maze. Pharmacol. Biochem. Behav. 1993, 44, 463–469. [Google Scholar] [CrossRef]
- Lister, R.G. The Use of a Plus-Maze to Measure Anxiety in the Mouse. Psychopharmacology 1987, 92, 180–185. [Google Scholar] [CrossRef]
- Seibenhener, M.L.; Wooten, M.C. Use of the Open Field Maze to Measure Locomotor and Anxiety-Like Behavior in Mice. J. Vis. Exp. 2015. [Google Scholar] [CrossRef] [Green Version]
- Carola, V.; D’Olimpio, F.; Brunamonti, E.; Mangia, F.; Renzi, P. Evaluation of the Elevated Plus-Maze and Open-Field Tests for the Assessment of Anxiety-Related Behaviour in Inbred Mice. Behav. Brain Res. 2002, 134, 49–57. [Google Scholar] [CrossRef]
- Treit, D. Animal Models for the Study of Anti-Anxiety Agents: A Review. Neurosci. Biobehav. Rev. 1985, 9, 203–222. [Google Scholar] [CrossRef]
- Cole, J.C.; Rodgers, R.J. Ethological Comparison of the Effects of Diazepam and Acute/Chronic Imipramine on the Behaviour of Mice in the Elevated Plus-Maze. Pharmacol. Biochem. Behav. 1995, 52, 473–478. [Google Scholar] [CrossRef]
- Schmitt, U.; Hiemke, C. Combination of Open Field and Elevated Plus-Maze: A Suitable Test Battery to Assess Strain as Well as Treatment Differences in Rat Behavior. Prog. Neuro-Psychopharmacol. Biol. Psychiatry 1998, 22, 1197–1215. [Google Scholar] [CrossRef]
- Sun, T.; He, W.; Hu, G.; Li, M. Anxiolytic-Like Property of Risperidone and Olanzapine as Examined in Multiple Measures of Fear in Rats. Pharmacol. Biochem. Behav. 2010, 95, 298–307. [Google Scholar] [CrossRef] [Green Version]
- Belujon, P.; Bezard, E.; Taupignon, A.; Bioulac, B.; Benazzouz, A. Noradrenergic Modulation of Subthalamic Nucleus Activity: Behavioral and Electrophysiological Evidence in Intact and 6-Hydroxydopamine-Lesioned Rats. J. Neurosci. 2007, 27, 9595–9606. [Google Scholar] [CrossRef] [Green Version]
- Sun, Y.N.; Wang, T.; Wang, Y.; Han, L.N.; Li, L.B.; Zhang, Y.M.; Liu, J. Activation Of 5-HT1A Receptors in the Medial Subdivision of the Central Nucleus of the Amygdala Produces Anxiolytic Effects in a Rat Model of Parkinson’s Disease. Neuropharmacology 2015, 95, 181–191. [Google Scholar] [CrossRef] [PubMed]
- O’Connor, K.A.; Feustel, P.J.; Ramirez-Zamora, A.; Molho, E.; Pilitsis, J.G.; Shin, D.S. Investigation of Diazepam Efficacy on Anxiety-Like Behavior in Hemiparkinsonian Rats. Behav. Brain Res. 2016, 301, 226–237. [Google Scholar] [CrossRef]
- Sousa, N.; Almeida, O.F.X.; Wotjak, C.T. A Hitchhiker’s Guide to Behavioral Analysis in Laboratory Rodents. Genes Brain Behav. 2006, 5, 5–24. [Google Scholar] [CrossRef] [PubMed]
- Yankelevitch-Yahav, R.; Franko, M.; Huly, A.; Doron, R. The Forced Swim Test as a Model of Depressive-like Behavior. J. Vis. Exp. 2015. [Google Scholar] [CrossRef]
- Porsolt, R.D.; Le Pichon, M.; Jalfre, M. Depression: A new Animal Model Sensitive to Antidepressant Treatments. Nature 1977, 266, 730–732. [Google Scholar] [CrossRef] [PubMed]
- Petit-Demouliere, B.; Chenu, F.; Bourin, M. Forced swimming test in mice: A Review of Antidepressant Activity. Psychopharmacology 2005, 177, 245–255. [Google Scholar] [CrossRef]
- Detke, M.J.; Rickels, M.; Lucki, I. Active Behaviors in the Rat Forced Swimming Test Differentially Produced by Serotonergic and Noradrenergic Antidepressants. Psychopharmacology 1995, 121, 66–72. [Google Scholar] [CrossRef]
