1. Introduction
Hypophosphatasia (HPP, OMIM entry #241500) is a rare genetic disorder, characterized by bone hypomineralization and rickets-like changes in radiological examinations, as well as reduced serum alkaline phosphatase concentrations in blood tests [
1,
2,
3,
4,
5]. HPP has a wide range of onset age and severity, and is usually classified into the following six types: perinatal severe (fetal-neonatal, characterized by respiratory insufficiency and hypercalcemia); perinatal benign (fetal-neonatal, characterized by prenatal skeletal manifestations that slowly resolve into a milder form); infantile (age < 6 months, characterized by rickets and an absence of elevated serum alkaline phosphatase activity); childhood (age ≥6 months to <18 years; characterized by manifestations that range from low bone mineral density for age (with unexplained fractures) to rickets (with premature loss of primary teeth with intact roots); adult (age ≥ 18 years, characterized by stress fractures and pseudofractures of lower extremities in middle age); and odonto (regardless of age, characterized by premature exfoliation of primary teeth without skeletal manifestations) [
1,
2,
3,
4,
5].
Typical dental manifestations of HPP are known to include early exfoliation of primary incisors before 4 years of age [
6,
7,
8]. This manifestation sometimes leads to diagnosis of mild HPP (e.g., odonto and childhood types) [
9,
10]. To the best of our knowledge, there have been few reports regarding long-term follow-up in patients with dental manifestations of HPP after early exfoliation of primary incisors [
11,
12,
13]. Here, we describe a patient with HPP who completed longitudinal follow-up for both posterior and anterior primary teeth. We also describe a new finding in primary teeth and provide our hypothesis regarding the pathogenesis of ankylosis in the teeth of patients with HPP.
2. Case Report
A 14-month-old boy was referred to the Department of Pediatric Dentistry at Osaka University Dental Hospital with the chief complaint of early loss of primary teeth. Intraoral examinations revealed that the primary mandibular bilateral incisors and the primary mandibular left lateral incisor were missing. We previously described a patient with HPP who was diagnosed on the basis of early exfoliation of primary teeth [
9]. The present patient exhibited a low level of serum alkaline phosphatase (192 IU/I); radiological examinations of the lower extremities and hands did not show metaphyseal irregularities indicative of rickets. Tissue-nonspecific alkaline phosphatase gene sequencing demonstrated a heterozygous c.550C > T (p.Arg184Trp) mutation. The patient’s condition was classified as odonto-type HPP, based on the results of these examinations.
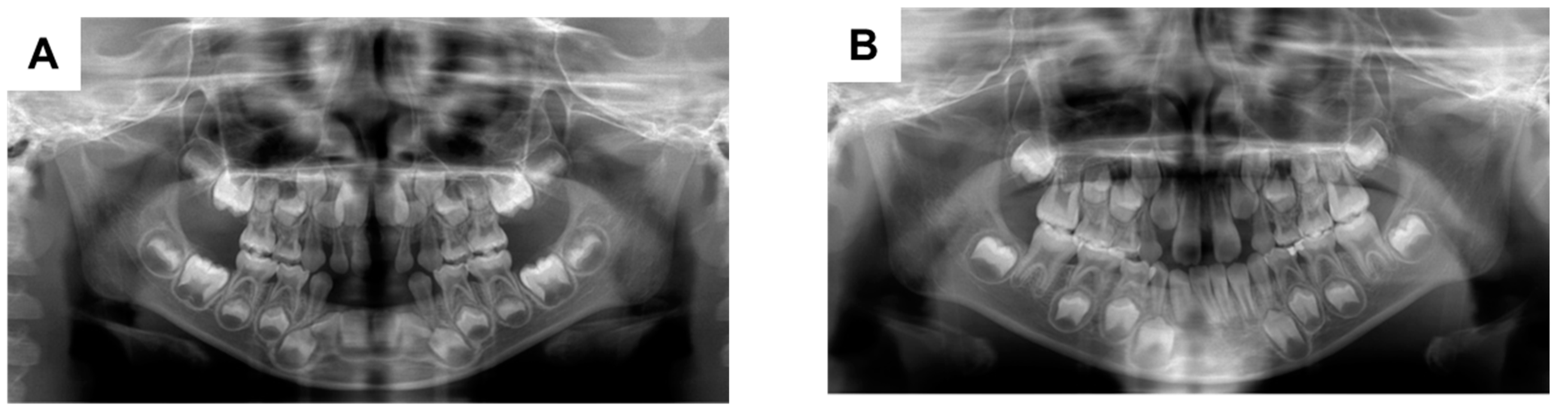