- Can, A.; Dao, D.T.; Arad, M.; Terrillion, C.E.; Piantadosi, S.C.; Gould, T.D. The Mouse Forced Swim Test. J. Vis. Exp. 2012, 59, e3638. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mezadri, T.J.; Batista, G.M.; Portes, A.C.; Marino-Neto, J.; Lino-de-Oliveira, C. Repeated Rat-Forced Swim Test: Reducing the Number of Animals to Evaluate Gradual Effects of Antidepressants. J. Neurosci. Methods 2011, 195, 200–205. [Google Scholar] [CrossRef] [Green Version]
- Lino-De-Oliveira, C.; De Lima, T.C.M.; Carobrez, A.D.P. Structure of the Rat Behaviour in The Forced Swimming Test. Behav. Brain Res. 2005, 158, 243–250. [Google Scholar] [CrossRef]
- Vieira, C.; De Lima, T.C.M.; de Carobrez, A.P.; Lino-de-Oliveira, C. Frequency of Climbing Behavior as a Predictor of Altered Motor Activity in Rat Forced Swimming Test. Neurosci. Lett. 2008, 445, 170–173. [Google Scholar] [CrossRef] [PubMed]
- Schintu, N.; Zhang, X.; Svenningsson, P. Studies of Depression-Related States in Animal Models of Parkinsonism. J. Parkinson’s Dis. 2012, 2, 87–106. [Google Scholar] [CrossRef] [Green Version]
- Vecchia, D.D.; Kanazawa, L.K.S.; Wendler, E.; de Hocayen, P.A.S.; Vital, M.A.B.F.; Takahashi, R.N.; Da Cunha, C.; Miyoshi, E.; Andreatini, R. Ketamine Reversed Short-Term Memory Impairment and Depressive-Like Behavior in Animal Model of Parkinson’s Disease. Brain Res. Bull. 2021, 168, 63–73. [Google Scholar] [CrossRef]
- Overstreet, D.H. Modeling Depression in Animal Models. Methods Mol. Biol. 2012, 829, 125–144. [Google Scholar] [CrossRef]
- Porsolt, R.D.; Brossard, G.; Hautbois, C.; Roux, S. Rodent Models of Depression: Forced Swimming And Tail Suspension Behavioral Despair Tests in Rats And Mice. Curr. Protoc. Neurosci. 2001. [Google Scholar] [CrossRef]
- Doron, R.; Lotan, D.; Einat, N.; Yaffe, R.; Winer, A.; Marom, I.; Meron, G.; Kately, N.; Rehavi, M. A Novel Herbal Treatment Reduces Depressive-Like Behaviors and Increases BDNF Levels in the Brain of Stressed Mice. Life Sci. 2014, 94, 151–157. [Google Scholar] [CrossRef]
- Caspi, A.; Sugden, K.; Moffitt, T.E.; Taylor, A.; Craig, I.W.; Harrington, H.L.; McClay, J.; Mill, J.; Martin, J.; Braithwaite, A.; et al. Influence of life stress on depression: Moderation by a polymorphism in the 5-HTT gene. Science 2003, 301, 386–389. [Google Scholar] [CrossRef]
- Kaufman, J.; Yang, B.Z.; Douglas-Palumberi, H.; Grasso, D.; Lipschitz, D.; Houshyar, S.; Krystal, J.H.; Gelernter, J. Brain-Derived Neurotrophic Factor-5-HTTLPR Gene Interactions and Environmental Modifiers of Depression in Children. Biol. Psychiatry 2006, 59, 673–680. [Google Scholar] [CrossRef]
- Cryan, J.F.; Valentino, R.J.; Lucki, I. Assessing Substrates Underlying the Behavioral Effects of Antidepressants Using the Modified Rat Forced Swimming Test. Neurosci. Biobehav. Rev. 2005, 29, 547–569. [Google Scholar] [CrossRef]
- Rénéric, J.P.; Bouvard, M.; Stinus, L. In the Rat Forced Swimming Test, Chronic but Not Subacute Administration of Dual 5-HT/NA Antidepressant Treatments May Produce Greater Effects than Selective Drugs. Behav. Brain Res. 2002, 136, 521–532. [Google Scholar] [CrossRef]
- López-Rubalcava, C.; Lucki, I. Strain Differences in the Behavioral Effects of Antidepressant Drugs in the Rat Forced Swimming Test. Neuropsychopharmacology 2000, 22, 191–199. [Google Scholar] [CrossRef]
- Anisman, H.; Zacharko, R.M. Multiple Neurochemical and Behavioral Consequences of Stressors: Implications for Depression. Pharmacol. Ther. 1990, 46, 119–136. [Google Scholar] [CrossRef]
- Kessler, R.C. The Effects of Stressful Life Events on Depression. Annu. Rev. Psychol. 1997, 48, 191–214. [Google Scholar] [CrossRef] [PubMed]
- Sullivan, P.F.; Neale, M.C.; Kendler, K.S. Genetic Epidemiology of Major Depression: Review and Meta-Analysis. Am. J. Psychiatry 2000, 157, 1552–1562. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Q.J.; Du, C.X.; Tan, H.H.; Zhang, L.; Li, L.B.; Zhang, J.; Niu, X.L.; Liu, J. Activation and Blockade of Serotonin7 Receptors in the Prelimbic Cortex Regulate Depressive-Like Behaviors in A 6-Hydroxydopamine-Induced Parkinson’s Disease Rat Model. Neuroscience 2015, 311, 45–55. [Google Scholar] [CrossRef] [PubMed]
- Lian, T.H.; Guo, P.; Zuo, L.J.; Hu, Y.; Yu, S.Y.; Liu, L.; Jin, Z.; Yu, Q.J.; Wang, R.D.; Li, L.X.; et al. An Investigation on the Clinical Features and Neurochemical Changes in Parkinson’s Disease with Depression. Front. Psychiatry 2019, 10. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Fontoura, J.L.; Baptista, C.; de Pedroso, F.B.; Pochapski, J.A.; Miyoshi, E.; Ferro, M.M. Depression in Parkinson’s Disease: The Contribution from Animal Studies. Parkinsons. Dis. 2017, 2017, 9124160. [Google Scholar] [CrossRef] [Green Version]
- Kano, O.; Ikeda, K.; Cridebring, D.; Takazawa, T.; Yoshii, Y.; Iwasaki, Y. Neurobiology of Depression and Anxiety In Parkinson’s Disease. Parkinson’s Dis. 2011, 2011. [Google Scholar] [CrossRef] [Green Version]
- Shin, E.; Rogers, J.T.; Devoto, P.; Björklund, A.; Carta, M. Noradrenaline Neuron Degeneration Contributes to Motor Impairments and Development of L-DOPA-Induced Dyskinesia in a Rat Model of Parkinson’s Disease. Exp. Neurol. 2014, 257, 25–38. [Google Scholar] [CrossRef]
- Leentjens, A.F.G.; Moonen, A.J.H.; Dujardin, K.; Marsh, L.; Martinez-Martin, P.; Richard, I.H.; Starkstein, S.E.; Köhler, S. Modeling Depression in Parkinson Disease: Disease-Specific and Nonspecific Risk Factors. Neurology 2013, 81, 1036–1043. [Google Scholar] [CrossRef] [Green Version]
- Gallagher, D.A.; Schrag, A. Psychosis, Apathy, Depression and Anxiety in Parkinson’s Disease. Neurobiol. Dis. 2012, 46, 581–589. [Google Scholar] [CrossRef]
- Remy, P.; Doder, M.; Lees, A.; Turjanski, N.; Brooks, D. Depression in Parkinson’s Disease: Loss of Dopamine and Noradrenaline Innervation in the Limbic System. Brain 2005, 128, 1314–1322. [Google Scholar] [CrossRef] [Green Version]
- Shinotoh, H.; Inoue, O.; Hirayama, K.; Aotsuka, A.; Asahina, M.; Suhara, T.; Yamazaki, T.; Tateno, Y. Dopamine D 1 Receptors in Parkinson’s Disease and Striatonigral Degeneration: A Positron Emission Tomography Study. J. Neurol. Neurosurg. Psychiatry 1993, 56, 467–472. [Google Scholar] [CrossRef]
- Corvol, J.C.; Muriel, M.P.; Valjent, E.; Féger, J.; Hanoun, N.; Girault, J.A.; Hirsch, E.C.; Hervé, D. Persistent Increase in Olfactory Type G-Protein a Subunit Levels May Underlie D1 Receptor Functional Hypersensitivity in Parkinson Disease. J. Neurosci. 2004, 24, 7007–7014. [Google Scholar] [CrossRef] [Green Version]
- Turjanski, N.; Lees, A.J.; Brooks, D.J. In Vivo Studies on Striatal Dopamine D1 and D2 Site Binding in L-Dopa-Treated Parkinson’s Disease Patients with and Without Dyskinesias. Neurology 1997, 49, 717–723. [Google Scholar] [CrossRef]
- Hurley, M.J.; Mash, D.C.; Jenner, P. Dopamine D1 Receptor Expression in Human Basal Ganglia and Changes in Parkinson’s Disease. Mol. Brain Res. 2001, 87, 271–279. [Google Scholar] [CrossRef]