The patient’s primary mandibular right lateral incisor spontaneously exfoliated when he was 2 years and 11 months of age; the primary maxillary left incisor also exfoliated when he was 4 years and 1 month of age. Partial dentures were applied for space maintenance; there were no problems regarding subsequent replacement with the corresponding permanent teeth (
Figure 1A). However, the primary mandibular right first molar was appeared to be submerged when the patient was 8 years and 3 months of age; the severity of submergence was greater when the patient was 9 years of age (
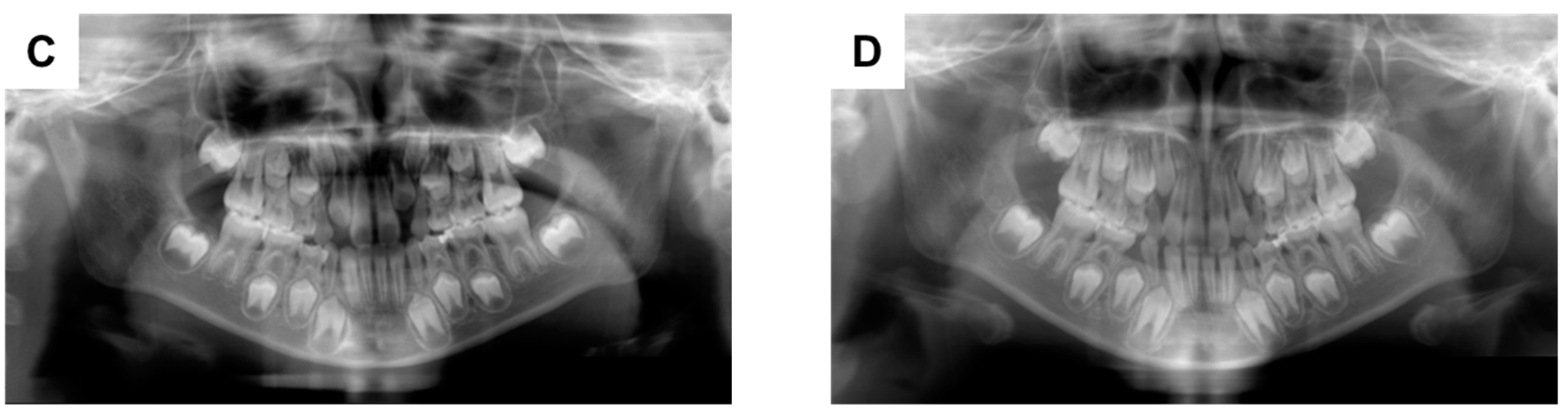
Figure 1B,C). The primary mandibular right first molar was about 1.5 mm submerged from the primary mandibular right second molar, and the periodontal ligament cavity was partially unclear (
Figure 2A,B). The primary mandibular right first molar was considered to be ankylosed, although the corresponding tooth in the opposite quadrant did not show similar findings. Thus, extraction of the affected tooth was performed (
Figure 2C). Histopathological analysis of the tooth showed disturbed cementum formation and acellular cementum, with wide and wavy ivory tubules and aplasia (
Figure 2D). The patient’s postoperative course was good, and no particular complications were observed. The mandibular right mandibular first premolar showed a tendency to erupt (
Figure 1D).
3. Discussion
Early exfoliation of primary teeth is a well-known dental manifestation in patients with HPP [
6,
7,
8,
9,
10]. Early exfoliation is presumably limited to the anterior region because of characteristics such as the time of eruption, tooth morphology, and number of roots involved. The primary incisors erupt first in primary dentition; these influence occlusal force. The primary incisors are also short; each exhibits a single, small root. However, there have been no reports regarding primary molars in patients with HPP who experience early exfoliation of primary incisors.
Here, we described a patient with HPP who completed a longitudinal follow-up period of approximately 10 years. During follow-up, the primary mandibular right first molar was submerged when the patient was 8 years of age; this submergence demonstrated further progression when the patient was 9 years of age. Therefore, the primary mandibular right first molar was considered to be ankylosed. We extracted a lower position of the patient’s primary teeth. Histopathological analysis of extracted tooth revealed disturbed cementum formation. Then, we confirmed the diagnosis as ankylosis. Thus, we presumed that ankylosis had been caused by disturbed cementum formation and altered occlusal force. The poor periodontal condition (due to disturbed cementum formation related to HPP) led to the absence of a root connection with alveolar bone by means of periodontal ligament. The excessive occlusal force gradually damaged this periodontal tissue and subsequently affected root adhesion to alveolar bone.