- Wenning, G.K.; Donnemiller, E.; Granata, R.; Riccabona, G.; Poewe, W. 123I-β-CIT and 123I-IBZM-SPECT Scanning in Levodopa-Naive Parkinson’s Disease. Mov. Disord. 1998, 13, 438–445. [Google Scholar] [CrossRef]
- Ichise, M.; Kim, Y.J.; Ballinger, J.R.; Vines, D.; Erami, S.S.; Tanaka, F.; Lang, A.E. SPECT Imaging of Pre- and Postsynaptic Dopaminergic Alterations in L- Dopa-Untreated PD. Neurology 1999, 52, 1206–1214. [Google Scholar] [CrossRef] [PubMed]
- Waeber, C.; Rigo, M.; Chinaglia, G.; Probst, A.; Palacios, J.M. Beta-Adrenergic Receptor Subtypes in the Basal Ganglia of Patients with Huntington’s Chorea and Parkinson’s Disease. Synapse 1991, 8, 270–280. [Google Scholar] [CrossRef] [PubMed]
- Maloteaux, J.M.; Laterre, E.C.; Laduron, P.M.; Javoy-Agid, F.; Agid, Y. Decrease of serotonin-S2 receptors in temporal cortex of patients with Parkinson’s disease and progressive supranuclear palsy. Mov. Disord. 1988, 3, 255–262. [Google Scholar] [CrossRef] [PubMed]
- Kish, S.J.; Tong, J.; Hornykiewicz, O.; Rajput, A.; Chang, L.J.; Guttman, M.; Furukawa, Y. Preferential Loss of Serotonin Markers in Caudate Versus Putamen in Parkinson’s Disease. Brain 2008, 131, 120–131. [Google Scholar] [CrossRef]
- Aubert, I.; Araujo, D.M.; Cécyre, D.; Robitaille, Y.; Gauthier, S.; Quirion, R. Comparative Alterations of Nicotinic and Muscarinic Binding Sites in Alzheimer’s and Parkinson’s Diseases. J. Neurochem. 1992, 58, 529–541. [Google Scholar] [CrossRef] [PubMed]
- Lange, K.W.; Wells, F.R.; Jenner, P.; Marsden, C.D. Altered Muscarinic and Nicotinic Receptor Densities in Cortical and Subcortical Brain Regions in Parkinson’s Disease. J. Neurochem. 1993, 60, 197–203. [Google Scholar] [CrossRef]
- McOmish, C.; Pavey, G.; McLean, C.; Horne, M.; Dean, B.; Scarr, E. Muscarinic Receptor Binding Changes in Postmortem Parkinson’s Disease. J. Neural Transm. 2017, 124, 227–236. [Google Scholar] [CrossRef] [PubMed]
- Meyer, P.M.; Strecker, K.; Kendziorra, K.; Becker, G.; Hesse, S.; Woelpl, D.; Hensel, A.; Patt, M.; Sorger, D.; Wegner, F.; et al. Reduced α4β2*-Nicotinic Acetylcholine Receptor Binding and Its Relationship to Mild Cognitive and Depressive Symptoms in Parkinson Disease. Arch. Gen. Psychiatry 2009, 66, 866–877. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mann, T.; Zilles, K.; Dikow, H.; Hellfritsch, A.; Cremer, M.; Piel, M.; Rösch, F.; Hawlitschka, A.; Schmitt, O.; Wree, A. Dopamine, Noradrenaline and Serotonin Receptor Densities in the Striatum of Hemiparkinsonian Rats Following Botulinum Neurotoxin-A Injection. Neuroscience 2018, 374, 187–204. [Google Scholar] [CrossRef] [PubMed]
- Creese, I.; Snyder, S.H. Nigrostriatal Lesions Enhance Striatal 3H-Apomorphine and 3H-Spiroperidol Binding. Eur. J. Pharmacol. 1979, 56, 277–281. [Google Scholar] [CrossRef]
- Creese, I.; Burt, D.R.; Snyder, S.H. Dopamine Receptor Binding Enhancement Accompanies Lesion-Induced Behavioral Supersensitivity. Science 1977, 197, 596–598. [Google Scholar] [CrossRef] [PubMed]
- Lucking, C.B.; Kosel, S.; Mehraein, P.; Graeber, M.B. Absence of the Mitochondrial A7237T Mutation in Parkinson’s Disease. Biochem. Biophys. Res. Commun. 1995, 211, 700–704. [Google Scholar] [CrossRef] [PubMed]
- Savasta, M.; Dubois, A.; Feuerstein, C.; Manier, M.; Scatton, B. Denervation Supersensitivity of Striatal D2 Dopamine Receptors Is Restricted to the Ventro—And Dorsolateral Regions of the Striatum. Neurosci. Lett. 1987, 74, 180–186. [Google Scholar] [CrossRef]
- Graham, W.C.; Clarke, C.E.; Boyce, S.; Sambrook, M.A.; Crossman, A.R.; Woodruff, G.N. Autoradiographic Studies in Animal Models of Hemi-Parkinsonism Reveal Dopamine D2 But Not D1 Receptor Supersensitivity. II. Unilateral Intra-Carotid Infusion of MPTP in the Monkey (Macaca fascicularis). Brain Res. 1990, 514, 103–110. [Google Scholar] [CrossRef]
- Chritin, M.; Savasta, M.; Mennicken, F.; Bal, A.; Abrous, D.N.; Le Moal, M.; Feuerstein, C.; Herman, J.P. Intrastriatal Dopamine-rich Implants Reverse the Increase of Dopamine D2 Receptor mRNA Levels Caused by Lesion of the Nigrostriatal Pathway: A Quantitative In Situ Hybridization Study. Eur. J. Neurosci. 1992, 4, 663–672. [Google Scholar] [CrossRef] [PubMed]
- Fornaretto, M.G.; Caccia, C.; Caron, M.G.; Fariello, R.G. Dopamine Receptors Status After Unilateral Nigral 6-OHDA Lesion—Autoradiographic And In Situ Hybridization Study in the Rat Brain. Mol. Chem. Neuropathol. 1993, 19, 147–162. [Google Scholar] [CrossRef]
- Narang, N.; Wamsley, J.K. Time Dependent Changes in DA Uptake Sites, D1 and D2 Receptor Binding and Mrna After 6-OHDA Lesions of the Medial Forebrain Bundle in the Rat Brain. J. Chem. Neuroanat. 1995, 9, 41–53. [Google Scholar] [CrossRef]
- Lawler, C.P.; Gilmore, J.H.; Watts, V.J.; Walker, Q.D.; Southerland, S.B.; Cook, L.L.; Mathis, C.A.; Mailman, R.B. Interhemispheric Modulation of Dopamine Receptor Interactions in Unilateral 6-OHDA Rodent Model. Synapse 1995, 21, 299–311. [Google Scholar] [CrossRef] [PubMed]
- Ryu, J.H.; Yanai, K.; Zhao, X.L.; Watanabe, T. The Effect of Dopamine D1 Receptor Stimulation on the Up-Regulation of Histamine H3-Receptors Following Destruction of the Ascending Dopaminergic Neurones. Br. J. Pharmacol. 1996, 118, 585–592. [Google Scholar] [CrossRef] [Green Version]
- Araki, T.; Tanji, H.; Fujihara, K.; Kato, H.; Imai, Y.; Mizugaki, M.; Itoyama, Y. Sequential Changes of Cholinergic and Dopaminergic Receptors in Brains After 6-Hydroxydopamine Lesions of the Medial Forebrain Bundle in Rats. J. Neural Transm. 2000, 107, 873–884. [Google Scholar] [CrossRef]
- Xu, Z.C.; Ling, G.; Sahr, R.N.; Neal-Beliveau, B.S. Asymmetrical Changes of Dopamine Receptors in the Striatum After Unilateral Dopamine Depletion. Brain Res. 2005, 1038, 163–170. [Google Scholar] [CrossRef] [PubMed]
- Mann, T.; Zilles, K.; Klawitter, F.; Cremer, M.; Hawlitschka, A.; Palomero-Gallagher, N.; Schmitt, O.; Wree, A. Acetylcholine Neurotransmitter Receptor Densities in the Striatum of Hemiparkinsonian Rats Following Botulinum Neurotoxin-A Injection. Front. Neuroanat. 2018, 12, 65. [Google Scholar] [CrossRef]
- Ho, Y.J.; Eichendorff, J.; Schwarting, R.K.W. Individual Response Profiles of Male Wistar Rats in Animal Models for Anxiety and Depression. Behav. Brain Res. 2002, 136, 1–12. [Google Scholar] [CrossRef]
- Estanislau, C.; Ramos, A.C.; Ferraresi, P.D.; Costa, N.F.; de Carvalho, H.M.C.P.; Batistela, S. Individual Differences in the Elevated Plus-Maze and the Forced Swim Test. Behav. Processes 2011, 86, 46–51. [Google Scholar] [CrossRef]
- Anyan, J.; Amir, S. Too Depressed to Swim or Too Afraid to Stop? A Reinterpretation of the Forced Swim Test as a Measure of Anxiety-Like Behavior. Neuropsychopharmacology 2018, 43, 931–933. [Google Scholar] [CrossRef]