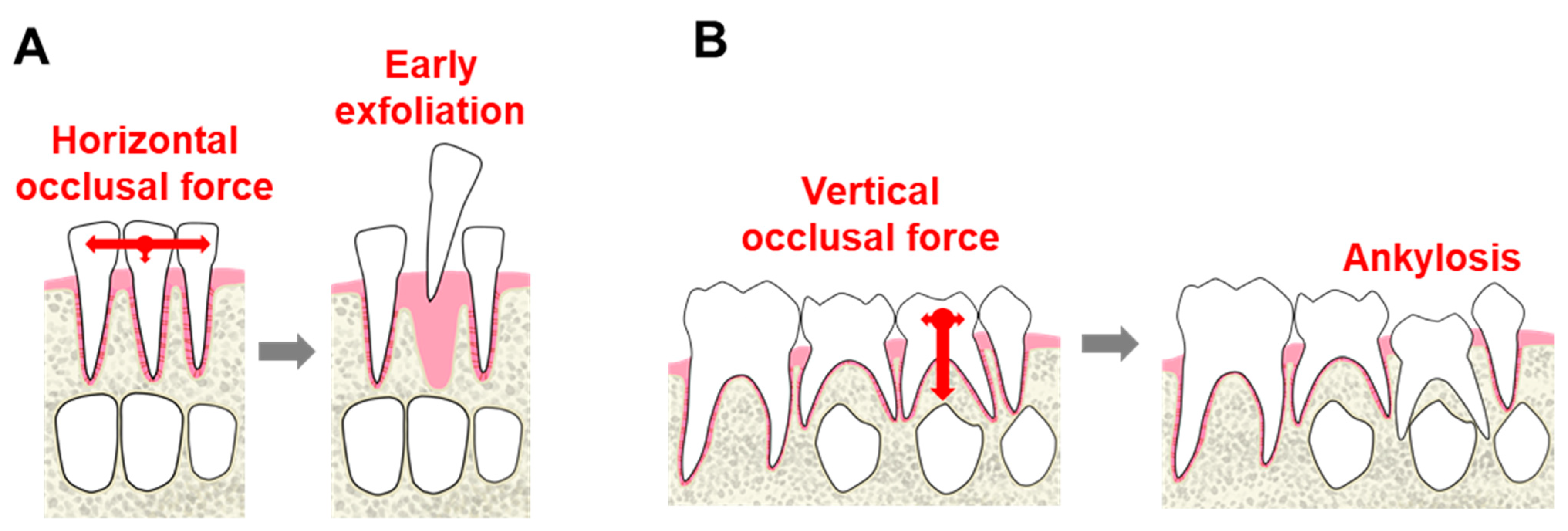
We suspect that the following mechanism contributed to the pathogenesis of ankylosis in this patient. In anterior teeth, lateral occlusal force is stronger than vertical force (
Figure 3A); this lateral force can promote tooth exfoliation. Conversely, occlusal force acts vertically in the posterior region, such that affected teeth may resist exfoliation (
Figure 3B). Therefore, ankylosis may occur in molars, but is less likely to occur in anterior teeth. Although this is the first report of ankylosis in a patient with HPP, the contributing factors are not fully clear and data for additional patients are needed; however, in patients with other severe types of HPP, exfoliation and ankylosis may not occur.
Notably, ankylosis was detected only in the primary mandibular right first molar. The opposite first molar was filled with composite resin due to caries; and the site of restoration was adjusted to reduce occlusion pressure. Alternatively, the partial denture clasp may have exerted excessive vertical force on the primary mandibular right first molar. The reason for local occurrence of ankylosis is unclear; thus, we plan to observe dentition exchange carefully in this patient.
Partial dentures are used for space maintenance in patients with HPP who experience early exfoliation [
6,
9]. In our patient, a mandibular denture was applied at the age of 4 years and a maxillary denture was applied at the age of 5 years; subsequent tooth replacement did not show any problems. We also considered the use of a band loop appliance for space maintenance after extraction of this ankylosed primary first molar; however, we did not apply this appliance because of the high likelihood of early exfoliation involving the mandibular right second molar. The patient’s orthodontist noted that the primary mandibular first and second molars would not move in the mesial direction because the mandibular first molar had fully erupted; distal movement of primary canines was desirable to resolve the patient’s tendency for anterior crossbite.
Tooth movement is more likely to occur in patients with HPP, because they exhibit weaker external force than the general population. Therefore, care is needed when performing an oral surgical procedure (e.g., tooth extraction) in these patients, to avoid application of excessive force to adjacent teeth.
4. Conclusions
Early exfoliation and ankylosis are important considerations in patients with HPP. Disturbed cementum formation in patients with HPP leads to early exfoliation in the anterior region and ankylosis in the posterior region. Ankylosis in molars might be caused by vertical occlusal force acting on periodontal tissue; early exfoliation in incisors might be caused by horizontal occlusal force. Dentists should focus on dentition and occlusion in primary dentition of patients with HPP. However, since HPP is a rare disease, there are many unclear points, and therefore it is necessary to accumulate cases. Total oral management should be performed with consideration of the possibility of ankylosis, as well as attention to premature tooth loss, during dental treatment of patients with HPP.