- Lamers, F.; Van Oppen, P.; Comijs, H.C.; Smit, J.H.; Spinhoven, P.; Van Balkom, A.J.L.M.; Nolen, W.A.; Zitman, F.G.; Beekman, A.T.F.; Penninx, B.W.J.H. Comorbidity Patterns of Anxiety and Depressive Disorders in A Large Cohort Study: The Netherlands Study of Depression and Anxiety (NESDA). J. Clin. Psychiatry 2011, 72, 342–348. [Google Scholar] [CrossRef]
- Huber, S.J.; Paulson, G.W.; Shuttleworth, E.C. Relationship of Motor Symptoms, Intellectual Impairment, and Depression in Parkinson’s Disease. J. Neurol. Neurosurg. Psychiatry 1988, 51, 855–858. [Google Scholar] [CrossRef] [Green Version]
- Mondolo, F.; Jahanshahi, M.; Granà, A.; Biasutti, E.; Cacciatori, E.; Benedetto, P. Evaluation of Anxiety in Parkinson’s Disease with Some Commonly Used Rating Scales. Neurol. Sci. 2007, 28, 270–275. [Google Scholar] [CrossRef]
- Santangelo, G.; Vitale, C.; Trojano, L.; Longo, K.; Cozzolino, A.; Grossi, D.; Barone, P. Relationship between Depression and Cognitive Dysfunctions in Parkinson’s Disease without Dementia. J. Neurol. 2009, 256, 632–638. [Google Scholar] [CrossRef]
- Witt, K.; Daniels, C.; Herzog, J.; Lorenz, D.; Volkmann, J.; Reiff, J.; Mehdorn, M.; Deuschl, G.; Krack, P. Differential Effects of L-Dopa and Subthalamic Stimulation on Depressive Symptoms and Hedonic Tone in Parkinson’s Disease. J. Neuropsychiatry Clin. Neurosci. 2006, 18, 397–401. [Google Scholar] [CrossRef] [PubMed]
- Kostić, V.S.; Djuričić, B.M.; Čovičković-Šternić, N.; Bumbaširević, L.; Nikolić, M.; Mršulja, B.B. Depression and Parkinson’s Disease: Possible Role of Serotonergic Mechanisms. J. Neurol. 1987, 234, 94–96. [Google Scholar] [CrossRef]
- Marsh, G.G.; Markham, C.H. Does Levodopa Alter Depression and Psychopathology in Parkinsonism Patients? J. Neurol. Neurosurg. Psychiatry 1973, 36, 925–935. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wang, G.; Hong, Z.; Cheng, Q.; Xiao, Q.; Wang, Y.; Zhang, J.; Ma, J.F.; Wang, X.J.; Zhou, H.Y. Validation of the Chinese Non-Motor Symptoms Scale for Parkinson’s disease: Results from a Chinese pilot study. Clin. Neurol. Neurosurg. 2009, 111, 523–526. [Google Scholar] [CrossRef] [PubMed]
- Malberg, J.E.; Eisch, A.J.; Nestler, E.J.; Duman, R.S. Chronic antidepressant treatment increases neurogenesis in adult rat hippocampus. J. Neurosci. 2000, 20, 9104–9110. [Google Scholar] [CrossRef] [PubMed]
- Sahay, A.; Hen, R. Adult hippocampal neurogenesis in depression. Nat. Neurosci. 2007, 10, 1110–1115. [Google Scholar] [CrossRef] [PubMed]
- Antonucci, F.; Bozzi, Y.; Caleo, M. Intrahippocampal infusion of botulinum neurotoxin e (BoNT/E) reduces spontaneous recurrent seizures in a mouse model of mesial temporal lobe epilepsy. Epilepsia 2009, 50, 963–966. [Google Scholar] [CrossRef] [PubMed]
- Gasior, M.; Tang, R.; Rogawski, M.A. Long-lasting attenuation of amygdala-kindled seizures after convection-enhanced delivery of botulinum neurotoxins a and B into the amygdala in rats. J. Pharmacol. Exp. Ther. 2013, 346, 528–534. [Google Scholar] [CrossRef] [Green Version]
- Paxinos, G.; Watson, C. The Rat Brain in Stereotaxic Coordinates, 7th ed.; Elsevier/Academic Press: Amsterdam, The Netherlands; London, UK, 2015; ISBN 9780123919496. [Google Scholar]
- Schwarting, R.K.W.W.; Huston, J.P. Unilateral 6-hydroxydopamine lesions of meso-striatal dopamine neurons and their physiological sequelae. Prog. Neurobiol. 1996, 49, 215–266. [Google Scholar] [CrossRef]
- Ungerstedt, U.; Arbuthnott, G.W. Quantitative recording of rotational behavior in rats after 6-hydroxy-dopamine lesions of the nigrostriatal dopamine system. Brain Res. 1970, 24, 485–493. [Google Scholar] [CrossRef]
- Emerich, D.F.; Lindner, M.D.; Winn, S.R.; Chen, E.Y.; Frydel, B.R.; Kordower, J.H. Implants of encapsulated human CNTF-producing fibroblasts prevent behavioral deficits and striatal degeneration in a rodent model of Huntington’s disease. J. Neurosci. 1996, 16, 5168–5181. [Google Scholar] [CrossRef]
- Nikkhah, G.; Bentlage, C.; Cunningham, M.G.; Björklund, A. Intranigral fetal dopamine grafts induce behavioral compensation in the rat Parkinson model. J. Neurosci. 1994, 14, 3449–3461. [Google Scholar] [CrossRef]
- Dunnett, S.B.; Torres, E.M. Rotation in the 6-OHDA-lesioned rat. Neuromethods 2011, 61, 299–315. [Google Scholar] [CrossRef]
- Ungerstedt, U. Striatal Dopamine Release after Amphetamine or Nerve Degeneration Revealed by Rotational Behaviour. Acta Physiol. Scand. 1971, 82, 49–68. [Google Scholar] [CrossRef]
- Björklund, A.; Dunnett, S.B. The amphetamine induced rotation test: A re-assessment of its use as a tool to monitor motor impairment and functional recovery in rodent models of Parkinson’s disease. J. Parkinson’s Dis. 2019, 9, 17–29. [Google Scholar] [CrossRef] [Green Version]
- Hudson, J.L.; van Horne, C.G.; Strömberg, I.; Brock, S.; Clayton, J.; Masserano, J.; Hoffer, B.J.; Gerhardt, G.A. Correlation of apomorphine- and amphetamine-induced turning with nigrostriatal dopamine content in unilateral 6-hydroxydopamine lesioned rats. Brain Res. 1993, 626, 167–174. [Google Scholar] [CrossRef]
- Hefti, F.; Melamed, E.; Sahakian, B.J.; Wurtman, R.J. Circling behavior in rats with partial, unilateral nigro-striatal lesions: Effect of amphetamine, apomorphine, and DOPA. Pharmacol. Biochem. Behav. 1980, 12, 185–188. [Google Scholar] [CrossRef]
- Hall, C. Emotional behavior in the rat. I. Defecation and urination as measures of individual differences in emotionality. J. Comp. Psychol. 1934, 18, 385–403. [Google Scholar] [CrossRef]
- DeFries, J.C.; Hegmann, J.P.; Weir, M.W. Open-field behavior in mice: Evidence for a major gene effect mediated by the visual system. Science 1966, 154, 1577–1579. [Google Scholar] [CrossRef]
- Eikelis, N.; Van Den Buuse, M. Cardiovascular responses to open-field stress in rats: Sex differences and effects of gonadal hormones. Stress 2000, 3, 319–334. [Google Scholar] [CrossRef] [PubMed]
- Andringa, G.; Van Oosten, R.V.; Unger, W.; Hafmans, T.G.M.; Veening, J.; Stoof, J.C.; Cools, A.R. Systemic administration of the propargylamine CGP 3466B prevents behavioural and morphological deficits in rats with 6-hydroxydopamine-induced lesions in the substantia nigra. Eur. J. Neurosci. 2000, 12, 3033–3043. [Google Scholar] [CrossRef]
- Denenberg, V.H. Open-field bheavior in the rat: What does it mean? Ann. N. Y. Acad. Sci. 1969, 159, 852–859. [Google Scholar] [CrossRef] [PubMed]
- Da Silva, T.P.; Poli, A.; Hara, D.B.; Takahashi, R.N. Time course study of microglial and behavioral alterations induced by 6-hydroxydopamine in rats. Neurosci. Lett. 2016, 622, 83–87. [Google Scholar] [CrossRef]
- Lucki, I. The forced swimming test as a model for core and component behavioral effects of antidepressant drugs. Behav. Pharmacol. 1997, 8, 523–532. [Google Scholar] [CrossRef]
- Deak, T.; Bellamy, C.; D’Agostino, L.G.; Rosanoff, M.; McElderry, N.K.; Bordner, K.A. Behavioral responses during the forced swim test are not affected by anti-inflammatory agents or acute illness induced by lipopolysaccharide. Behav. Brain Res. 2005, 160, 125–134. [Google Scholar] [CrossRef]