Author Contributions
Conceptualization, M.H. and R.O.; methodology, R.O.; validation, M.H., R.O. and Y.O.; formal analysis, R.N.; investigation, Y.O.; resources, R.O.; data curation, S.M.; writing—original draft preparation, M.H.; writing—review and editing, K.N.; visualization, S.M.; supervision, N.U.; project administration, K.N. All authors have read and agreed to the published version of the manuscript.
Funding
This research was funded by a grant from JSPS KAKENHI, grant number JP15K11364.
Institutional Review Board Statement
The study was conducted according to the guidelines of the Declaration of Helsinki, and approved by the Ethics Committee of Osaka University of Graduate School of Dentistry (protocol code H29-E15-1 and date of approval 12 September 2017).
Informed Consent Statement
Written informed consent was obtained from the legal guardian of this patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request.
Data Availability Statement
Not applicable.
Conflicts of Interest
The authors hereby confirm that there are no known conflicts of interest associated with this publication and there has been no significant financial support for this work that could have influenced the findings presented.
References
- Whyte, M.P.; Zhang, F.; Wenkert, D.; McAlister, W.H.; Mack, K.E.; Benigno, M.C.; Coburn, S.P.; Wagy, S.; Griffin, D.M.; Ericson, K.L.; et al. Hypophosphatasia: Validation and expansion of the clinical nosology for children from 25 years experience with 173 pediatric patients. Bone 2015, 75, 229–239. [Google Scholar] [CrossRef] [PubMed]
- Whyte, M.P. Hypophosphatasia-aetiology, nosology, pathogenesis, diagnosis and treatment. Nat. Rev. Endocrinol. 2016, 12, 233–246. [Google Scholar] [CrossRef] [PubMed]
- Whyte, M.P.; Wenkert, D.; Zhang, F. Hypophosphatasia: Natural history study of 101 affected children investigated at one research center. Bone 2016, 93, 125–138. [Google Scholar] [CrossRef] [PubMed]
- Mornet, E. Hypophosphatasia. Metabolism 2018, 82, 142–155. [Google Scholar] [CrossRef]
- Michigami, T.; Ohata, Y.; Fujiwara, M.; Mochizuki, H.; Adachi, M.; Kitaoka, T.; Kubota, T.; Sawai, H.; Namba, N.; Hasegawa, K.; et al. Clinical practice guidelines for hypophosphatasia. Clin. Pediatr. Endocrinol. 2020, 29, 9–24. [Google Scholar] [CrossRef]
- Okawa, R.; Nakano, K.; Matsumoto, M.; Kawabata, K.; Ooshima, T. Oral manifestations of patients with hypophosphatasia. Pediatr. Dent. J. 2012, 22, 155–162. [Google Scholar] [CrossRef]
- Bloch-Zupan, A. Hypophosphatasia: Diagnosis and clinical signs—A dental surgeon perspective. Int. J. Paediatr. Dent. 2016, 26, 426–438. [Google Scholar] [CrossRef] [Green Version]
- Okawa, R.; Kokomoto, K.; Kitaoka, T.; Kubota, T.; Watanabe, A.; Taketani, T.; Michigami, T.; Ozono, K.; Nakano, K. Japanese nationwide survey of hypophosphatasia reveals prominent differences in genetic and dental findings between odonto and non-odonto types. PLoS ONE 2019, 14, e0222931. [Google Scholar] [CrossRef]
- Okawa, R.; Kitaoka, T.; Saga, K.; Ozono, K.; Nakano, K. Report of Two Dental Patients Diagnosed with Hypophosphatasia. J. Clin. Case Rep. 2016, 6, 2. [Google Scholar] [CrossRef] [Green Version]
- Okawa, R.; Kadota, T.; Matayoshi, S.; Nakano, K. Dental Manifestations Leading to the Diagnosis of Hypophosphatasia in two children. J. Dent. Child. 2020, 87, 3–7. [Google Scholar]
- Lynch, C.D.; Ziada, H.M.; Buckley, L.A.; O’Sullivan, V.R.; Aherne, T.; Aherne, S. Prosthodontic rehabilitation of hypophosphatasia using dental implants: A review of the literature and two case reports. J. Oral Rehabil. 2009, 36, 462–468. [Google Scholar] [CrossRef] [PubMed]
- Olsson, A.; Matsson, L.; Blomquist, H.K.; Larsson, A.; Sjödin, B. Hypophosphatasia affecting the permanent dentition. J. Oral Pathol. Med. 1996, 25, 343–347. [Google Scholar] [CrossRef] [PubMed]
- Watanabe, H.; Umeda, M.; Seki, T.; Ishikawa, I. Clinical and laboratory studies of severe periodontal disease in an adolescent associated with hypophosphatasia. A case report. J. Periodontol. 1993, 64, 174–180. [Google Scholar] [CrossRef] [PubMed]
| Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).