- Willner, P. The validity of animal models of depression. Psychopharmacology 1984, 83, 1–16. [Google Scholar] [CrossRef]
- Gregus, A.; Wintink, A.J.; Davis, A.C.; Kalynchuk, L.E. Effect of repeated corticosterone injections and restraint stress on anxiety and depression-like behavior in male rats. Behav. Brain Res. 2005, 156, 105–114. [Google Scholar] [CrossRef] [PubMed]
- Armario, A.; Gavaldà, A.; Martí, O. Forced swimming test in rats: Effect of desipramine administration and the period of exposure to the test on struggling behavior, swimming, immobility and defecation rate. Eur. J. Pharmacol. 1988, 158, 207–212. [Google Scholar] [CrossRef]
- Can, A.; Dao, D.T.; Terrillion, C.E.; Piantadosi, S.C.; Bhat, S.; Gould, T.D. The tail suspension test. J. Vis. Exp. 2012, 59, 3769. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mitchell, N.C.; Gould, G.G.; Smolik, C.M.; Koek, W.; Daws, L.C. Antidepressant-like drug effects in juvenile and adolescent mice in the tail suspension test: Relationship with hippocampal serotonin and norepinephrine transporter expression and function. Front. Pharmacol. 2013, 4, 131. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Huwiler, A. Tail suspension test. In Drug Discovery and Evaluation: Pharmacological Assays; Vogel, H., Ed.; Springer: Berlin/Heidelberg, Germany, 2008; pp. 791–793. [Google Scholar]
- Shinde, V.; Yegnanarayan, R.; Shah, P.; Gupta, A.; Pophale, P. Antidepressant-like activity of flunarizine in modified tail suspension test in rats. N. Am. J. Med. Sci. 2015, 7, 100–103. [Google Scholar] [CrossRef] [Green Version]
- Chermat, R.; Thierry, B.; Mico, J.A.; Steru, L.; Simon, P. Adaptation of the tail suspension test to the rat. J. Pharmacol. 1986, 17, 348–350. [Google Scholar]
- Paumier, K.L.; Sortwell, C.E.; Madhavan, L.; Terpstra, B.; Celano, S.L.; Green, J.J.; Imus, N.M.; Marckini, N.; Daley, B.; Steece-Collier, K.; et al. Chronic amitriptyline treatment attenuates nigrostriatal degeneration and significantly alters trophic support in a rat model of parkinsonism. Neuropsychopharmacology 2015, 40, 874–883. [Google Scholar] [CrossRef] [Green Version]
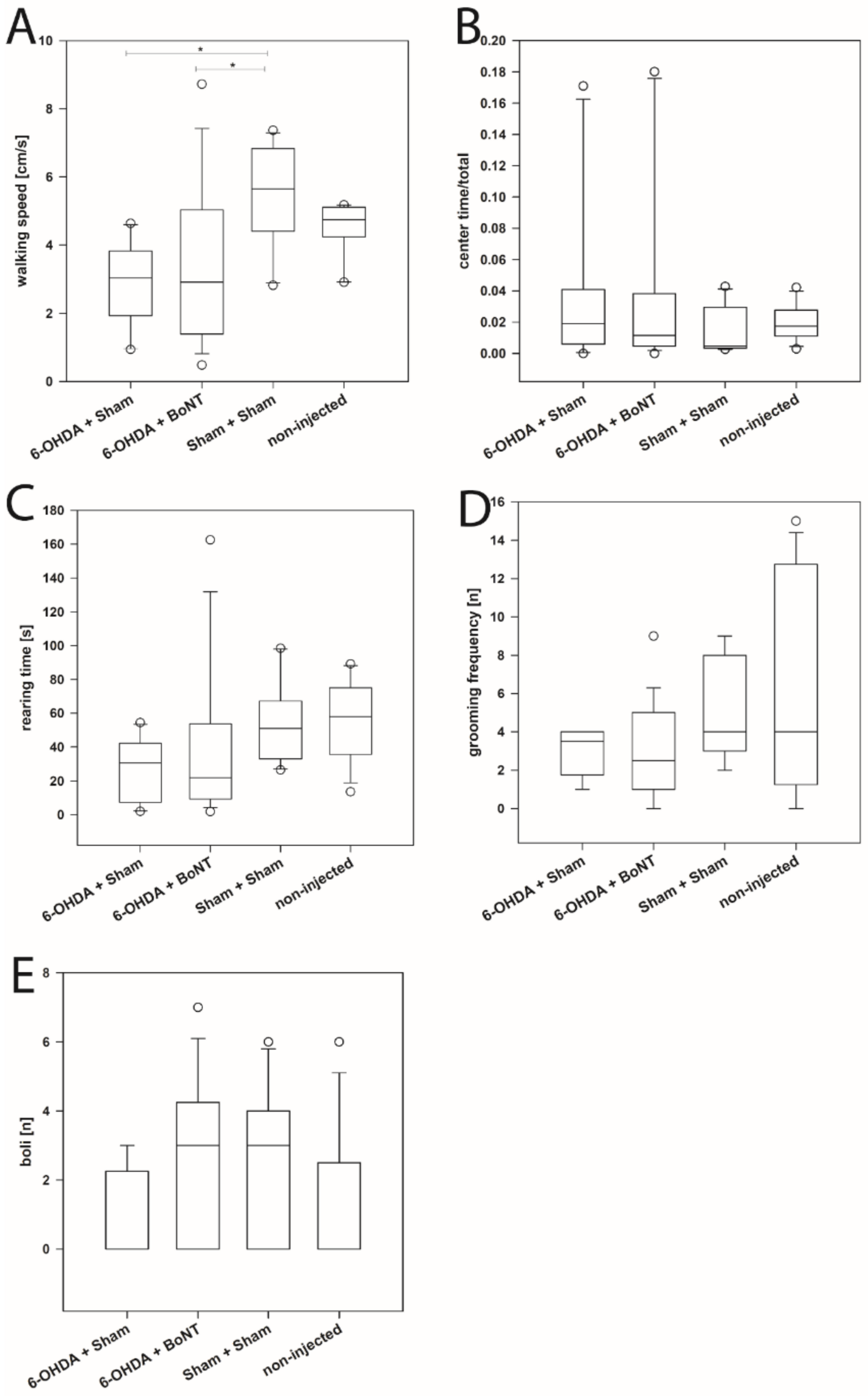



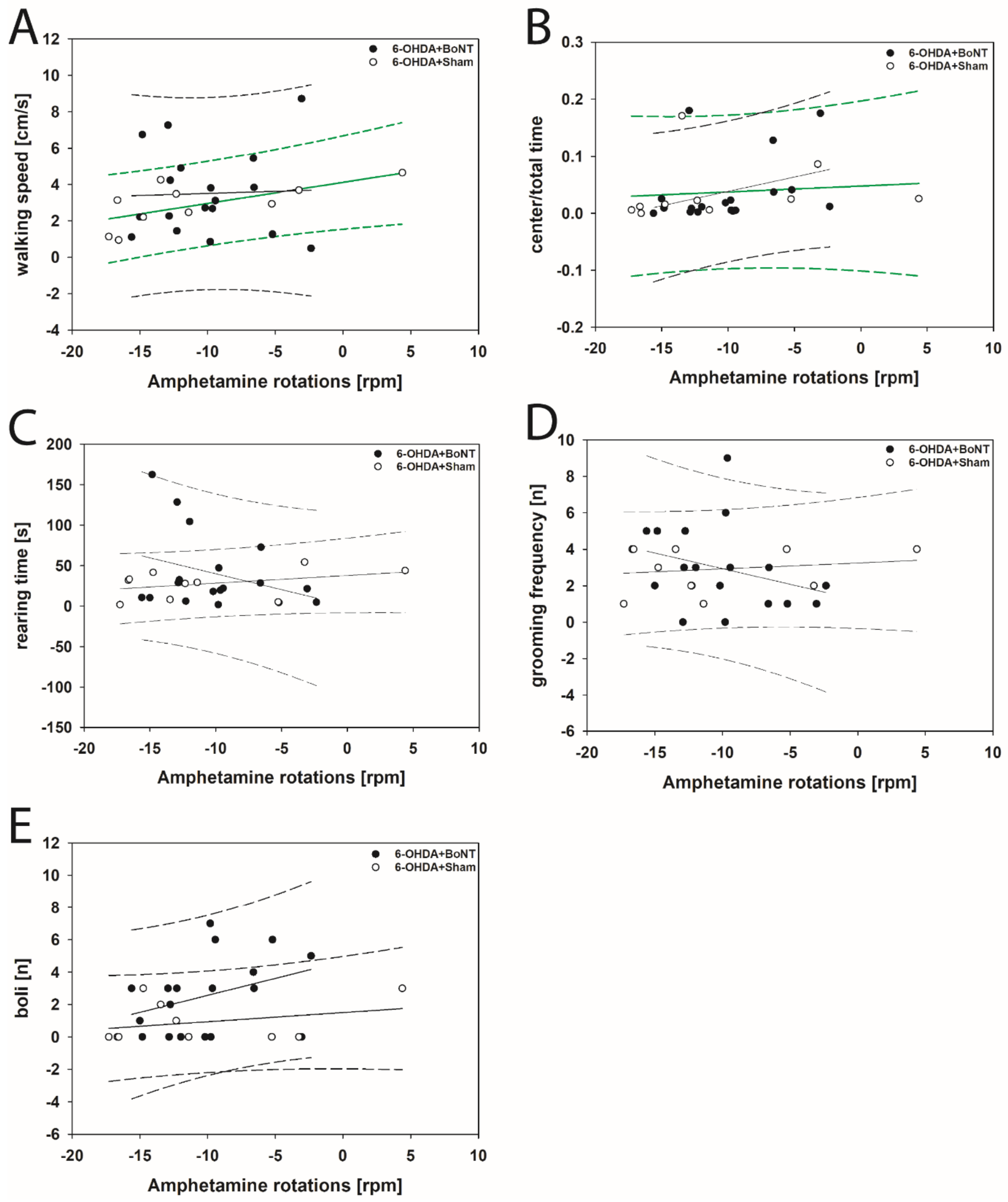

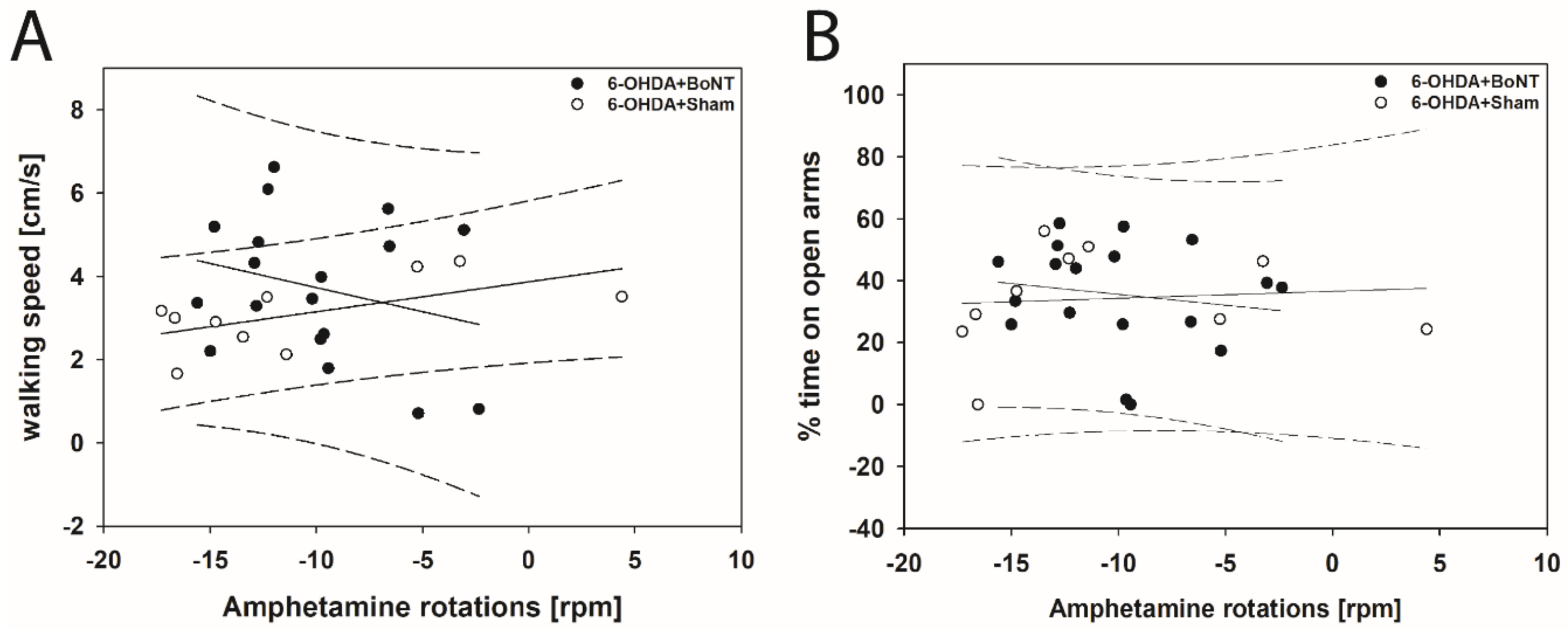
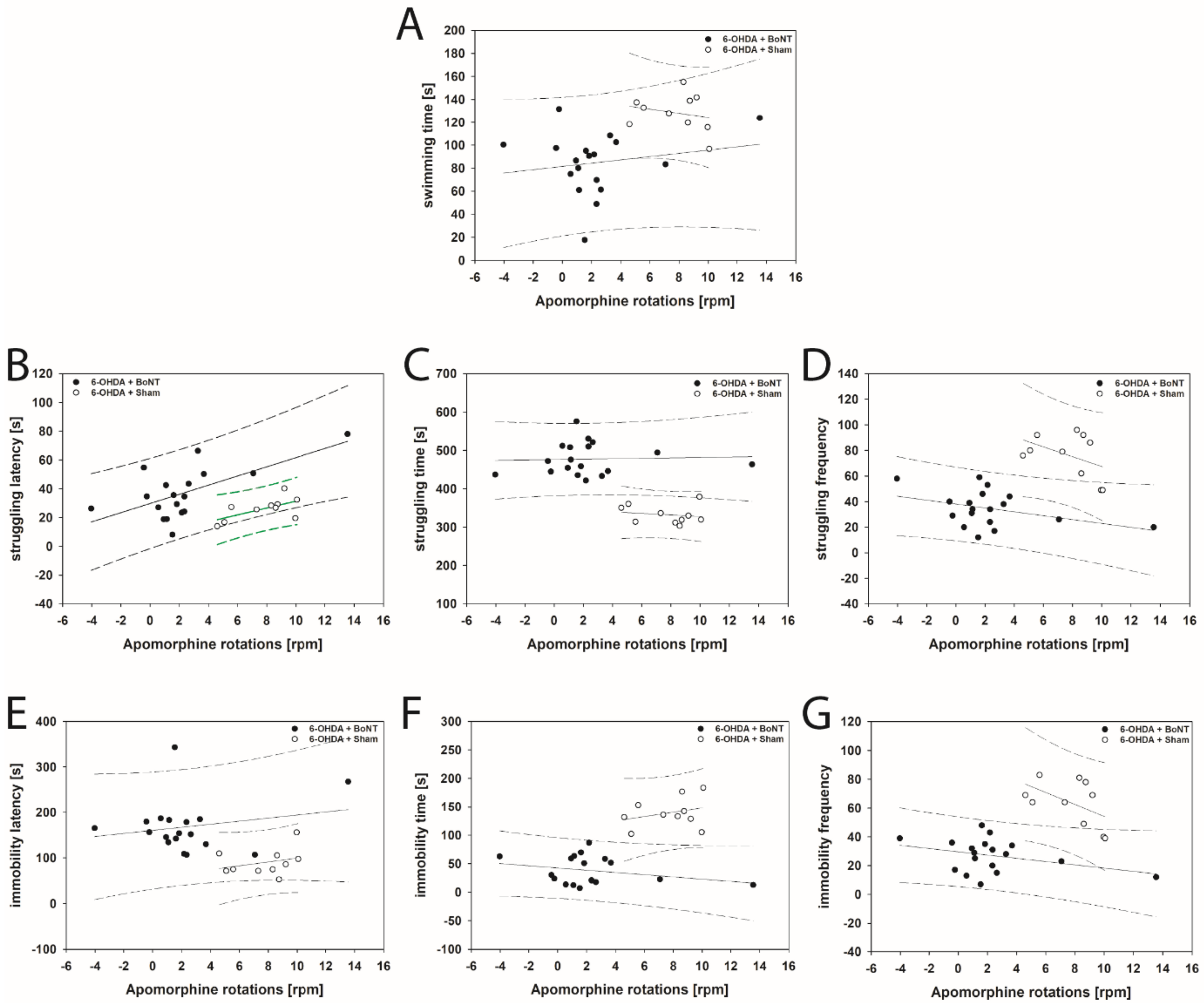
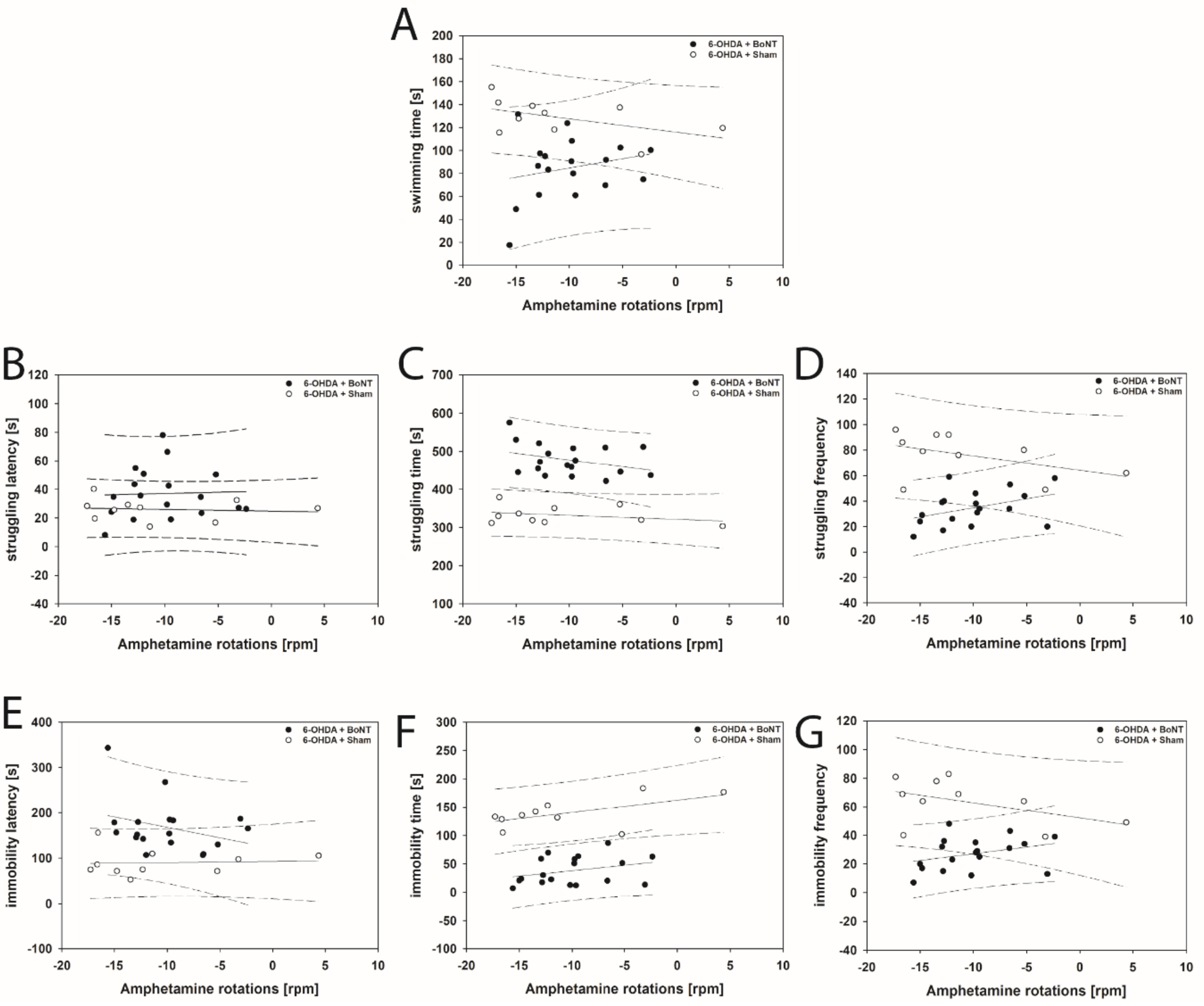
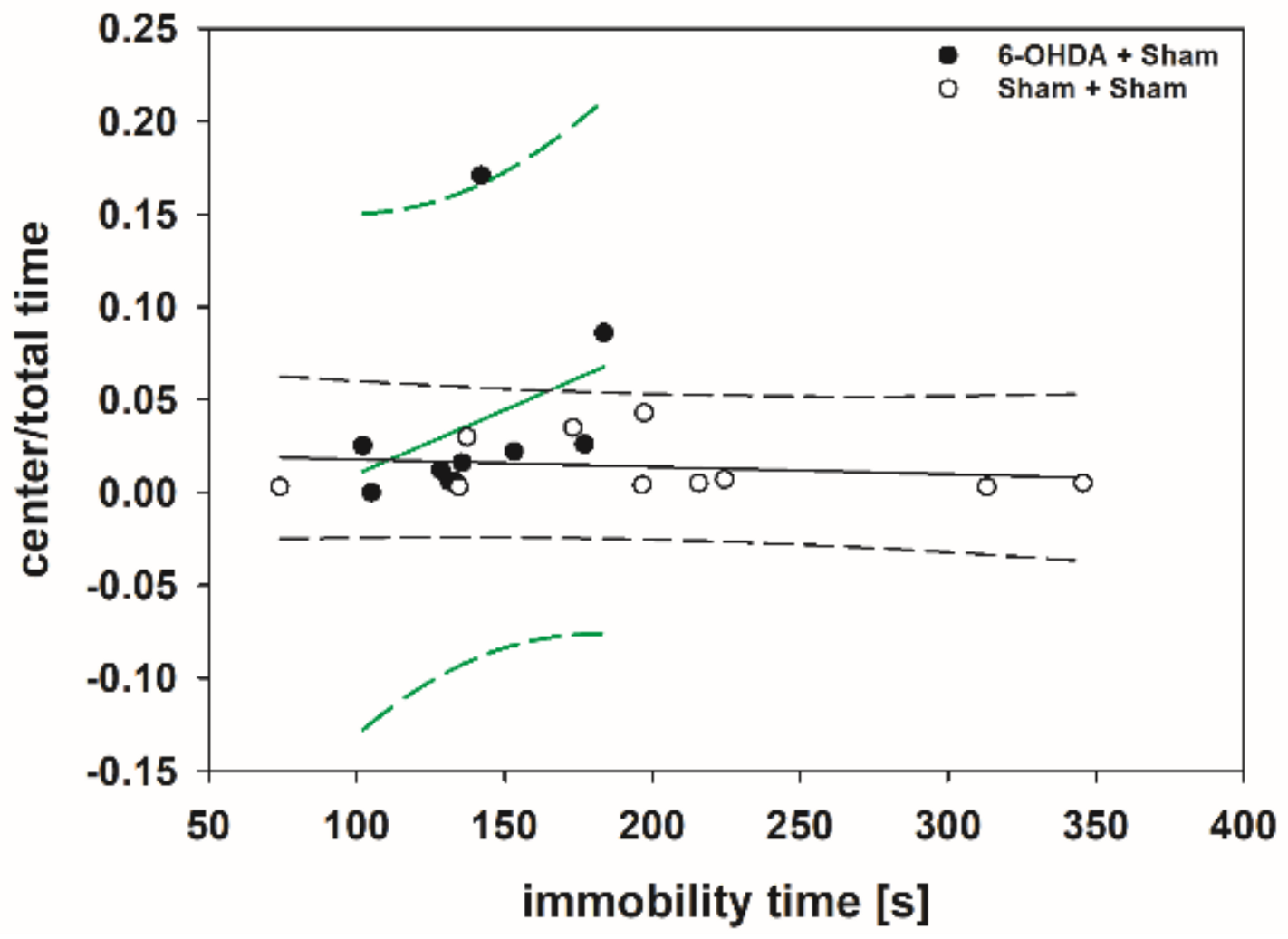

Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Antipova, V.; Holzmann, C.; Hawlitschka, A.; Witt, M.; Wree, A. Antidepressant-Like Properties of Intrastriatal Botulinum Neurotoxin-A Injection in a Unilateral 6-OHDA Rat Model of Parkinson’s Disease. Toxins 2021, 13, 505. https://0-doi-org.brum.beds.ac.uk/10.3390/toxins13070505
Antipova V, Holzmann C, Hawlitschka A, Witt M, Wree A. Antidepressant-Like Properties of Intrastriatal Botulinum Neurotoxin-A Injection in a Unilateral 6-OHDA Rat Model of Parkinson’s Disease. Toxins. 2021; 13(7):505. https://0-doi-org.brum.beds.ac.uk/10.3390/toxins13070505
Chicago/Turabian StyleAntipova, Veronica, Carsten Holzmann, Alexander Hawlitschka, Martin Witt, and Andreas Wree. 2021. "Antidepressant-Like Properties of Intrastriatal Botulinum Neurotoxin-A Injection in a Unilateral 6-OHDA Rat Model of Parkinson’s Disease" Toxins 13, no. 7: 505. https://0-doi-org.brum.beds.ac.uk/10.3390/toxins13070505





